Case
A previously well girl, 13 years of age, presented to the emergency department at a rural hospital complaining of a ‘crawling’ foreign body sensation in her right eye. Several hours earlier, she had been by the Murrumbidgee River when she felt something go into her eye.
On examination, the right eye showed diffuse conjunctival hyperaemia without evidence of discharge or ciliary injection. Visual acuity and external ocular movements were unimpaired, and both pupils remained equal and reactive to light. On close examination under slit-lamp magnification, multiple small, live larvae, measuring 1–2 mm, were noted on the conjunctiva. The left eye was of normal appearance.
Saline washout was attempted without success and the larvae could not be brushed away with a cotton tip. After administration of local anaesthetic drops, removal of approximately 30 larvae was performed with jeweller-style ophthalmic forceps. The patient was discharged home on a course of chloramphenicol eye drops and encouraged to re-present if she experienced ongoing issues. Fresh specimens were sent to the local laboratory, where they were placed in saline solution and transferred to the medical entomology department at a tertiary hospital. The organisms were subsequently identified as first instar Oestrus ovis larvae (Figure 1).
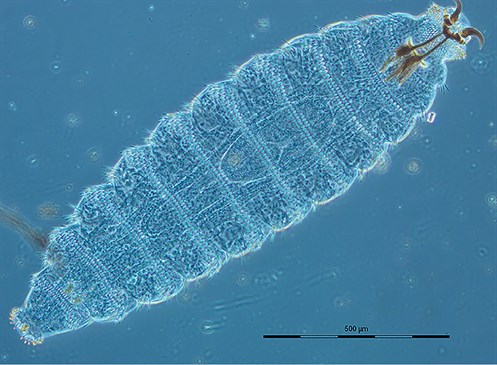
Figure 1. First instar Oestrus ovis larvae collected from the conjunctiva of the patient. Note the oral hooks used to grasp onto the host’s tissue
Question 1
What is the diagnosis?
Question 2
What are the differential diagnoses? How can primary care physicians differentiate a presentation of ophthalmomyiasis from other causes of red eye or foreign body sensation?
Question 3
Which flies can cause ophthalmomyiasis? How are the flies transmitted?
Question 4
What are the risk factors of ophthalmomyiasis? How common is this condition?
Question 5
Given that livestock are key hosts of O. ovis, do drenching practices help prevent external ophthalmomyiasis?
Question 6
How is this condition treated?
Question 7
What are the complications if the diagnosis is missed?
Answer 1
This case describes a presentation of external ophthalmomyiasis, which is the invasion of ocular tissues by the larvae of dipterous flies.1
Answer 2
On the basis of multiple case series, the typical symptoms of ophthalmomyiasis include sudden-onset ‘crawling’ foreign body sensation, pain and itch. Frequently reported signs include conjunctival hyperaemia, chemosis, watery discharge and eyelid oedema.2–5 In addition, fluorescein staining may reveal punctate epithelial erosions.3
Common differential diagnoses of a foreign body sensation, with or without red eye, include true foreign bodies (ie metal/organic) and conjunctivitis (viral, bacterial or allergic). Conditions such as episcleritis, scleritis and keratitis are more easily differentiated, but should be considered.6
Definitive diagnosis requires visualisation of larvae by examination under adequate illumination and magnification, ideally a slit-lamp biomicroscope, loupe or 20D lens. Larvae are commonly found within the fornices, measuring approximately 1–2 mm.2,3
Answer 3
Commonly recognised causative species of ophthalmomyiasis are the cattle botfly (Hypoderma bovis), the Russian botfly (Rhinoestrus purpureus) and, as exemplified in this report, the nasal botfly (O. ovis).3 As obligatory parasites, they complete a large part of their lifecycle developing in the nasal sinuses of sheep and goats before being sneezed out to pupate among the pasture. Infestation has also been reported in domestic cats and dogs.7 Transmission occurs when the gravid female ejects a stream of milky fluid containing first instar larvae onto the animal’s mucous membranes. This act can be performed from up to 0.5 m away.2,8
Answer 4
Risk factors of ophthalmomyiasis may include those that increase exposure to flies, namely young age, alcohol abuse, debility and close contact with farm animals.2,3 While the incidence has not been epidemiologically described, many authors suspect under-reporting because of poor clinician awareness.2,3,9 A PubMed literature review was performed using the combined search terms ‘ophthalmomyiasis’ (title) and ‘Oestrus ovis’ (all fields), with results limited to English language. The authors noted that within Australian literature, there are only a handful of detailed reports, the first by Thyer in 1967, and none published in the past 30 years.8
Answer 5
Livestock drenching practices in Australia are not recommended as routine treatment for O. ovis infestations; however, some drenching products, such as macrocyclic lactones (eg ivermectin), are reportedly effective against O. ovis.7 The infestation rate within Australian livestock is poorly described since the introduction of these agents.10
Answer 6
The removal of larvae using fine forceps under the aid of local anaesthetic eye drops has been used with good success. Flushing or removal with a damp cotton-tip is typically unsuccessful as the larvae cling onto ocular tissues with their oral hooks (Figure 1). Most authors recommend prophylactic topical antibiotics following larvae extraction to prevent secondary infection.2,3 The adjunctive administration of oral ivermectin has proven effective in cases of concurrent nasal myiasis.3,4
Answer 7
O. ovis larvae are not able to mature in the human host; yet, if the diagnosis is missed, they will live for up to 10 days on the ocular surface, causing severe inflammation that may preclude eye opening.2,8 Ophthalmomyiasis may be limited to superficial structures such as the conjunctiva, or rarely may penetrate the globe or invade orbital tissue.1 The risk of complications differs depending on the causative organism; hence, taxonomic identification is essential in guiding prognosis.3,8
Key points
- Ophthalmomyiasis should be considered in those presenting with a history of sudden onset unilateral red eye or foreign body sensation in rural regions.
- Diagnosis requires careful examination under best available magnification and illumination.
- Treatment requires manual removal of larvae with fine forceps. Larvae should be sent for laboratory identification to guide prognosis.
Authors
Julian C Kelman BMed, Resident Medical Officer, St Vincent’s Hospital Sydney, Darlinghurst, NSW; Wagga Wagga Rural Referral Hospital, Wagga Wagga, NSW. julian.kelman@icloud.com
Zachary E McPherson BMedSci, PhD candidate, School of Medicine and Public Health, University of Newcastle, NSW
Benjamin WC Sim MBBS, MPH, Ophthalmology Registrar, Wagga Wagga Rural Referral Hospital, Wagga Wagga, NSW; Sydney Eye Hospital, Sydney, NSW
Competing interests: None.
Provenance and peer review: Not commissioned, externally peer reviewed.
Acknowledgement
Photograph with thanks to parasitologist Dr Rogan Lee and Senior Technical Officer Merilyn J Geary, Medical Entomology, Pathology West, Westmead Hospital, NSW, Australia.