General practices have a responsibility to ensure their patients can receive timely access to medical care and advice. 1,2 This includes the potential of having a general practitioner (GP) visit patients at their place of residence (if a visit is deemed safe and reasonable to conduct). 1,2 The number of GP home visits has decreased in recent years, 3 with an estimated 690,000 fewer visits nationwide in 2009–10, compared with a decade earlier. 4 The rate of home visits has decreased significantly, 4,5 halving between 1997 and 2007 (from 15.8 to 7.7 visits annually per 100 Australians). 6 In 2009–10, only 0.64% of all GP–patient encounters were home visits, down from 1.75% 11 years earlier. 7
A GP visit to a home or institution (such as an aged care facility) attracts a higher Medicare Benefits Schedule (MBS) payment than a traditional practice-based consultation. A standard practice-based daytime consultation attracts a fee of $37.05, compared with $63 for a standard daytime home visit, and up to $153 for an after-hours home visit. 2 Home visits are generally bulk-billed, meaning there is no cost to the patient. In 2014, over $87 million in Medicare benefits were paid for 1.4 million non-urgent home or institutional visits conducted that year. 3
Two-thirds of GP home visits are to residential aged care facilities, 5 and the majority (60%) are for the treatment of adults aged 65 years and older. 3,6 GP home visits are less likely to be for paediatric patients, with only 4.5% for children aged 4 years and under and 3.7% for children aged 5–14 years. 3 Of all patients who receive a home visit, the overall rate of referral to hospital emergency departments (EDs) is 1.6%. 7
While GP home visits to younger Australians remain uncommon, EDs are experiencing increasingly high numbers of paediatric presentations. 8 The majority are for lower urgency clinical conditions, triaged at the ED as category 4 or 5 on the Australasian Triage Scale. 8 Such presentations typically involve normal respiration and circulation, no haemodynamic compromise, and mild or no pain. 9 More children aged ≤9 years and classified as triage category 4 or 5 present at the ED after hours than during business hours. 10 Young children aged 0–4 years are among the highest ED users for low-urgency conditions during the after-hours period. 10
Of the children who do receive GP home visits, 76% of these visits occur after hours. 3 A decreasing proportion of general practices provide after-hours care on their own or in cooperation with other practices. Nearly half of all general practices (47.4%) rely solely on Medical Deputising Services (MDSs) to provide after-hours care (up from 34.5% a decade ago). 11 Thus, MDSs, rather than general practices, are often the providers of home visits for paediatric patients.
There are accredited MDS companies (sometimes known as ‘locum services’) with employed or contracted GPs operating in most states of Australia. Approximately 85% of the population resides within MDS coverage areas. 12 MDSs provide care in the federally defined after-hours periods of before 8 am and after 6 pm on weekdays, before 8 am and after noon on Saturdays, and all day on Sundays and public holidays. 2 MDSs are permitted to accept bookings two hours before the after-hours period begins. This may have an impact on whether some patients attempt to call their GP during the overlapping period when practices are still open and when the MDSs have started to accept bookings. MDSs are required to provide a report to the patient’s regular GP on any home-visit recipient. 12
Federal funding provides incentives and grants to encourage practices and MDS companies to offer after-hours and home‑visiting services. 12,13 Despite significant government funding to support and publicise home-visiting GP services, there is very little Australian research on their use, particularly for paediatric patients. This study examined whether parents or guardians of children presenting to a hospital ED for lower urgency conditions contacted a home visiting GP service prior to ED presentation.
Methods
Data collection
This survey was conducted as part of a larger study investigating factors associated with paediatric use of EDs for lower urgency conditions. The questions that are relevant to the use of home‑visiting GP services are supplied in Figure 1. Parents or guardians of children aged ≤9 years presenting with lower urgency conditions (triage category 4 or 5) to the EDs of three public general hospitals and one paediatric specialty hospital in metropolitan Melbourne were approached by trained research assistants. The hospitals were located within geographic areas with MDS coverage. Parents or guardians who were in obvious distress or had limited English proficiency were not approached. Participants gave informed consent before being left for approximately 10 minutes to complete an electronic survey (on an iPad) while waiting for their child to be seen.
Participants were recruited across three time periods on weekdays (8.00 am to 4:59 pm, 5.00 pm to 9:59 pm and 10:00 pm to 7:59 am) and on weekends (5.00 pm Friday night to 7:59 am Monday morning). Participants received a $10 supermarket gift voucher as reimbursement for their time.
Data collection was conducted between May and November 2014. Data were collected and managed using Research Electronic Data Capture (REDCap) tools hosted at the University of Melbourne. 14 The study received ethics approval from the University of Melbourne Human Research Ethics Committee and from the ethics committees at each of the four participating hospitals (reference: 1341293.1/34070A).
Data analysis
The responses were analysed relative to any contact with home-visiting GP services prior to ED presentation. Statistical analyses were performed using STATA 13.0 (StataCorp College Station, TX). Frequency and descriptive analyses were initially undertaken to examine the data. Subsequently, bivariate analyses using chi-square statistics were conducted to determine the differences (if any) among respondents on the basis of the hospital of presentation or demographic variables. The variables included birth order of the child brought to the ED (first born versus all other), age of the primary carer (≤30 versus >30 years), household income (≤$100,000 versus >$100,000) and the time band of presentation to the ED.
