Case study
A boy, six years of age, presented with painful swelling of his left ear, cheeks and left hand. He had a past history of eight presentations to general practitioners (GPs) or the local emergency department from the age of two to six years with the diagnosis of either impetigo or cellulitis. There was no history of trauma or medication use precipitating the episodes. On three occasions, either vesicles or bullae were seen on examination. He had been treated with oral antibiotics at each presentation.
The lesions would typically worsen then resolve. Swabs of the lesions for microscopy, culture and sensitivity (MC&S) were taken on four occasions and no bacteria had been cultured. A swab for Varicella zoster virus and Herpes simplex virus polymerase chain reaction (PCR) on vesicle fluid had been negative. Blood samples taken during one episode showed:
- White cell count = Normal
- Eosinophils = 1.8 x 109/L (normal 0.1–0.8 x 109/L)
- C-reactive protein (CRP) = Normal
- Immunoglobulin E (IgE) = >2000 KIU/L (normal <12 KIU/L)
The boy had been seen by a dermatologist, who considered bullous insect bite reaction.
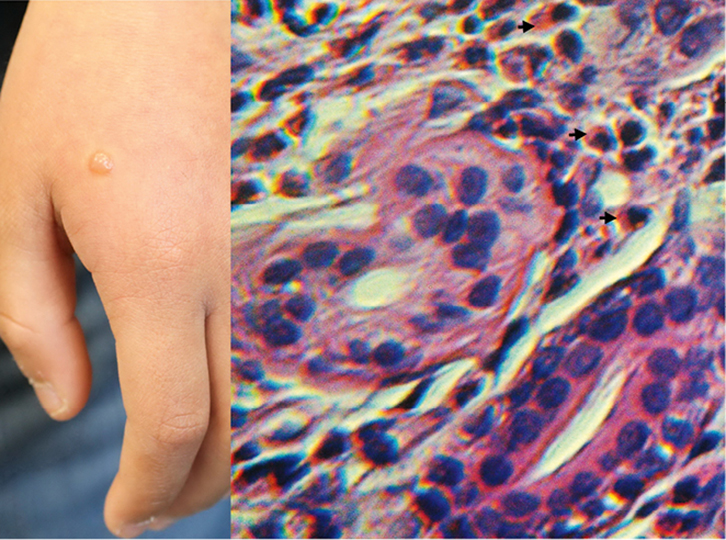
On examination, the boy had a swollen, red, tender left ear, red plaques on his cheeks with golden-coloured crust, and red swelling of the dorsum of his left hand with an overlying bulla (Figures 1, 2). His oral temperature was 37.3°C.
 |
 |
| Figure 1. Cheek plaques and swollen ear |
Figure 2. Hand bulla with histopathology illustrating eosinophils |
Question 1
What differential diagnoses should be considered?
Question 2
What investigations would be helpful in making a diagnosis?
Answer 1
The differential diagnoses include bacterial cellulitis as there is moderate erythema and oedema. Bacterial cellulitis usually presents as a red, swollen, tender plaque with a border that is not sharply demarcated. The boy has multiple plaques, which reduces the likelihood of bacterial cellulitis. The plaques on the boy are not distributed symmetrically or widely, as usually occurs in morbilliform drug reactions, and lack the distinct distribution of allergic contact dermatitis.
The presence of the eruption on the face, ear and dorsum of the hand could be suggestive of polymorphic light eruption, photoallergic drug reaction and phototoxic drug reaction. Recurrent episodes with no bacteria cultured on swabs, elevated serum eosinophils and IgE level raises the suspicion of eosinophilic cellulitis.
Answer 2
Biopsy of the affected skin would be helpful in making a diagnosis. Bacterial swabs should be repeated.
Case continued
A swab of the skin from the left ear did not show leucocytes on Gram stain and no bacteria were cultured. Punch biopsy of the bulla on the hand showed superficial and deep perivascular dermatitis rich in eosinophils (Figure 2). No flame figures were seen. The history of recurrent episodes and the histopathology of dermatitis with abundant eosinophils supports the diagnosis of eosinophilic cellulitis.
Question 3
What is eosinophilic cellulitis?
Answer 3
Eosinophilic cellulitis is a rare condition first described in 1971 as recurrent granulomatous dermatitis with eosinophilia.1 Clinically, it presents as a tender, pruritic, oedematous, cellulitis-like eruption.2 Eosinophilic cellulitis resembles bacterial cellulitis because patients usually present with a warm, erythematous skin lesion.3 Given the similarity in the presentation of the two conditions, eosinophilic cellulits is often misdiagnosed as bacterial cellulitis.4 A lack of response to antibiotic treatment should lead the physician to consider the diagnosis of eosinophilic cellulitis.3
Lesions heal with slight hyperpigmentation resembling morphea.3 Recurrence is common.3 The aetiology is largely unknown but is thought to be a hypersensitivity reaction from a variety of stimuli.4 Insect bites may precipitate some cases.5 Cases have been associated with non-Hodgkin’s lymphoma6 and drug ingestion.7
The histopathological features of eosinophilic cellulitis are dynamic, starting with dermal oedema and infiltration of eosinophils, development of ‘flame figures’, and finishing with the appearance of phagocytic histiocytes.7 Flame figures are collagen bundles in the dermis surrounded by debris from eosinophils.1
Question 4
How would you manage this condition?
Answer 4
The most effective treatment for eosinophilic cellulitis is oral prednisolone.3 Topical corticosteroids have demonstrated efficacy and should be considered in cases of limited disease or for residual lesions.3 Antihistamines can be administered to relieve itching, but they are ineffective in clearing cutaneous lesions.3 In cases of eosinophilic cellulitis with an underlying cause, treating the underlying condition has led to resolution of the syndrome.3
Key points
- Cellulitis with an atypical presentation or that is not responding to antibiotic treatment should trigger the suspicion of eosinophilic cellulitis.3
- The diagnosis of eosinophilic cellulitis should be based on the typical clinical picture and course of the disease with its recurrences, and histopathology.8
Author
Darryn Rennie MBBS, FRACGP, DipACSCM, General Practitioner, Dalyellup Family Medical Centre, and Clinical Senior Lecturer School of Primary, Aboriginal and Rural Health Care, University of Western Australia, Dalyellup, WA. drennie@westnet.com.au
Competing interests: None.
Provenance and peer review: Not commissioned, externally peer reviewed.