In this article, we aim to provide a strong rationale for why the assessment of walking (gait) speed of older adults should be an integral component of general practice. We suggest that by regularly assessing gait speed and using evidence-based approaches to improve gait and reduce the risk of falls,1,2 general practitioners (GPs) will be able to substantially improve patients’ physical performance outcomes, ease care burden and reduce healthcare costs.
Walking is a key physical performance task for people of all ages, including older adults. The majority of older Australians have decreased physical activity, leading to poor physical function such as reduced gait speed, strength and balance.3 Specifically, individuals with slower gait speeds are at a higher risk of disability, cognitive impairment, institutionalisation, falls and mortality.4 A meta-analysis has found that older individuals in the lowest quartile of gait speed had a threefold increased risk of mortality when compared with individuals in the highest quartile.4
Preferred (habitual) gait speed is a simple, quick and easily obtained clinical measure5 that has commonly been used by geriatricians for decades. Gait speed also has similar predictive ability as larger geriatric composite tools such as the Short Physical Performance Battery or the Timed Up and Go tests.3,4 Gait speed is generally assessed using a stopwatch to time how long it takes an individual to walk a set distance. The distance is usually 2.4–8 m, with 4 m being the most commonly used.4 All gait speed tests should be performed at the patients’ usual walking speed and with their regular gait aid, if required. The tester should be positioned in line with the finish line, and initiate and stop timing when the patients’ closest hip or foot passes the respective lines. Patients could perform two to three trials during their GP consultation in approximately two minutes. On the basis of the established population gait speed data, the GP could categorise the individual and provide appropriate management (Figure 1).
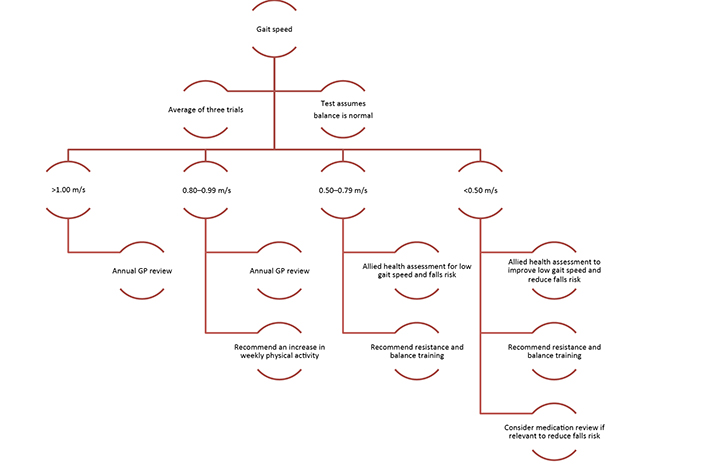 |
| Figure 1. Walking speed flowchart |
More sophisticated pressure mat systems (eg GAITRite and Gait Matt II) that assess other spatio-temporal variables, including step length, step rate and ground contact time, may also be used in larger general practice clinics or residential aged care facilities (RACFs). These systems provide additional clinically relevant information, including a prediction of falls risk.6 They may best be operated by physiotherapists, accredited exercise physiologists, practice nurses or medical students. The timing and location of a patient’s footprint is quantified via the embedded pressure sensors in the mat. These data can be viewed on a laptop screen, and are automatically calculated and saved in a database.
While a variety of gait speed thresholds exist, healthy community-dwelling older adults tend to experience poorer health if they walk <0.8 m/s,4,7 whereas for frail older adults aged >80 years, a more realistic threshold might be <0.5 m/s.8 For patients identified as having a habitual gait speed below the relevant thresholds,4,7,8 or for those experiencing a decline greater than the maximum expected decline of 0.05 m/s per year,9 we recommend that GPs perform further tests to identify reasons for their poor gait speed. This is important as reduced gait speed could reflect a serious acute illness, worsening of an existing medical condition or the development of a new chronic condition.4
As previously mentioned, reduced gait speed is an indication of an increased risk of falls.7 The reduced gait speed may also be a marker of reduced overall physical function, suggesting the patient may benefit from progressive resistance and balance training. These exercise forms can substantially improve muscular strength, endurance and balance. They can produce clinically significant improvements in gait speed, including increases of 0.04–0.12 m/s in RACF residents after only 10–13 weeks of training, ultimately resulting in reduced risk of falls.1 Physiotherapists and accredited exercise physiologists are ideally placed to deliver these exercise classes to older adults.
In conclusion, we strongly encourage GPs to routinely assess their older patients’ gait speed (at least on an annual basis) and develop referral pathways to provide evidence-based interventions for patients with low and/or declining gait speed. For GPs working closely with retirement villages or RACFs, we would encourage them to meet with the facility providers and managers to make a case for why monitoring a resident’s gait speed is important. The GP may also assist facilities to develop pathways whereby those identified with poor gait speed can access appropriate interventions. Regular monitoring of gait speed and intervening (where appropriate) will produce clinically relevant and measurable positive changes to many older adults that will transfer to improved outcomes for the patient and a reduction in healthcare expenditure.10
Authors
Samantha Fien BExSci, PhD candidate, Faculty of Health Science and Medicine, Bond University, Robina, QLD. samantha.fien@student.bond.edu.au
Timothy Henwood PhD, Principal, AgeFIT Solution, Honorary Senior Research Fellow, School of Human Movement & Nutrition Sciences, University of Queensland; and Faculty of Health Science and Medicine, Bond University, Robina, QLD
Mike Climstein PhD, FACSM, FASMF, FAAESS, Adjunct Associate Professor, Exercise, Health and Performance Faculty Research Group, University of Sydney, Sydney, NSW
Justin William Leslie Keogh PhD, Associate Professor, Faculty of Health Science and Medicine, Bond University, Robina, QLD; Human Potential Centre, AUT University, Auckland, NZ; Cluster for Health Improvement, Faculty of Science, Health, Education and Engineering, University of the Sunshine Coast, Sippy Downs, QLD
Competing interests: None.
Provenance and peer review: Not commissioned, externally peer reviewed.