Case study
A previously well Caucasian woman, 59 years of age, presented with a single lesion on her vulva that was noted to be slowly enlarging over several months. The patient was not on any regular medication, had no sexual history of unprotected sex and no family history of similar dermatological conditions.
Physical examination of the vulva revealed a well-delineated, 2 x 1.5 cm whitish-pink verrucous plaque, with a papillomatous and velvety surface of soft consistency and without infiltration (Figure 1).
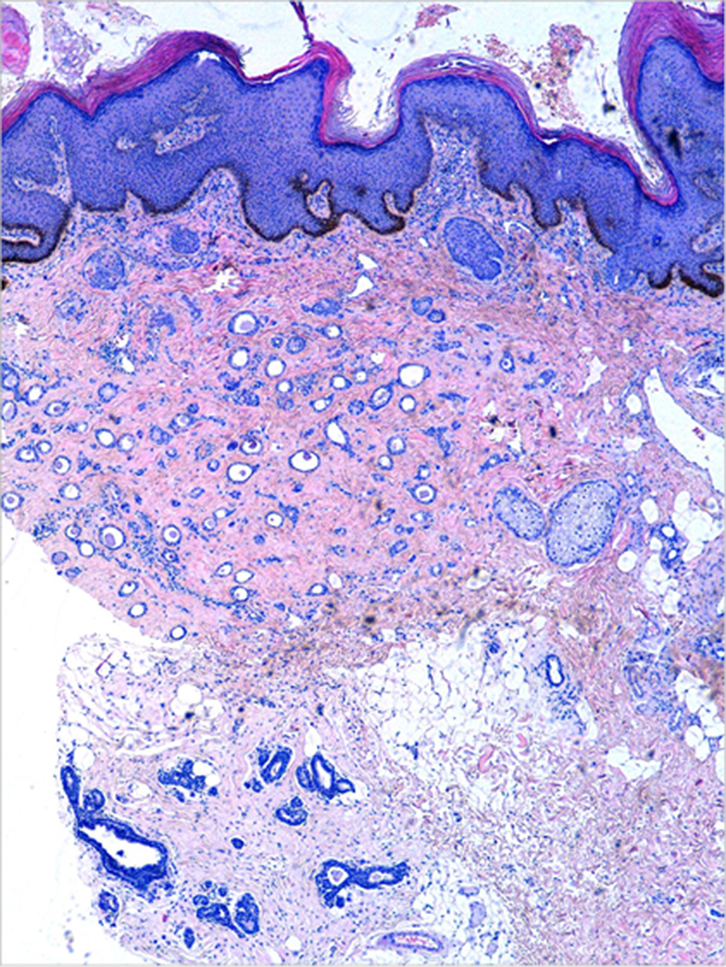
Full blood count and standard biochemistry tests were normal. An initial diagnosis of condyloma acuminatum (anogenital wart) was suspected given the typical clinical presentation. However, there was no response to podophyllotoxin treatment. A skin punch biopsy was performed and confirmed a histological diagnosis of syringoma (Figure 2). No specific treatment was prescribed and the patient continued periodic clinical review.
 |
 |
| Figure 1. Whitish-pink plaque with a papillomatous surface on the vulva |
Figure 2. Ductal epithelial estructures, some of which appeared as tadpole, embedded in fibrous stroma (haematoxylin and eosin x10) |
Question 1
What are vulval syringomas?
Question 2
What are the clinical signs and symptoms?
Question 3
What are the main differential diagnoses?
Question 4
What is the most appropriate management?
Answer 1
Syringoma is a benign adnexal neoplasm, of apocrine or eccrine origin, with mainly ductal differentiation. Syringomas can appear on any site of the skin surface, although they more frequently involve the periorbital area, particularly the eyelids. Vulval syringomas are an under-diagnosed cutaneous condition in clinical practice as most cases do not present with symptoms and may go unnoticed.1 Vulval syringomas tend to present during puberty and are more frequent between the third and fourth decade of life.1 However, they can appear at any age, and rare cases have been described in children and the elderly.
