‘There’s something in my eye!’ This is a common ophthalmic problem in the rooms of general practitioners (GPs). The Royal Australian College of General Practitioners’ (RACGP’s) 2016 curriculum includes ‘the removal of a foreign body, including any residual corneal ulcer or rust’ as a required skill.1 Variability of access to a slit lamp is acknowledged by the RACGP.2 However, safe and effective initial assessment and management of corneal foreign bodies can be carried out with a good history, examination and intervention using readily available equipment.
History
A thorough history of symptoms, mechanism of injury, suspected material involved, timing of the incident and an ocular history will direct management approach. Symptoms include a foreign body sensation, grittiness, irritation, pain, redness, photophobia, blurred vision and excessive watering of the eyes. A particular inciting event will usually be recalled.
Metallic foreign bodies in the context of hammering or drilling metal-on-metal (Figure 1A), particularly in the absence of protective eyewear, may just embed in the corneal surface but can penetrate the eye if travelling at sufficiently high velocity.3,4 In the case of globe penetration, urgent referral to the nearest emergency department with ophthalmological care should occur.5 Foreign bodies involving organic material, such as those sustained while gardening, carry a high risk of infection and often warrant referral. Seeds (Figure 1B), insect scales (Figure 1C) and caterpillar setae are infrequent, but have well-described vision threatening consequences.6
The time of the incident is important. A superficial foreign body embedded earlier that day is particularly amenable to removal in a GP’s office as there will be no encroaching corneal epithelium and no rust ring. If the inciting event occurred a few days prior, and there has been an increase in pain, significant worsening of vision and diffuse conjunctival redness (Figure 1D), then a corneal infection and/or endophthalmitis are more likely and urgent referral is indicated.
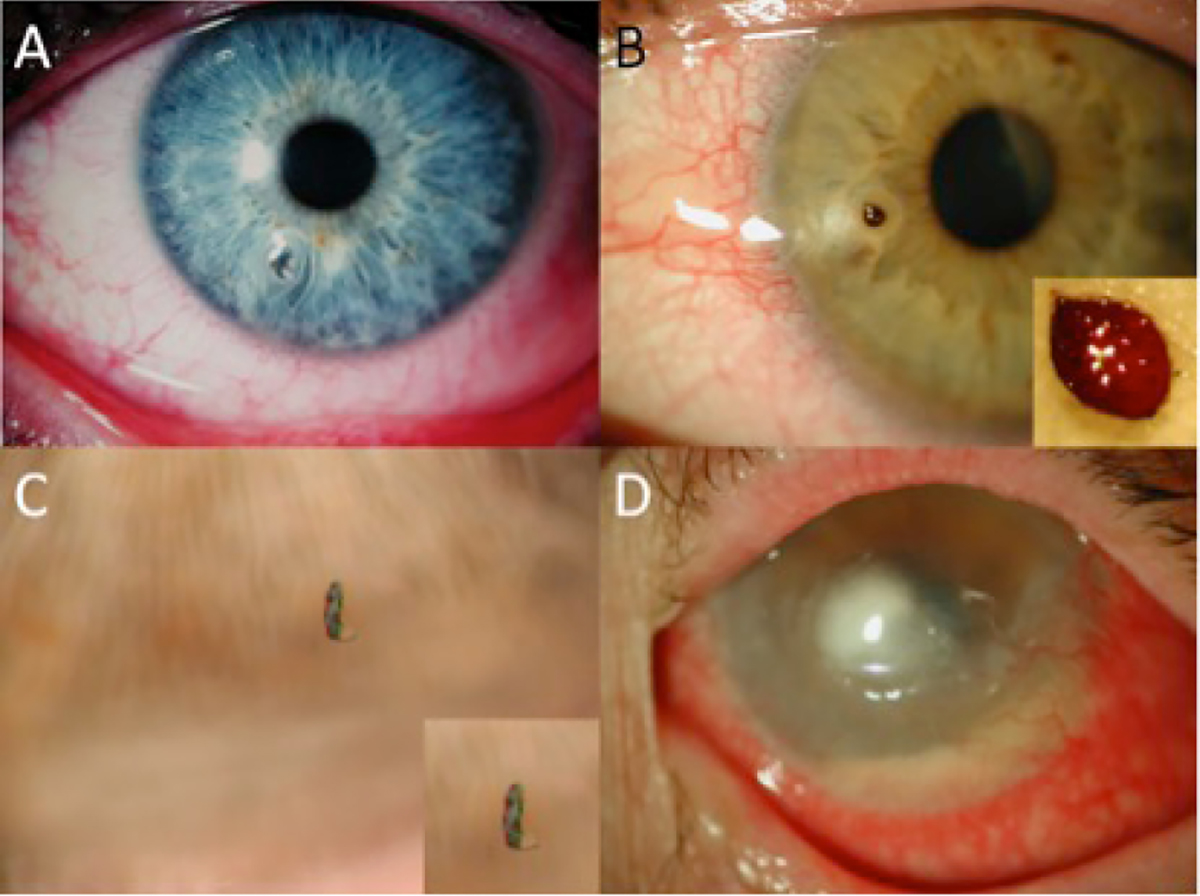
Figure 1. Corneal foreign bodies
A. Metallic particle from drilling; B. Seed; C. Insect scale; D. Keratitis and endophthalmitis from a contact lens
It is important to note any previous eye conditions. Concurrent contact lens use is an indication for referral because of the risk of severe infection with unusual organisms. Do not commence antibiotics as microbiological specimens may need to be taken. Take care to ensure that amblyopia or pre-existing poor vision in an eye is not mistaken for a reduction in visual acuity associated with a foreign body.
