Injury to the tarsometatarsal joint, commonly referred as the Lisfranc joint, is a relatively rare occurrence.1 However, it is considered a red flag condition in general practice because of the debilitating consequences of a missed diagnosis.2 Awareness and a high degree of clinical suspicion is vital for this diagnosis, as it has been estimated that 20–40% of Lisfranc injuries are initially missed.3,4 The technical definition of a Lisfranc injury involves the displacement of one or more of the metatarsals from the tarsus, and injuries can range from subtle subluxations to obvious fracture dislocations. Clinically, the term is sometimes used to specifically describe an injury involving the second tarsometatarsal joint.5,6
The Lisfranc joint complex was named after a 19th century French army field surgeon who first described amputation through this location.7 It represents the junction between the forefoot and mid-foot, and is composed of the tarsometatarsal articulations and associated ligaments.3 The ligaments supporting this joint can be broadly classified into dorsal, plantar and interosseous ligaments.8 The strongest and most clinically significant ligament is the interosseous Lisfranc ligament, which transverses from the base of the second metatarsal to the plantar surface of the medial cuneiform (Figure 1).9,10 Importantly, given the arrangement of these ligaments, the dorsal aspect of the joint is significantly weaker than the plantar aspect.7
Several interlinked classification systems exist for Lisfranc injuries; however, they are all based on a three-column conceptualisation of the mid-foot as shown in Figure 1.5–7,9 The Hardcastle Classification System is commonly used. It divides the injuries into types A, B and C (Figure 2).7
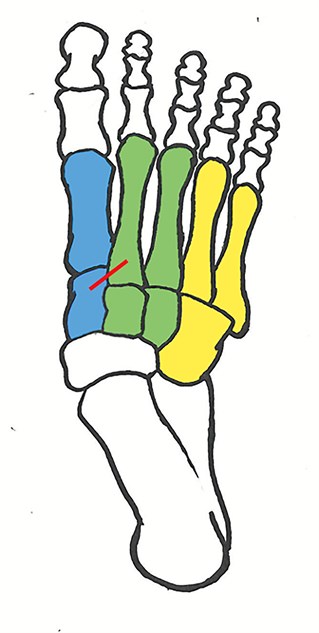
Figure 1. Anatomy of the mid-foot
The joint is often separated into three columns: medial, middle and lateral columns. The Lisfranc ligament (red) is the most clinically significant ligament 9,10
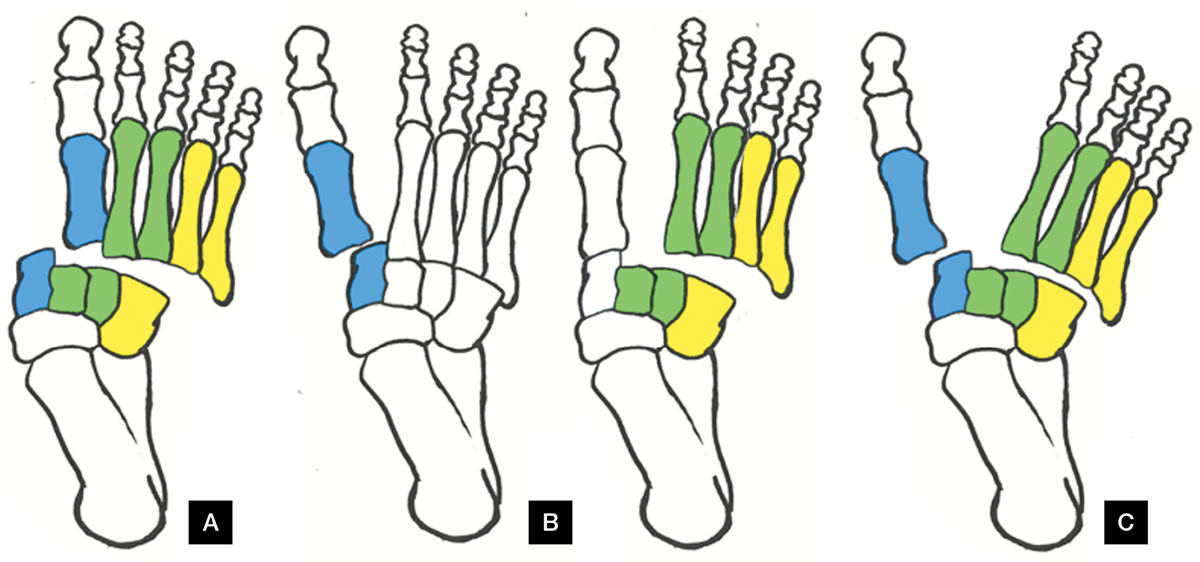
Figure 2. Hardcastle Classification System
Type A. Injuries involve an incongruity of the entire joint. Type B. Refers to injuries where a partial segment of the joint is displaced. Type C. Injuries are described as divergent; the first metatarsal is displaced medially with any combination of the remaining four etatarsals displaced laterally.7
Mechanism of injury
Lisfranc injuries can arise from a variety of situations and mechanisms, with both direct and indirect injuries possible. Direct injuries are due to a force applied to the dorsum of the foot. Direct injuries are the most common cause of Lisfranc injuries, with motor vehicle accidents, crush injuries and falls from a height being prominent mechanisms.3,5,9 There is often associated soft tissue injury, vascular compromise and other fractures.4,9