Results
Electronic surveys were completed by 1150 parents or guardians of children aged ≤9 years and triaged as category 4 and 5. Approximately 19.9% who were considered eligible and were approached by a research assistant declined to participate. There were roughly equal numbers of participants recruited across the four hospitals. Demographic data are presented in Table 1.
Table 1. Demographic characteristics of participants
|
| Demographic characteristic | | % (n) |
|---|
| Time band of ED presentation (n = 1150) |
|
|
|
Day (8:00 am – 4:59 pm) |
27 (309) |
|
Evening (5.00 pm – 9:59 pm) |
27 (308) |
|
Night (10.00 pm – 7:59 am) |
17 (198) |
|
Weekend |
29 (335) |
| Age of child (n = 1143) |
|
|
|
<1 years |
23 (258) |
|
1–4 years |
51 (583) |
|
5–9 years |
26 (302) |
| Household composition (n = 1122) |
|
|
|
Single parent |
14 (162) |
|
Dual parent |
82 (917) |
|
Other |
4 (43) |
| Household income (n = 1095) |
|
|
|
$0–25,000 |
13 (137) |
|
$25,001–50,000 |
16 (173) |
|
$50,001–80,000 |
23 (251) |
|
$80,001–100,000 |
17 (184) |
|
>$100,000 |
32 (350) |
| Age of child’s primary carer (n = 1129) |
|
|
|
<20 |
4 (48) |
|
21–30 |
27 (306) |
|
31–40 |
52 (590) |
|
>40 |
16 (185) |
| Chief complaint (n = 1116) |
|
|
|
Injury |
34 (373) |
|
Illness |
66 (743) |
| Birth order (n = 1129) |
|
|
|
First born |
53 (602) |
|
All other |
47 (527) |
| Private health insurance status of child (n = 1130) |
|
|
|
Covered |
41 (460) |
|
Not covered |
59 (670) |
| Education of primary carer (n = 1124) |
|
|
|
Secondary school or less |
20 (226) |
|
Trade or other certificate level |
20 (226) |
|
Undergraduate diploma |
13 (141) |
|
Bachelor’s degree |
28 (316) |
|
Postgraduate qualification |
19 (215) |
| Citizenship status of primary carer (n = 1122) |
|
|
|
Australian citizen (by birth) |
68 (765) |
|
Australian citizen (by oath) |
17 (192) |
|
Permanent resident |
13 (142) |
|
Temporary resident |
2 (21) |
|
Tourist |
0 (2) |
Rare item non-response to individual demographic questions means that the number of respondents for each question may differ slightly. Percentages are rounded and
may not sum to 100%. |
Contacting home visiting GP services
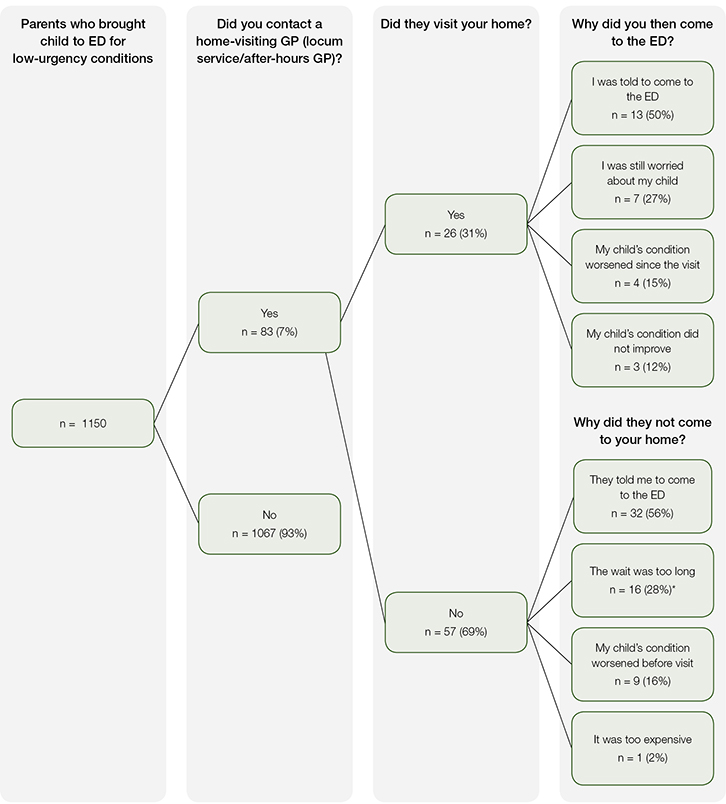
Few participants (n = 83; 7%) reported having contacted a home-visiting GP service prior to bringing their child to the ED. There were no significant differences relative to time of day of presentation, hospital of presentation or demographic variables (see Figure 1 for full results).
 |
|
*Response more common among parents of first-born children (P = 0.02). No other significant differences were found relative to time of day of ED presentation, hospital of presentation, or demographic variables. Percentages are rounded and may not sum to 100%.