Examination
The equipment required for the office-based examination and removal of a corneal foreign body is outlined in Box 1.
Box 1. Equipment for removal of a corneal foreign body in a general practitioner’s office
- Snellen chart
- Bright light source (eg pen torch, ophthalmoscope or a medical light on a stand or wall-mounted)
- Eyelid speculum (optional)
- Loupes (if available)
- Fluorescein strip or drops
- Topical anaesthetic drops (eg oxybuprocaine 0.4%)
- Cobalt blue light, from an ophthalmoscope or Wood’s lamp
- Sterile cotton tips
- Sterile normal saline
- Sterile 25G 16 mm hypodermic needle or 15 scalpel blade
|
Visual acuity
This is the most important but often overlooked parameter to document in the patient’s medical notes. If there are no available hard copies of a Snellen chart, it is sufficient to use those available via smartphone apps or downloaded from the internet. Snellen charts do not have to be positioned at the traditional 3 m or 6 m if these distances are not achievable, as long as the distance used and distance specified by the visual acuity chart, particularly if it is from the internet, are recorded. A drop of topical anaesthetic can be instilled to reduce interfering photophobia. If the patient cannot see any letters, move the chart closer. In the case of a greater visual deficit, record whether the patient can ‘count fingers’ and the distance at which this is possible. If their vision does not permit them to count fingers, record whether they can detect ‘hand movement’ or have ‘perception of light’ at a distance of 10 cm.
Conjunctiva, cornea, anterior chamber and pupils
These structures can be examined with a bright-focused light, such as a pen torch, ophthalmoscope or loupes. An ophthalmoscope provides a magnified view of these structures when dialled to +10D and held at 10 cm.7
The location, size and depth of the corneal foreign body should be noted, particularly if it is in the central pupillary zone. Surrounding corneal opacity may indicate a rust ring, burn, infection, oedema or scar tissue. Irregularities in pupil shape may indicate a penetrating foreign body causing iris incarceration.
Eyelid eversion
If there is no sign of penetration, the upper and lower eyelids of both eyes should always be single everted (Figure 2A) to examine for foreign bodies on the tarsal plate (Figure 2B), and the upper lids double everted (Figures 2C, D) to look for foreign bodies in the upper fornix. These can be easily missed, causing the patient ongoing foreign body symptoms despite removal of the corneal lesion.
