It is well known that Australia has an ageing population. Morbidity and mortality rates increase with ageing1 and increase the burden on the healthcare system. In recent years, emergency department (ED) presentations have increased from 5.7 million in 2008–09 to 6.7 million in 2012–13,2 with older person presentations rising at a rate of 6% annually.3 Those aged 65 years or older are the fastest growing demographic,4 and those aged older than 80 years represent a disproportionately high presentation rate.5
After an ED presentation, many older people will be discharged home for follow-up care with their family doctor in general practice. Effective transition between the different modes of care is imperative, as problems with clinical handover can have a negative impact on patient safety and quality of care.6 This includes increased health risks and re-admissions7,8 in an already at-risk group for ED re-presentation.9
Various factors promote the effective discharge planning of older people as they move from acute to community care. Involvement and education of family members and/or carers, as well as effective interdisciplinary communication between healthcare professionals, including those in general practice, have been found to improve care.8 Discharge communication between EDs and general practice has long been identified as problematic.10 Absent, delayed or inaccurate communication can affect continuity of care and contribute to adverse effects.11 In one survey, almost one-third of general practitioners (GPs) reported that discharge letters were not received, or that deficiencies in the discharge information was such that the transition process was hindered.12
There is scant literature available on the general practice follow-up behaviour of older people after an ED admission. We sought to investigate this phenomenon in a suburban hospital in south-western Sydney in New South Wales, Australia.
Methods
The primary aim of this prospective, descriptive study was to measure the proportion of patients aged 65 years and older, discharged from a suburban ED, who had been given explicit general practice follow-up instructions, who then sought care in general practice by day seven after discharge. Potential contributing factors to general practice follow-up, such as social support/isolation and mobility, were also explored.
Research participants were drawn from patients attending the ED of Fairfield Hospital. Over a two-week period in July 2016, patients were advised of the study via ED waiting room posters. The ED staff distributed pamphlets at the time of discharge. Apart from informing patients that a researcher might contact them by telephone, there were no other changes to routine ED care.
Admission and discharge data were reviewed to determine patients who satisfied the inclusion and exclusion criteria. Inclusion criteria were patients who were:
- aged 65 years or older
- admitted to the ED during the recruitment weeks
- subsequently discharged directly back into the community
- sent with a discharge summary (identified in the ED electronic records system) that included explicit general practice follow-up instructions.
Exclusion criteria were patients who were admitted as inpatients to Fairfield Hospital or transferred to another public health facility prior to discharge.
Prospective participants were contacted by telephone at least seven days after their discharge from the ED and their data collected if they consented to take part in the study. Where a language barrier was encountered at the time of consent, a participant-nominated family member was consented to complete the telephone questionnaire on the participant’s behalf.
Paper forms were used to collect participant data and these were later collated into a spreadsheet. Demographic data were drawn from discharge summaries (ie age, gender, marital status, religion, language spoken at home), as well as details pertaining to the presentation (ie initial complaint, Australian Triage Scale [ATS], time of admission and length of stay, level of healthcare worker responsible for data entry, specifics of follow-up instructions). The road distances between the participants’ home address and Fairfield Hospital and listed general practice address were computed. Further data were collected during the structured telephone interview:
General practice follow-up
- Did the patient recall receiving a discharge summary when leaving the hospital?
- Did the patient present to a GP and, if so, when did they present and was this GP the discharge summary addressee?
- Had they seen a doctor other than a GP?
- Mobility
- Did they have access to a car and, if so, did they drive themselves or were they driven by someone else?
- Do they use mobility aids (eg walking stick, frame)?
Social support
The validated six-question Lubben Social Network Scale (LSNS-6), a self-reported measure of social support/isolation tool, was administered (Table 1)13 – social support is related to health-seeking decisions, and close networks associated with a reduced likelihood of attending EDs unnecessarily.14
Table 1 – Lubben Social Network Scale (LSNS-6)13
|
Family: Considering the people to whom you are related by birth, marriage, adoption, etc
|
|---|
- How many relatives do you see or hear from at least once a month?
- How many relatives do you feel at ease with that you can talk about private matters?
- How many relatives do you feel close to such that you could call on them for help?
|
|
Friendships: Considering all of your friends, including those who live in your neighbourhood
|
|---|
- How many of your friends do you see or hear from at least once a month?
