Men’s health is often described in terms of male-specific (sexual and reproductive health) problems, but it is their broader health behaviours and use of health services that contribute to their overall health. Australian men have a shorter life expectancy than women,1 and seven of the 10 most common risk factors that contribute to burden of disease are more common in men than women.2 These differences are driven by a combination of gender and biological influences.3
Men see general practitioners (GPs) less frequently than women.4 A report describing GP consultations with male patients using Bettering the Evaluation and Care of Health (BEACH) data from 1999–2000 found that patterns of attendance and health problems managed differed across age groups. Younger men (aged <40 years) were less likely than women to visit a GP, and when they did attend, they tended to have acute illnesses, injuries and psychological problems managed. In middle age (40−64 years) chronic conditions began to emerge, particularly musculoskeletal morbidities. For older men (≥65 years), chronic conditions were predominant.5
In this study, we investigated men’s use of GP services by age (compared with women) to see whether patterns identified in the previous study on their use of GP services and the types of problems managed in different age groups have changed.
Method
We analysed GP–patient encounters with male patients from data collected in the BEACH program from April 2014 to March 2015. The methods of the BEACH program and supplementary analysis of nominated data (SAND) sub-studies are described in detail elsewhere.6 Encounters with men aged 15–44 years, 45–64 years and 65 years or older were compared. Data about patients’ regular general practice were gathered from June to September 2013 from a SAND sub-study.7 The average use of GP services in the population was calculated using Medicare claims data (supplied by Australian Government Department of Health) and Australian Bureau of Statistics (ABS) population data.8
Results
Use of GP services
In 2013–14, males in the Australian population were less likely to see a GP at least once (80% of males in the population) than females (88%; Figure 1). Males also had a lower average annual number of GP consultations per head of population (4.6) than females (6.1; Figure 2). While attendance patterns were similar for male and female children, there were differences in the older age groups, particularly in the 15–44 year age group, where only 71% of men attended at least once (Figure 1) and visited an average 3.1 times per head of population that year (Figure 2).
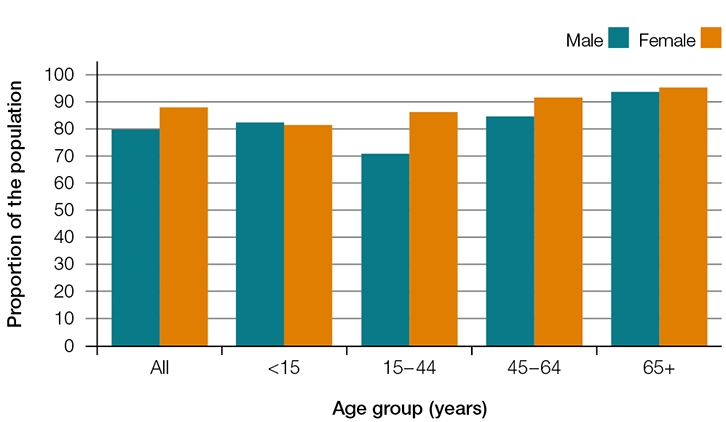 |
| Figure 1. Proportion of the population who saw a GP at least once by sex and age groups, 2013–14 |
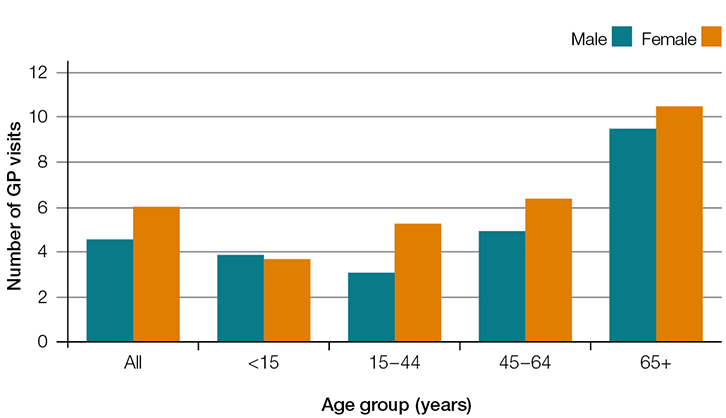 |
| Figure 2. Average number of GP visits per head of population by sex and age groups, 2013–14 |
Regular general practice
Of the 7799 patients sampled in the SAND sub-study, 94.8% of all males and 96.8% of all females had a general practice they considered their regular practice. Men aged 15–44 years were significantly less likely to have a regular practice (87.3%; 95% confidence interval [CI]: 84.4–90.3) than women of the same age (94.3%; 95% CI: 92.9–95.7). For all other age groups, there was no difference in the proportion of males and females who had a regular practice.