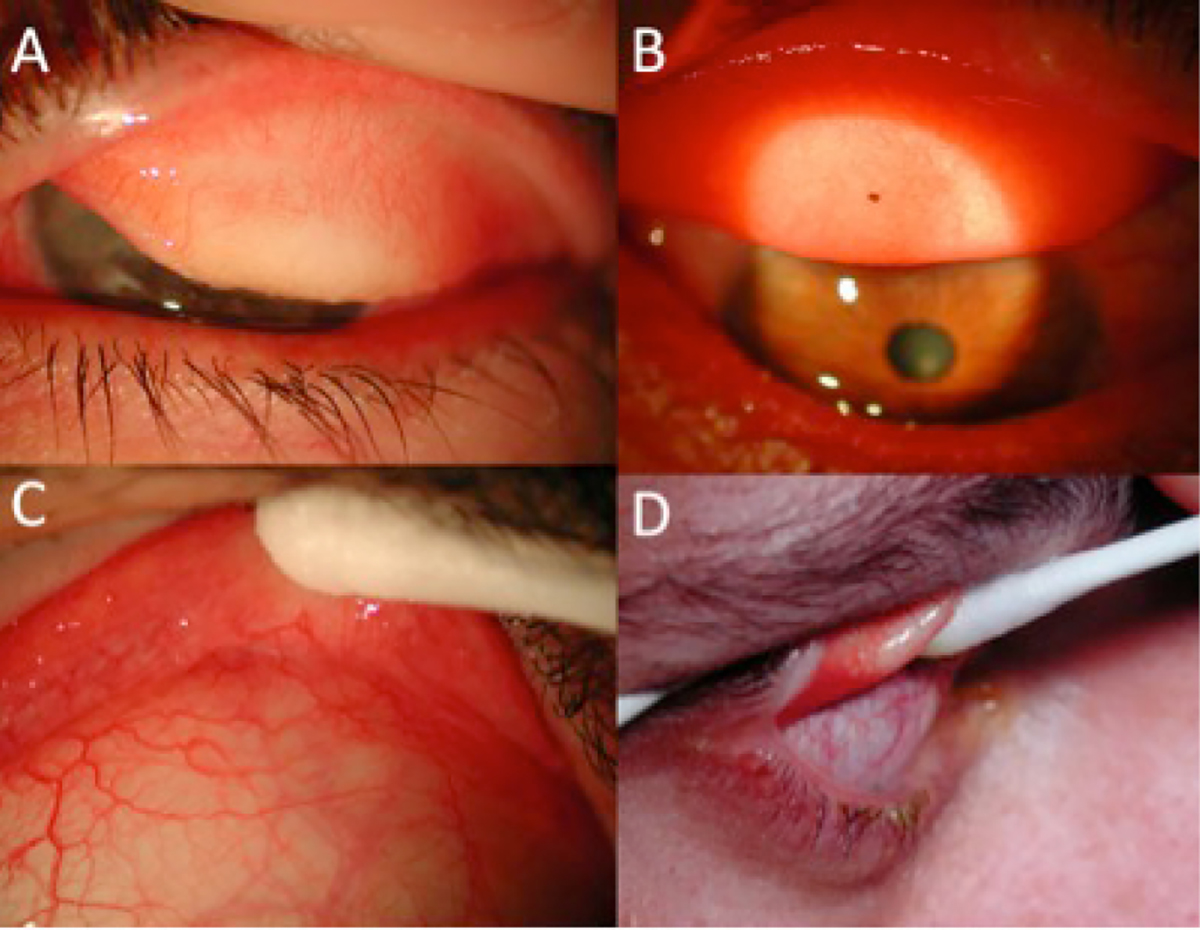
Figure 2. Eyelid eversion
A. Single eversion; B. Subtarsal foreign body; C. Double eversion of eyelid with moist cotton tip; D. Side view of double eversion
Fluorescein
Fluorescein is used to detect any epithelial defect associated with the foreign body. It can be instilled via a moistened strip or as drops, and the ocular surface viewed with a cobalt blue filter from an ophthalmoscope or a Wood’s lamp. Multiple vertically orientated linear abrasions should raise suspicion of a tarsal plate foreign body. The Seidel’s test using 2% fluorescein can detect an aqueous leak that will occur in non–self sealing corneal perforations.