One-third of Lisfranc injuries are caused by indirect trauma, which are more commonly missed.5,9 The main mechanism of indirect injury is axial force through the foot or twisting on a plantar-flexed foot. Forced external rotation of the foot is another documented mechanism. These mechanisms are all very common in sports (eg football, equestrian activities), but also possible in household accidents and falls.3,4,9 It is because of these commonly occurring mechanisms that Lisfranc injuries warrant such a high degree of clinical suspicion.
Clinical presentation
The clinical presentation of Lisfranc injuries is as diverse as the possible mechanisms, and a high degree of clinical suspicion is often needed to diagnose subtle injuries.11 Plantar ecchymosis is considered pathognomonic for a Lisfranc injury.12 Other clinical signs that should trigger clinicians’ suspicions include swelling in the mid-foot and pain during attempted weight-bearing, especially mid-foot pain when walking down stairs.1,9
On examination, pain may be elicited by palpation of the dorsal aspect of the involved tarsometatarsal joints. Provocative tests include:
- Piano-key test – the metatarsals are grasped, and passive dorsiflexion and plantar flexion is performed at the tarsometatarsal joint (Figure 3). Subluxation or pain suggests injury.1,9
- Mid-foot compression with dorsal and plantar flexion of the first metatarsal head relative to the second metatarsal head.13
- Compression across the width of the foot to stress the space between the first and second metatarsals (Figure 4). Pain or a palpable click is suggestive of a Lisfranc injury.1,14
- Passive pronation with abduction of the forefoot, while the hindfoot is held still. Pain is a positive result, which is considered specific for tarsometatarsal injuries.6,14
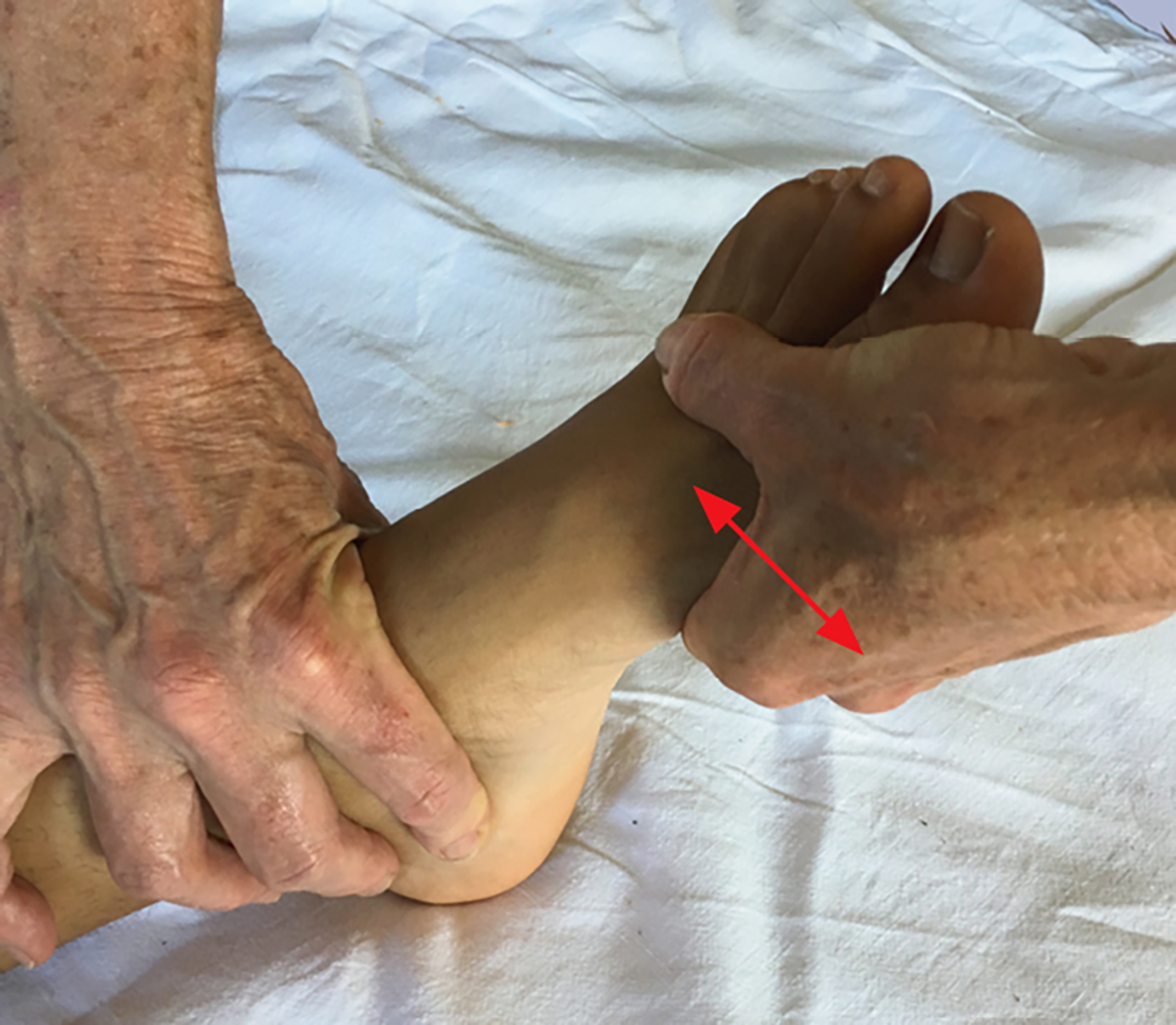
Figure 3. Piano-key test
The metatarsals are grasped, and passive dorsiflexion and plantar flexion is performed at the tarsometatarsal joint.1,9 This position can also be used to assess passive pronation with abduction of the forefoot.6,14

Figure 4. Provocative test
Compression across the width of the foot to stress the space between the first and second metatarsals. Pain or a palpable click is suggestive of a Lisfranc injury.1,14