Answer 2
Vulval syringomas tend to be asymptomatic lesions that can sometimes present with intense pruritus, affecting the patient’s quality of life. The severity of pruritus and size of the syringomas may increase in situations such as menstruation and pregnancy.1 There seems to be a possible hormonal influence, although no clear relationship has been established.1 The severity of pruritus may also increase in situations involving higher body temperatures, caused by the postganglionic cholinergic sympathetic nerve stimulation of the eccrine glands.1–5
Vulval syringomas may exclusively affect the genital area, or they may be associated with other concurrent syringomas in extragenital sites, mainly the periorbital area. Three different clinical forms of presentation in the vulva have been described:1–5
- multiple bilateral and symmetrical small-sized papules (between 1 and 5 mm in diameter), skin tone or brown in colour
- myeloid variant with cyst-like, whitish or yellowish bilateral and symmetrical papules
- bilateral and symmetrical lichenoid plaques, similar in appearance to lichen simplex chronicus.
Answer 3
Clinical diagnosis of vulval syringomas is usually difficult because of the non-specific appearance of the lesions. When dealing with vulval papules or plaques, several differential diagnoses should be considered:
- epidermal cysts
- milia
- idiopathic vulvar calcinosis
- steatocystoma multiplex
- condylomata acuminate (anogenital wart)
- lymphangioma circumscripta
- Fox-Fordyce disease
- angiokeratomas
- soft fibromas
- desmoplastic trichoepithelioma
- eccrine epithelioma
- lichen planus
- lichen simplex chronicus.
Hence, biopsy and histological examination are mandatory to confirm the definitive diagnosis. Vulval syringoma must be considered in the differential diagnosis of chronic vulval pruritus.1–5
Answer 4
Given the benign nature of vulval syringomas, no treatment is necessary; however, treatment may be provided for symptomatic cases, or for aesthetic reasons. There is no standardised optimal treatment. Pruritus does not usually respond to topical corticosteroids or oral antihistamines. There are multiple therapeutic options for eliminating vulval syringomas, all of them with variable outcomes and a high relapse rate:6–9
- topical atropine
- curettage
- cryotherapy
- electrosurgery
- dermoabrasion
- topical trichloroacetic acid
- surgical removal.
The best therapeutic option described to date is ablation with carbon dioxide laser, which reduces the pruritus and resolves the lesions effectively and safely, but with a relapse rate of up to 60%.7
Key points
- Vulval syringomas have variable clinical presentations.
- They should be suspected if a verrucous or papillomatous plaque does not respond to standard treatments for condyloma acuminatum (anogenital wart).
- Skin biopsy and histological study is necessary to confirm the diagnosis.
- No treatment is necessary, but it may be performed in symptomatic cases or for cosmetic reasons.
- Therapeutic options have variable outcomes and a high relapse rate.
Authors
Adrián Imbernón-Moya MD, Dermatologist, Department of Dermatology, Hospital Universitario Severo Ochoa, Leganés (Madrid), Spain. adrian_imber88@hotmail.com
Elena Vargas-Laguna MD, Dermatologist, Department of Dermatology, Hospital Universitario Severo Ochoa, Leganés (Madrid), Spain
Alejandro Lobato-Berezo MD, Dermatologist, Department of Dermatology, Hospital Universitario Severo Ochoa, Leganés (Madrid), Spain
Marcela Martínez-Pérez MD, Dermatologist, Department of Dermatology, Hospital Universitario Severo Ochoa, Leganés (Madrid), Spain
Micaela Churruca-Grijelmo MD, Dermatologist, Department of Dermatology, Hospital Universitario Severo Ochoa, Leganés (Madrid), Spain
Antonio Aguilar-Martínez MD, Dermatologist, Department of Dermatology, Hospital Universitario Severo Ochoa, Leganés (Madrid), Spain
Eva Fernández-Cogolludo MD, Dermatologist, Department of Dermatology, Hospital Universitario Severo Ochoa, Leganés (Madrid), Spain
Miguel Ángel Gallego-Valdés MD, Head, Department of Dermatology, Hospital Universitario Severo Ochoa, Leganés (Madrid), Spain
Competing interests: None
Provenance and peer review: Not commissioned, externally peer reviewed.
Acknowledgements
We thank José Luis Agud and Fernando Burgos for their reviews and editing of the manuscript.