Differential diagnosis
A corneal abrasion with no foreign body is a possible alternative diagnosis. The cornea is densely innervated by free nerve endings, which makes it difficult to distinguish between an abrasion and a foreign body on the basis of symptoms alone. Of 1155 consecutive patients presenting to a UK emergency department with an ocular foreign body sensation, 157 (13.6%) had a corneal abrasion only.8 If no foreign body can be found in the GP’s office examination and the foreign body sensation persists overnight, referral should be made for review of the eye on a slit lamp.
Other differential diagnoses include Herpes simplex virus (HSV) keratitis, exposure keratopathy, chemical exposure, ultraviolet exposure or ‘welding flash’ and recurrent corneal erosion syndrome.3,9 These can be differentiated on the basis of history.
Investigations
Generally, a corneal foreign body does not require further investigation. If there is suspicion of ocular penetration, an orbital X-ray, including lateral and anterior–posterior views, or computed tomography (CT) scan can be requested. Magnetic resonance imaging (MRI) is avoided in case of metallic foreign bodies.
Removal of the foreign body
Refer to the list of equipment in Box 1.
Positioning
Lay the patient in a comfortable supine position, with the involved eye closest to the attending clinician. Wear loupes if they are available and illuminate the eye with a medical light or, alternatively, use the light and magnification from the ophthalmoscope held in the non-dominant hand. Unfortunately, the ophthalmoscope does not facilitate stereopsis. Ask the patient to focus on a particular point on the ceiling so that the foreign body sits as centrally between the lids as possible. Avoiding the lids and lashes is more sterile, and reduces the chance of eliciting a blink reflex. If necessary, the eyelids can be kept open using an eyelid speculum, the examiner’s fingertips, a cotton tip or an assistant.
Anaesthetic and pupil dilator
Instil local anaesthetic into both eyes as this reduces blepharospasm. Topical oxybuprocaine 0.4% takes approximately 20 seconds to work and lasts for 20 minutes. A drop of topical pupil dilator such a cyclopentolate 1%, if available, can be helpful to reduce ciliary spasm after removal of a foreign body. Avoid atropine as its effects of pupil dilation and loss of accommodation can last for two weeks or more.10
Removal techniques
The choice of technique will depend on the nature of the foreign body, remembering that whatever instrument is used, the eye should be approached from the side within a plane less than 5 cm from the face. This is less confronting for the patient as they will not be able to clearly focus on the object, and eliminates the blink reflex caused by an object approaching the eye front-on.
Cotton tip removal
Superficial foreign bodies with no surrounding corneal reaction can often be removed in a dabbing or nudging motion with a cotton tip soaked with local anaesthetic or saline.
Hypodermic needle (25G 16 mm) or 15 blade removal
Corneal thickness is 0.55 mm centrally, and thicker peripherally, so the removal of superficial foreign bodies poses a low risk for perforation if a safe technique is observed. It can be helpful to bend the tip of the needle 90° away from the bevel using sterile forceps or the needle cap. Mount the needle on the end of a cotton tip and work with the bevel side away from the eye. The needle (Figure 3C) or blade (Figure 3D) should be held tangential to the eye surface. Motions when performing the procedure should come from the finer joints of the fingers, with the hand resting on a firm point of contact.