It is important to examine the entire foot and ankle for synchronous injuries, although acute swelling and discomfort of the foot can impair this assessment. Signs of an unstable injury include a broadened foot and shortening in the anteroposterior plane.6 In these situations, it is important to consider the nearby neurovascular bundle, consisting of the dorsalis pedis artery and deep peroneal nerve.10 Severe fracture dislocations can result in vascular compromise and, occasionally, consequential ischaemic injury.3,6,10 Compartment syndrome of the foot is another rare complication.6
Investigations
First-line investigations for a suspected Lisfranc injury include bilateral weight-bearing anteroposterior radiographic imaging with 30° oblique, and lateral views of the involved foot and ankle.1,4 The anteroposterior view is ideal for assessing the first and second tarsometatarsal joint, with the remaining joints assessable in the oblique and lateral radiographs.9 Comparison of bilateral weight-bearing anteroposterior views is necessary to assess joint space widening and instability.2,9 The fleck sign is often seen on anteroposterior views. It is a small avulsion fracture from the Lisfranc ligament, which is present at the medial base of the second metatarsal or medial cuneiform. This sign is considered pathognomonic for Lisfranc injuries.1,10
Weight-bearing radiographs are vital to identify subtle injuries, and every effort should be made to obtain them.4 If acute pain makes obtaining these difficult, it may be useful to wait one week before imaging.1,4 Lisfranc injuries can be very subtle, with up to 20% of cases missed on initial radiographs.8 If there is a high clinical suspicion of injury, computed tomography (CT) is a useful next step. Thin-cut CT imaging often identifies small fractures and subtle subluxation of the joint. Magnetic resonance imaging (MRI) can be useful in assessing the Lisfranc ligament.1,4,15 Abducted stress radiographs of the affected foot may be useful to demonstrate dynamic instability of the Lisfranc joint complex.1
Management
Patients with inadequately stabilised injuries have a high risk of developing debilitating post-traumatic degenerative changes and generally poor outcomes.1,4 Orthopaedic referral is indicated whenever there is a proven Lisfranc injury or a high degree of clinical suspicion. Patients should be kept non–weight bearing until the review.2
Non-operative management
Non-operative management is indicated only for patients who clinically present with a Lisfranc injury but have no evidence of instability or diastasis on weight-bearing radiographs. Often, an MRI shows a Lisfranc ligament sprain. Correct management of these patients is crucial, as purely ligamentous injuries often have a poor prognosis.1,4 Physiotherapy input would be a valuable addition at all stages of conservative management.
