Case
A man of Indian descent, 46 years of age, underwent a renal transplant two years ago for lupus nephritis. Aside from systemic lupus erythematosus, the patient had no other medical comorbidities. Immunosuppressive therapy included azathioprine 50 mg twice daily, tacrolimus 1 mg twice daily and prednisolone 5 mg daily. A 2 mm pigmented macule on his right sole was detected during a routine skin check (Figure 1). The pigmented lesion had not been noted previously. On examination with the naked eye, the lesion was unusual as it was darkly pigmented. Dermoscopy revealed a parallel ridge pattern with diffuse varying pigment and no involvement of furrows (Figure 2).

Figure 1. A 2 mm pigmented macule on the right sole
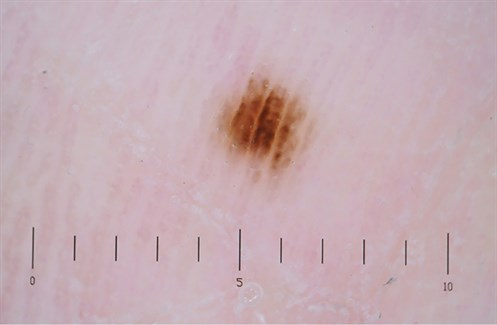
Figure 2. Dermoscopy image showing a parallel ridge pattern and no involvement of furrows
Question 1
What are the differential diagnoses to consider in this patient?
Answer 1
In this case, the top differentials include acral melanoma and acral naevus. Acral melanoma is the most frequent subtype of melanoma diagnosed in Asian populations.1−4 Organ transplant recipients are also at increased risk of developing melanoma.5 Acral melanoma and acral naevus usually have different dermoscopic patterns, so dermoscopy is useful in differentiating between them.2,4 Given the history of immunosuppression and the signs on dermoscopy, melanoma needs to be excluded in this patient.
Case Continued
An excisional biopsy was performed, removing the entire lesion. Histopathology reported a benign acral lentigo with no evidence of atypical melanocytic proliferation, dysplasia or malignancy. It is important to note that an excisional biopsy is recommended for the removal of suspicious pigmented lesions.6,7 Sometimes the biopsy technique may vary depending on the size and location of the lesion. Partial biopsies of pigmented lesions are not recommended as they may lead to false negatives.8
Question 2
In an acral naevus, what pattern of pigmentation might be observed on dermatoscopy?
Question 3
What is a parallel ridge pattern (PRP)?
Question 4
What is the next step if a PRP is found on examination?
Question 5
Does a PRP sign on dermatoscopy always entail an acral melanoma?
Answer 2
Dermoscopy of an acral naevus usually reveals pigmentation along the furrows of skin markings with lattice and fibrillar patterns.1−4 A fibrillar pigment pattern denotes densely packed fine pigmentation that is arranged across the parallel skin markings.4 Pigmentation that runs parallel along the furrows of the skin on hands and feet usually indicates a benign acral naevus.1,2,4
Answer 3
In acral melanoma, pigmentation is observed in the ridges, usually extending over the whole lesion as well as being irregular.2,4 As the melanoma progresses, the pigmentation intensifies and variable shades are observed, which is usually an indicator of invasive melanoma.2,4 This observation of pigmentation in the ridges is known as a ‘parallel ridge pattern’ (PRP) and is a very important dermatoscopic feature of malignant melanoma.4 PRP is very helpful in diagnosing early acral melanomas as it has a reported 86−99% specificity.3,4
Answer 4
Saida and colleagues have outlined a good algorithm for the diagnosis of acral naevi versus acral melanoma.2 All lesions demonstrating PRP should be biopsied; if no PRP is seen, then features distinguishing an acral naevi dermoscopically should be identified.2 If fibrillar or lattice features are not present on dermoscopy and the lesion is greater than 7 mm then a biopsy is warranted, otherwise periodic review of the lesion should be organised.2 If the patient has risk factors for developing skin cancer, such as being immunosuppressed, then there should be a low threshold for a biopsy.
Answer 5
Although PRP has been reported for its high specificity in diagnosing melanoma, there are other conditions in which PRP is observed.3
These include:
- Acral subcorneal haemorrhage: Caused by trauma and may display PRP on dermatoscopy.3 A helpful dermatoscopic sign that may be observed in acral subcorneal haemorrhage is ‘pebbles’ on the ridges.3
- Hyperpigmentation on the volar skin induced by anticancer drudrugs: anticancer medication, such as 5-flurouracil, may induce hyperpigmentation on acral skin, which can display PRP on dermatoscopy.3
- Acral pigmented macules associated with Peutz–Jeghers syndrome: Peutz–Jeghers is an autosomal dominant disorder, which results in small pigmented lesions displaying PRP.3 These lesions are commonly found on the lips and acral areas.3
- Pigmented plantar warts may also display PRP on exmaination.3
- Miscellaneous causes, such as pigmentation to a dye (eg paraphenylenediamine) on acral skin, can display the PRP sign.3
Taking a good history and addressing key questions that cover the range of other conditions that produce PRP on dermatoscopy can help to exclude melanoma.2,4
Conclusion
This case addresses an interesting point that PRP on dermatoscopy does not always entail melanoma and highlights other conditions in which PRP can be observed. High-risk patients, such as those who are immunosuppressed, should be examined thoroughly with a low threshold for performing biopsies on doubtful lesions. All suspicious lesions on dermatoscopy exhibiting PRP should be biopsied along with a detailed history to exclude melanoma.
Key points
-
All lesions displaying a PRP on dermatoscopy should be biopsied.
-
Generally, excisional biopsies are recommended for suspicious pigmented lesions.
Authors
Harini Rajgopal Bala MBBS, B.Pharm, MPH, Diploma in Dermatology, Skin and Cancer Foundation Inc, University of Melbourne, Carlton, Vic. hbala@skincancer.asn.au
Alvin H Chong FACD, MBBS, Skin and Cancer Foundation Inc, University of Melbourne, Carlton, Vic; St Vincent’s Hospital, Department of Dermatology, Melbourne, Vic
Competing interests: None.
Provenance and peer review: Not commissioned, externally peer reviewed.