The aim of the procedure is the safe and complete removal of the foreign body and any surrounding rust ring (Figure 3A–D). It is best to accomplish this in one to two sittings in total, so if there is any doubt this has not been achieved then referral for slit lamp examination and complete removal is advised. The site of a residual rust ring, even at the peripheral cornea, is at risk of infection and recurrent erosion. The flat part of the 15 blade tip can be useful to remove the rust ring (Figure 3D). Dental burrs should be avoided because of the risk of deeper damage to the corneal stroma and infection from the usual non-sterile status of the instrument.
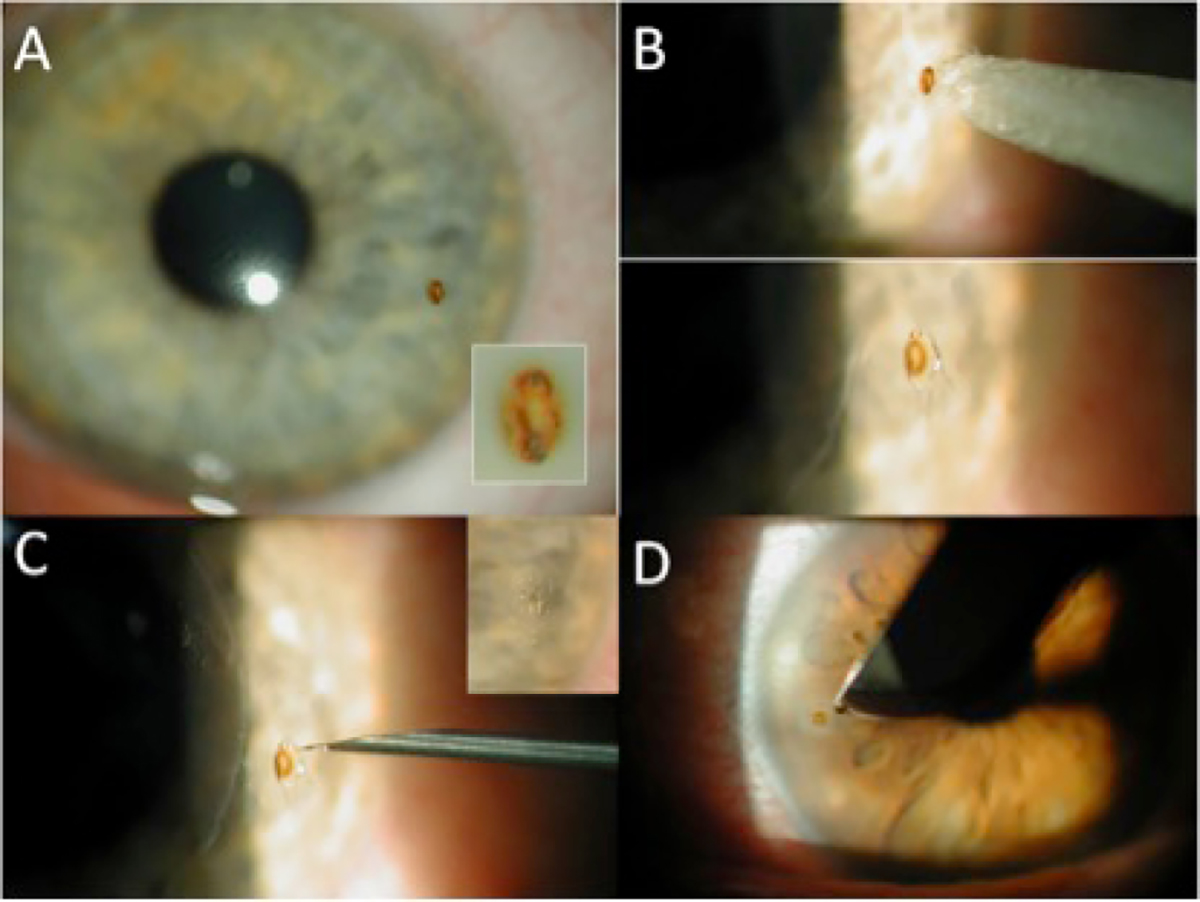
Figure 3. Rust rings
A. Corneal rust ring; B. Use of moist cotton tip; C. Further removal with 25G hypodermic needle; D. 15 blade scalpel
Irrigation
Irrigation of the ocular surface and upper and lower fornices can be performed after the procedure to wash out any residual loose foreign body material. A 10 mL ampoule of sterile saline is usually sufficient.