Encounters with male patients
In 2014–15, 42.9% of all encounters were with male patients. Compared with those in older age groups (5.2% aged 45–64 years and 2.3% aged 65+ years), male patients aged 15–44 years were significantly more likely to be new to the practice (12.2%). These young men had high rates of new problems managed at encounters (64.9 per 100 encounters) and this decreased significantly in each subsequent age group. By contrast, the number of problems and chronic problems managed per encounter increased with age. The distribution of problems managed by body system is shown in Table 1.
Table 1. Encounters with male patients aged 15–44 years, 45–64 years and 65+ years, 2014–15
|
| |
15–44 years
(n = 10,958) |
45–64 years
(n = 11,629) |
65+ years
(n = 13,195) |
New to practice, per cent of patients
(95% CI) |
12.2
(11.1–13.2) |
5.2
(4.4–5.9) |
2.3
(1.9–2.7) |
Problems managed, rate per 100 encounters
(95% CI) |
135.3
(132.8–137.8) |
160.2
(157.4–162.9) |
175.1
(171.9–178.3) |
New problems, rate per 100 encounters
(95% CI) |
64.9
(62.6–67.2) |
54.0
(52.0–56.1) |
47.9
(46.1–49.8) |
Chronic problems, rate per 100 encounters
(95% CI) |
35.8
(34.0–37.6) |
69.3
(66.7–71.8) |
87.8
(84.4–91.2) |
| Type of problem managed*, per cent of problems managed (95% CI) |
| Respiratory |
15.1
(14.1–16.1) |
9.0
(8.4–9.6) |
8.3
(7.8–8.8) |
| Psychological |
14.8
(13.5–16.1) |
9.9
(9.2–10.6) |
4.9
(4.5–5.3) |
| Musculoskeletal |
14.2
(13.4–15.0) |
14.0
(13.3–14.7) |
10.9
(10.3–11.4) |
| General & unspecified |
13.1
(12.3–13.9) |
12.4
(11.6–13.2) |
11.9
(11.1–12.7) |
| Skin |
13.1
(12.4–13.8) |
10.7
(10.0–11.4) |
12.0
(11.3–12.6) |
| Digestive |
8.9
(8.3–9.5) |
7.8
(7.4–8.3) |
6.9
(6.5–7.3) |
| Endocrine & metabolic |
5.4
(4.9–6.0) |
11.7
(11.0–12.3) |
10.8
(10.2–11.4) |
| Circulatory |
3.9
(3.5–4.3) |
12.7
(12.1–13.4) |
20.2
(19.5–21.0) |
| Neurological |
2.7
(2.4–3.0) |
2.7
(2.4–3.0) |
2.4
(2.2–2.7) |
| Ear |
2.4
(2.1–2.7) |
1.9
(1.7–2.2) |
2.0
(1.8–2.2) |
| Male genital system |
2.4
(2.1–2.7) |
2.9
(2.6–3.3) |
3.3
(3.1–3.6) |
| Eye |
1.4
(1.1–1.6) |
1.2
(1.0–1.4) |
1.8
(1.6–1.9) |
| Urology |
1.1
(0.9–1.3) |
1.5
(1.3–1.7) |
2.7
(2.4–2.9) |
| Blood |
0.8
(0.6–1.0) |
0.9
(0.7–1.2) |
1.6
(1.3–1.9) |
| Social |
0.6
(0.4–0.8) |
0.6
(0.4–0.7) |
0.3
(0.2–0.4) |
| *Types of problems are classified according to the International Classification of Primary Care, version 2 (ICPC-2) |
Overall, respiratory, psychological and musculoskeletal problems were more commonly managed in young men, whereas circulatory and endocrine/metabolic problems were more common among older men.