- How many friends do you feel at ease with that you can talk about private matters?
- How many friends do you feel close to such that you could call on them for help?
|
|
Scoring: 0, none; 1, one; 2, two; 3, three or four; 4, five to eight; 5, nine or more
|
|---|
Analyses
Data were analysed using Microsoft Excel and IBM SPSS 23. Participants’ demographics were analysed using descriptive statistics. The data were further explored using independent samples t-test, Mann-Whitney U test and chi-squared test, to examine the effect of continuous, ordinal, and categorical variables respectively, on seven-day general practice follow up. These exploratory analyses were used to identify potential explanatory factors and further hypotheses.
Ethics approval
Ethical approval for the study was obtained from the South Western Sydney Local Health District’s Research and Ethics Office (reference number: HE16/066 LNR).
Results
Patient population
A total of 70 people satisfied the inclusion criteria. They were contacted via telephone at least seven days after their ED discharge date for possible participation. Of these, 17 could not be contacted by telephone and three were unable to participate because of difficulties with language, leaving 50 participants who were included in the study.
Participant demographics
The majority of the 50 participants were women (60%) and married (74%), with a mean age of 75.3 years. English was the most common individual language spoken, although more than half of the participants (58%) used another language as their primary language – Assyrian, Italian, Arabic, and Spanish in order of frequency. One-fifth of telephone questionnaires were conducted with a nominated family member.
Most participants were either ATS 3 (36%) or ATS 4 (54%), and generally presented during the day between 6.00 am and 6.00 pm (72%). On the LSNS-6, 20% of participants were scored as ‘socially isolated’, defined as a score of less than 12.13 The mean self-reported satisfaction rating for the ED visit was high (8.2/10; Table 2).
General practice follow-up by day seven after ED discharge
Most participants (76%) attended a general practice by day seven after discharge; day three was the median follow-up day (Figure 1). Of those participants, 18% consulted a GP who was not the addressee in the discharge summary. Almost all participants stated that they received a printed discharge summary on leaving the Fairfield Hospital ED (96%).
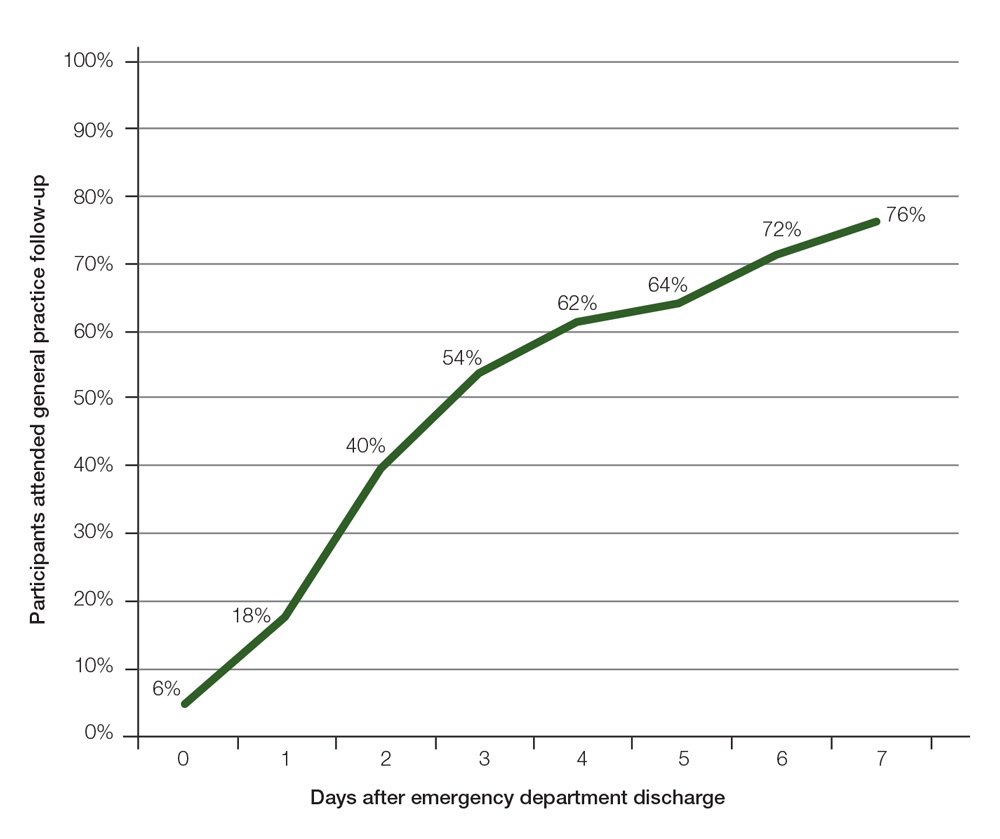
Figure 1. Cumulative proportion of study participants who attended general practice follow up after emergency department discharge (days 0–7)
General practice follow-up by day seven – Exploratory analyses
The most statistically significant effect found associated with seven-day general practice follow-up was to Question 3 in the LSNS-6: ‘How many relatives do you feel close to such that you can call on them for help?’ (Table 3). Participants who
attended general practice follow-up by day seven reported a higher score (more relatives that can be called on to help) on this item (P = 0.003).