Post-procedure
Antibiotic ointment such as chloramphenicol 0.5% should be instilled and a double eye pad applied, with the inner one doubled over in a manner that the eyelid cannot be opened. The patient needs instruction not to drive or operate machinery while wearing the eye pad. This must be documented clearly in the patient’s medical notes. Generally, eye pads are kept on for a period of 24 hours to expedite healing of the epithelial defect and for pain relief. An alternative approach is to omit the eye pad but use the antibiotic ointment or drops four times a day. This depends on the doctor’s and patient’s preference. The literature strongly suggests that there is no difference in time to healing or complication rate with or without patching.11,12 Over-the-counter oral analgesia can be used for pain relief. Do not discharge the patient with topical anaesthetic drops; these result in an increased complication rate from corneal anaesthesia.13 Laboratory research also suggests time-dependant and dose-dependant toxicity.14
The patient can be examined the following day to measure visual acuity again and repeat fluorescein staining. Any increase in pain, photophobia, redness, epithelial defect size or opacity may indicate the onset of keratitis and requires a referral. Topical antibiotics in the form of ointment or drops, which are less blurring, are continued four times a day for five to seven days. This visit is also an opportune time for patient education on the importance of wearing eye protection while undertaking activities that pose risks. A certificate of leave from work or study for one to two days is not unreasonable.
Box 2. Indications for referral to an ophthalmologist
- Penetrating eye injury or intraocular foreign body
- Incomplete removal or practitioner uncertainty
- Persisting foreign body symptoms
- Persisting rust ring
- Persisting vision loss
- Keratitis
- Endophthalmitis
- Persisting epithelial defect
- Recurrent erosion
- Paediatric or uncooperative patients that may require examination under anaesthesia
|
Paediatrics
Patients younger than 10 years of age are much less likely to tolerate examination and foreign body removal. Irrigation and removal with a cotton tip can be attempted after instillation of topical anaesthetic drops, provided the patient’s head can be stabilised with safety. If there is any concern, the patient needs to be referred to a paediatric facility where examination and treatment under general anaesthesia are possible.
Referral and prognosis
Most corneal foreign bodies result in minimal superficial scarring of no visual significance. However, removal of a corneal foreign body without the aid of a slit-lamp can be a challenging procedure, and if the GP does not feel safe to proceed, referral to an ophthalmologist is warranted. This pertains particularly to central and paracentral corneal foreign bodies that are deeper than expected. Even when removed with minimal iatrogenic trauma, this location caries a higher risk of a visually significant corneal scar. Pertinent indications for referral are summarised in Box 2.
Key points
- Initial assessment and management of corneal foreign bodies is within the scope of a GP.
- A moistened cotton bud, 25G hypodermic needle or 15 blade is a suitable approach for superficial foreign bodies and rust rings in the office provided there is good light, adequate magnification and a cooperative patient.
- Referral to an ophthalmologist is indicated if there are any concerns.
Authors
Alison Fraenkel BBiomedSc, MBBS, Preclinical Fellow, City Eye Centre, Brisbane, Qld
Lawrence R Lee MBBS, FRANZCO, FRACS, Associate Professor, City Eye Centre, University of Queensland; Royal Brisbane & Womens Hospital, Brisbane, Qld. eye@cityeye.com.au
Graham A Lee MD, MBBS, FRANZCO, Associate Professor, City Eye Centre, University of Queensland; Mater Hospital, Brisbane, Qld
Competing interests: None.
Provenance and peer review: Commissioned, externally reviewed.