Respiratory problems (in particular upper respiratory tract infection [URTI], asthma and acute bronchitis) were the most common types of problem managed in men aged 15–44 years (15.1% of problems), followed by psychological (14.8%) and musculoskeletal (14.2%) problems. Depression and anxiety were the most common individual psychological problems managed, and back complaint and sprain/strain were the most common musculoskeletal problems.
Men aged 45–64 years most commonly had musculoskeletal (14.0%), circulatory (12.7%), and general and unspecified (such as check-ups; 12.4%) problems managed. The chronic conditions hypertension, diabetes, lipid disorders and depression were the most common individual problems managed, together accounting for 17.7% of problems in this age group.
Men aged 65 years and older had circulatory (20.2%), skin (12.0%), and general and unspecified (11.9%) problems commonly managed. Hypertension (9%), diabetes (5%), osteoarthritis (3%) and lipid disorders (3%) were the most common individual problems.
Male-specific problems (those classified as related to the genital system) accounted for a small proportion of all problems managed in men. These problems were more common at encounters with older men (3.3% of problems) than at those with men aged 45–64 years (2.9%) and 15–44 years (2.4%).
Discussion
Sex-specific changes in GP service use occur during adolescence. While the majority of young women continue to have regular contact with GPs, the same cannot be said for young men. For women, this is likely to be due to the need for ongoing contact for cervical cancer screening, contraception and reproductive issues. Men in the 15–44 year age group are the least likely of all age–sex groups in the Australian population to have seen a GP at least once in a year, and have the lowest number of attendances per head of population.
Lower attendance patterns do not necessarily indicate that young men have a problem with access to GPs or that there is an unmet need for services. It would be expected that younger men would be healthy and have less need for GP services. However, our study demonstrates that they are the least likely to have a regular general practice and to have visited a GP. This picture is consistent with previous studies.4,5 Young men are also more likely than other age–sex groups to engage in risky behaviours, such as at risky alcohol consumption and tobacco smoking.7,9 GPs should be mindful that young men may not have established an ongoing relationship with a GP or practice. Encouraging such a relationship is thought to support continuity of care, disclosure of sensitive information and optimal health outcomes.10,11
The types of problems GPs managed at encounters with male patients changed with increasing patient age. The patterns identified were similar to the results from the 1999–2000 study.5 In the younger age group, acute conditions, injury and psychological problems were common. From the age of 45 years onward, chronic diseases start to emerge among the most common problems. For older men, chronic diseases are the predominant types of problem managed.
Traditionally, discussion about men’s health focuses on male-specific problems. Men are encouraged to talk to their doctor about their ‘tackle – those bits below the belt’.12 We applaud this, but our study highlights that such problems account for a small proportion of all problems dealt with in men in general practice.
A holistic approach to men’s health would be beneficial, particularly in young men who are less frequent users of GP services and may miss out on the benefits (such as prevention, continuity of care and early diagnosis of disease) associated with a having a regular practice.
Authors
Clare Bayram BAppSc (HIM) (Hons), PhD, Research Fellow and Project Manager, BEACH program, Family Medicine Research Centre, Sydney School of Public Health, Sydney Medical School, University of Sydney, Parramatta, NSW. clare.bayram@sydney.edu.au
Lisa Valenti BEc, MMedStat, Senior Research Analyst, Family Medicine Research Centre, Sydney School of Public Health, Sydney Medical School, University of Sydney, Parramatta, NSW
Helena Britt BA, PhD, Professor of Primary Care Research, Director, Family Medicine Research Centre, Sydney School of Public Health, Sydney Medical School, University of Sydney, Parramatta, NSW
Competing interests: None.
Provenance and peer review: Commissioned, externally peer reviewed.
Acknowledgements
We wish to thank the general practitioners who participated for their generosity. During the data collection period of this study, the BEACH program was funded by the Australian Government Department of Health, AstraZeneca Pty Ltd (Australia), Novartis Pharmaceuticals Australia Pty Ltd, bioCSL (Australia) Pty Ltd, AbbVie Pty Ltd, Merck Sharp & Dohme (Australia) Pty Ltd, and the Australian Government Department of Veterans’ Affairs. Funding organisations had no editorial control over any aspect of this article.