Recently, it has been suggested that these patients be managed in a progressive, stepwise fashion. For the first two weeks, the foot should be immobilised in a short walker boot with protective weight-bearing. After the initial two weeks, the patient should be re-examined and weight-bearing radiographs repeated.1,9 If there is no tenderness over the joint line and no diastasis on imaging, the patient should be encouraged to weight-bear with the short boot as tolerated for the next six to eight weeks. Once the patient is pain-free under abducted stress, they can swap to a stiff-soled shoe with rigid orthotic support for the next six months. Running on uneven surfaces and twisting activities should be discouraged for the first three to four months, to minimise the risk of recurrence. Athletes should expect a recovery period of at least 6–12 months before returning to competitive activity is possible.1
Surgical management
Any evidence of dynamic instability or clear diastasis at the Lisfranc joint requires operative management. There are numerous techniques for surgical stabilisation of these injuries, with the best method being a controversial topic. Regardless of method, meticulous anatomical reduction is essential for optimal outcomes. Patients with a statically reduced joint but dynamic instability are generally good candidates for percutaneous reduction and internal fixation; however, numerous other authors argue for open reduction.1,4,12 Arthrodesis is occasionally indicated.1 Postoperatively, patients should remain non–weight bearing for two to four weeks, with their foot immobilised in a short leg splint or cast.1,4,9,14 After this time, sutures are typically removed and postoperative weight-bearing radiographs should be obtained. From two to six weeks postoperatively, partial weight-bearing in a short controlled ankle motion (CAM) boot is recommended.1 Then, from six weeks to three months postoperatively, patients should transition to a supportive shoe with an orthotic insert as comfort allows.1,9 The exact timeline of this stepwise progression is controversial and general practitioners (GPs) should refer to the personalised advice given by the orthopaedic surgeon.1,4,7
High-impact activity is discouraged until any metal work is removed; however, low-impact activity is encouraged as tolerated. General return to athletic activity is allowed as for non-operative management.
Complications
Given the intrinsic instability of the mid-foot, post-traumatic arthritis is a potentially devastating but common complication of poorly treated or missed Lisfranc injuries. Even after surgical fixation, approximately 40–94% of patients develop this, often requiring conversion to a mid-foot arthrodesis.1 Chronic pain and loss of working productivity are also common.16
Conclusion
A high degree of clinical suspicion is often needed to diagnose subtle Lisfranc injuries, along with an awareness of physical signs and obtaining weight-bearing radiographs. Correct diagnosis is imperative given the high risk of post-traumatic degenerative changes. Clinical presentation of a Lisfranc injury with no radiographic evidence usually reflects a Lisfranc ligament sprain and can be managed conservatively. Any evidence of instability or diastasis of the joint requires an orthopaedic referral for surgical fixation.
Authors
Sacha Wynter BSc, Griffith Medical Student, Dalby Hospital, Dalby, Qld. sacha.wynter@griffithuni.edu.au
Cameron Grigg MBBS, General Surgery Principle House Officer, Toowoomba Base Hospital, Qld
Competing interests: None.
Provenance and peer review: Not commissioned, externally peer reviewed.