The participants in this study who had not seen a GP by day seven after discharge seemed more likely to have been female, unmarried/widowed, did not drive, took more regular medications and spent longer in the ED (Table 3).
Discussion
This project measured the proportion of older patients with explicit general practice follow-up instructions who sought care by day seven after ED discharge. While larger studies have addressed why these presentations initially occur,14 we believe that this is the first study of its kind to specifically quantify general practice follow-up behaviour of older people.
In our study, most older patients consulted with a GP in a timely manner. A small number consulted a GP on the day of discharge, a fifth by the next day, and half by day three. This is encouraging from the perspective of continuity of care, and identifies the imperative of discharge summary availability.
Almost all participants in this study stated they were supplied with a printed copy of their discharge summary. Earlier Australian research identified that GPs only receive a quarter of discharge summaries for older people when they were given to patients for hand delivery.15 Direct transmission (eg secure messaging, facsimile) increases the proportion of discharge summaries received.15 However, this study demonstrates a potential upper boundary to the effectiveness of that strategy – a fifth of our participants saw a GP who was not the nominal addressee of the discharge summary.
This finding suggests that any single method of hospital discharge communication is unlikely to be effective. Importantly, where clinical transitions have been suboptimally managed, preventable hospital visits, and even increases in mortality, can occur.16 Looking forward, routinely uploading discharge summaries into the online ‘My Health Record’ (formerly the Australian ‘Personally Controlled Electronic Health Record’) may be the long-term communication solution, assuming there is near universal uptake by the Australian community and health providers. In the present day, however, EDs may need to continue transmitting discharge summaries using multiple methods.
The exploratory analyses conducted were designed to identify potential explanations of the results. Some intriguing associations identified include those between gender, marital and driving status, and general practice follow-up. In this study, women were less likely to be married (more likely to have been widowed), and less likely to drive. Those who were not married and did not drive were less likely to attend for follow-up with their GP. Not surprisingly in this context, the women observed in this study were less likely to attend for follow-up. Transportation barriers are more likely to affect women than men.17 This is a potential identifiable at-risk population regarding their ability to access care, and further research seems warranted.
Another association worthy of further investigation involves individuals who may have been more ill. Worryingly, participants who took a larger number of regular medications and had a longer ED admission were seemingly less likely to have attended general practice follow-up by day seven.
Social isolation as measured by the LSNS-6 score did not seem to be associated with general practice follow-up. Curiously, one question seemed especially important, ‘How many relatives do you feel close to such that you can call on them for help?’, where a low score is associated with a lower likelihood of general practice follow-up. Others have found that social isolation per se may not affect general practice use;18 however, early and active family involvement in discharge planning can assist frail, older patients in the successful transfer from hospital to community care.8 This finding may reflect familial involvement in the discharge process, especially given the acute setting, and the cultural context in which the study took place, with most participants from non–English speaking backgrounds.