Figure 1. Use of home-visiting GP services prior to ED presentation for children aged ≤9 years with lower urgency conditions (triage category 4 or 5)
|
Receiving a home visit
Of the 83 participants who contacted a home-visiting GP service, only 26 (31%) received a visit from the GP. When asked why they subsequently attended the ED, 13 (50%) reported being told to do so by the visiting GP, while 7 (27%) reported being still worried about their child.
Reasons for not receiving a home visit
Of the 57 parents who contacted a home visiting GP but did not receive a visit, more than half (n = 32; 56%) reported being told to go to the ED by the service. A further 16 participants (28%) reported not having the visit because the projected wait time was too long. This response was more common among parents of first-born children ( P = 0.02). No significant differences were found when the results were stratified by the other demographic variables.
Discussion
Among the most important findings from our study was that only 7% of participants had contacted a home-visiting GP service prior to presenting at the ED with a child with a lower urgency condition. It is important for future research to explore what proportion of parents are aware of the existence of home-visiting GP services, and understand when and how they can be contacted. Recent research in the same geographical area found that although some general practices displayed information about home-visiting GP services in patient waiting areas, this was not always prominent. 15
It is also possible that parents knew about the home-visiting GP services but chose not to contact them. In a study in the same area, 440 adults were asked what actions they would take if they were sick after hours. The most common response was to go to the ED (39%). A further 23% would wait until the following day to seek care, and only 9% would contact a home-visiting GP or locum service. 16 A similar study of 281 adults in New South Wales also found a strong preference to use the ED for after-hours care (60%) rather than a home-visiting GP service (18%). 17
Another key finding of our study was that half of the parents of children who received a home visit reported being told to take their child to the ED. Additionally, more than half of those who contacted a home-visiting service but did not receive a visit reported that they were referred directly to the ED by the service.
The reasons behind referral to the ED are unknown and should be the focus of future investigations. It is possible that the call centres and GPs attending to these children may have less confidence in their ability to provide paediatric, rather than adult, care. Children make up a relatively small, and decreasing, proportion of all GP consultations, 18,19 and most home visits are to older adults. 3,6,7 The level of experience of home-visiting GPs in treating paediatric patients is unknown. Additionally, over one quarter of those who did receive a GP home visit came to the ED because they were still worried about their child’s condition. Future research will need to explore parents’ levels of confidence in the advice or treatment provided.
Over one quarter of parents or guardians who contacted a service but did not receive a visit believed that the projected wait time was too long. This view was more common among parents attending the ED with their first-born child. It is unknown whether parents of first-borns are willing to accept the same length wait as parents of second-born or subsequent children. While we did not collect data on what length of time our respondents deemed excessive, most home-visiting GP services promote their ability to have a doctor attend the home within a maximum of a few hours. 20 Parents may not be aware that a low-urgency patient presenting to an ED may also end up waiting several hours for treatment. 21,22
Non-urgent home visits cost Medicare $87 million 3 per year and attract significant federal funding though incentives and grants. 12,13 However, home visits are not necessarily an efficient use of GPs’ time. In the time it takes to drive and visit one patient at home, the GP could potentially have seen multiple patients at their practice. 23 Further, there are limitations on what can be achieved during a home visit. The GP does not have access to the patient’s history and notes, nor is there medical equipment available during a home visit. Many Australian GPs feel that these issues present challenges to providing safe and effective patient care in the context of a home visit. 23
This study has some limitations. The research questionnaire was administered only in English. This may limit generalisability to the wider Australian population, as awareness and use of primary care services may differ according to English proficiency. Further, the study was conducted in four hospitals in metropolitan Melbourne. Access to primary healthcare services and MDS coverage can vary greatly between regions. It is known that the use of after-hours GP services for adults in the areas included in this study is similar to other comparable metropolitan areas in Australia. 24,25 It cannot be determined what proportion of children contacting or seen by a home-visiting GP do not subsequently present to an ED.
Conclusion
Very few parents of children presenting to the ED with lower urgency conditions had contacted a home visiting GP service. Of those presenting to the ED who received a GP home visit, half were referred to the ED. Among those who contacted a service but did not actually receive a visit, over half reported being referred to the ED when they rang. Referral of children to the ED by home-visiting services warrants further investigation to determine the appropriateness of care these services are able to provide to children.
Authors
Amy R Allen BBNSc, BPsySci (Hons), GradDipAoD, Research Assistant, Centre for Health Policy, Melbourne School of Population and Global Health, University of Melbourne, Parkville, VIC
Erin Turbitt PhD, Research Fellow, Centre for Health Policy, Melbourne School of Population and Global Health, University of Melbourne, Parkville, VIC
Gary L Freed MD, MPH, Director, Health Systems and Workforce Unit, Centre for Health Policy, Melbourne School of Population and Global Health, University of Melbourne, Parkville, VIC. gary.freed@unimelb.edu.au
Competing interests: None.
Provenance and peer review: Not commissioned, externally peer reviewed.
References