Table 2. Participant demographics
|
Total number of participants = 50
|
|
|
General demographics
|
|
|
Sex
|
n (%)
|
|
Male
|
20 (40.0)
|
|
Female
|
30 (60.0)
|
|
Age, years 75.3 (65.0–91.0; 7.7)*
|
|
|
Marital status
|
n (%)
|
|
Yes
|
37 (74.0)
|
|
No or widowed
|
13 (26.0)
|
|
English primary language
|
n (%)
|
|
Yes
|
21 (42.0)
|
|
No
|
29 (58.0)
|
|
Questionnaire conducted with a family member
|
n (%)
|
|
Yes
|
10 (20.0)
|
|
No
|
40 (80.0)
|
|
Number regular medications
|
4.7 (3.1)†
|
|
ED presentation
|
|
|
Australian Triage Scale
|
n (%)
|
|
1
|
0 (0.0)
|
|
2
|
3 (6.0)
|
|
3
|
18 (36.0)
|
|
4
|
27 (54.0)
|
|
5
|
2 (4.0)
|
|
Time in minutes spent in ED
|
214 (98)†
|
|
ED satisfaction rating‡
|
8.2 (1.7)†
|
|
Kilometres from home to ED
|
4.8 (4.3)†
|
|
Kilometres from home to GP
|
3.8 (3.3)†
|
|
Mobility and transport
|
|
|
Uses aid§
|
n (%)
|
|
Yes
|
23 (46.0)
|
|
No
|
27 (54.0)
|
|
Drives a car
|
n (%)
|
|
Yes
|
29 (58.0)
|
|
No
|
21 (42.0)
|
|
Owns a car
|
n (%)
|
|
Yes
|
27 (54.0)
|
|
No
|
23 (46.0)
|
|
Access to a driver
|
n (%)
|
|
Yes
|
48 (96.0)
|
|
No
|
2 (4.0)
|
|
Social isolation
|
|
|
LSNS-6 score
|
|
|
Median (range)
|
15 (7–28)
|
|
Interquartile range
|
9
|
|
Socially isolatedǁ, n (%)
|
10 (20)
|
|
*Mean (range; SD); †mean (SD); ‡score out of 10;
- walking stick, frame or wheelchair; ǁscore <12
ED, emergency department; GP, general practitioner; LSNS-6, Lubben-6 Social Network Scale
|
Strengths and limitations
The main strengths of this study lie in its design. Being prospective in nature, we attempted to recruit all eligible participants over the recruitment period, and the majority of eligible participants (50/70) were included. As data were collected directly from participants or participant‑nominated family members, we are confident of the accuracy of the primary outcome (proportion of people who attended follow-up with their GP).
There are limitations associated with this small study. It was conducted at a single location in an ethnically diverse area of Sydney. It is possible that this is a unique study population that may not reflect broader Australia. Extrapolation of the seven-day general practice follow-up finding to other sites should be made cautiously. Language difficulties were also encountered. Interviews were sometimes conducted with a nominated family member, translating or answering on the participant’s behalf. Use of formal health translators would have been preferable, but this resource was not available. This introduces a source of bias, particularly in the LSNS-6, where the questions are somewhat subjective.
Importantly, the explanatory analyses were designed to be exploratory in nature and should only be seen as hypothesis-generating, given the small study numbers and low statistical power. A limitation of structured questionnaires with forced-choice options is that we cannot be certain about how participants interpreted some questions or the reasons that underlie the responses. Further investigation on this topic could involve replicating the project at more sites. Qualitative research of participants’ perspectives may illuminate the barriers and facilitators to general practice follow up after an ED visit.
Table 3. Associations between general practice follow-up and other factors
|
Participant characteristics
|
General practice follow-up by day seven after discharge
|
Significance*
|
|
|
|---|
|
|
|
Yes
|
No
|
|
|
Sex
|
Male (%)
|
90
|
10
|
P = 0.091†
|
|
|
Female (%)
|
67
|
33
|
|
Age
|
Mean years (SD)
|
74.3 (7.0)
|
78.3 (9.0)
|
P = 0.176‡
|
|
Married or regular partner
|
Yes (%)
|
84
|
16
|
P = 0.055†
|
|
No (%)
|
54
|
46
|
|
English primary language
|
Yes (%)
|
86
|
14
|
P = 0.311†
|
|
No (%)
|
71
|
29
|
|
Number of regular medications
|
Mean (SD)
|
4.1 (3.1)
|
6.4 (2.3)
|
P = 0.02‡
|
|
Australian Triage Scale
|
1 (%)
|
0
|
0
|
P = 0.484§
|
|
2
|
3
|
17
|
|
3
|
37
|
33
|
|
4
|
58
|
42
|
|
5
|
3
|
8
|
|
Length of ED admission
|
Mean minutes (SD)
|
201 (100)
|
256 (85)
|
P = 0.076‡
|
|
ED satisfaction rating
|
Mean (SD) out of 10
|
7.9 (1.8)
|
9.0 (1.1)
|
P = 0.018‡
|
|
Road distance from home to ED
|
Mean (SD) in km
|
4.6 (3.9)
|
5.1 (5.6)
|
P = 0.785‡
|
|
Road distance from home to GP
|
Mean (SD) in km
|
3.4 (3.0)
|
5.0 (4.2)
|
P = 0.276‡
|
|
Uses mobility aid
|
Yes (%)
|
70
|
30
|
P = 0.508†
|
|
No (%)
|
81
|
19
|
|
Drives a car
|
Yes (%)
|
90
|
10
|
P = 0.051†
|
|
No (%)
|
66
|
34
|
|
Owns a car
|
Yes (%)
|
85
|
15
|
P = 0.183†
|
|
No (%)
|
65
|
35
|
|
Access to a driver
|
Yes (%)
|
97
|
3
|
P = 0.426†
|
|
No (%)
|
92
|
8
|
|
LSNS-6 scoreǁ
|
Median (interquatile range)
|
17 (8)
|
13 (4)
|
P = 0.108§
|
|
Socially isolatedǁ
|
Yes (%)
|
80
|
20
|
P = 1.00†
|
|
No (%)
|
75
|
25
|
|
Question 3 on Lubben Social Network Scale (Scale 0–5)#
|
Median response
|
4
|
2.5
|
P = 0.003§
|
|
*The test is between the participants who did and did not attend GP follow-up; †Pearson chi-square (exact significance) test, two-sided. ‡Independent samples t-test, equal variance not assumed, two-tailed; §Independent samples Mann–Whitney U-test, 2-sided. ǁLubben Social Network Scale – score <12 is defined as ‘socially isolated’; #’How many relatives do you feel close to such that you can call on them for help?’; scoring: 0, none; 1, one; 2, two; 3, three or four; 4, five to eight; 5, nine or more; ED, emergency department; GP general practitioner; SD, standard deviation
|
Implications for general practice
After an ED admission, it is possible that most older people follow up with their GP within days. Discharge summaries optimally need to be available at the time of discharge.
Some older people follow up with a GP who is not the addressee of the discharge summary. To assist in adequate clinical handover, discharge summaries may need to be communicated in a variety of methods including automating upload from ED to the national online My Health Record.
The absence of close family relationships and the lack of car transport may be barriers to general practice follow up after an ED admission.
Authors
Belinda Watson BSc(Med) (Hons), MD (candidate), School of Public Health and Community Medicine, UNSW Sydney, NSW
Chun Wah Michael Tam BSc(Med), MBBS, MMH (GP), FRACGP, Staff Specialist, General Practice Unit, South Western Sydney Local Health District & Ingham Institute of Applied Medical Research, Sydney, NSW; and Conjoint Senior Lecturer, UNSW Sydney, NSW. m.tam@unsw.edu.au
Belinda Pellizzon DASc (Nursing), GradDipCritCare(Emergency Nursing), DipPM, Nursing Unit Manager, Emergency Department, Fairfield Hospital, South Western Sydney Local Health District, Prairiewood, NSW
Lucille Ban MBBS, Deputy Director, Emergency Department, Fairfield Hospital, South Western Sydney Local Health District, Prairiewood, NSW
Harry Doan MBBS, Director of Medical Services, Fairfield Hospital, South Western Sydney Local Health District, Prairiewood, NSW
Competing interests: None.
Provenance and peer review: Not commissioned, externally peer reviewed.
Acknowledgements
The researchers would like to acknowledge the assistance of the medical, nursing and administrative staff of the Fairfield ED and General Practice Unit in making this research project possible. They would also like to acknowledge the patients and family members who willingly gave their time and participated in the study. We thank Dr Andrew Knight for his comments on the drafts. Lastly, they would like to thank GP Synergy Ltd for providing a medical student scholarship and the opportunity to conduct this research.
Figure 1. Cumulative proportion of study participants who attended general practice follow up after emergency department discharge (days 0–7)