Mrs MG, 78 years of age, had a squamous cell carcinoma (SCC) excised from the dorsum of her left hand. However, the skin was too fragile to suture with simple, interrupted sutures as the skin tore easily (Figure 1).
 |
| Figure 1. Dorsal left hand following excision |
Question 1
What are the causes of fragile skin?
Question 2
What changes occur in the skin as people age?
Question 3
What conservative option is available when managing this wound? What are the potential problems?
Question 4
What surgical options are available in the management of this wound?
Answer 1
The main causes of fragile skin are ageing and sun damage. However, other causes, such as medications (eg steroids, immunosuppressants, oral retinoids), rheumatoid disease, poor nutrition and rare conditions (eg epidermolysis bullosa, Ehlers-Danlos syndrome, prolidase deficiency, osteogenesis imperfecta), should be kept in mind.1
Answer 2
Many significant structural and functional changes occur within the skin tissue during ageing. These include:2,3
- impaired cell growth, turnover and repair
- epidermal atrophy (cellular turnover slowing to around 50%)
- dermal atrophy (a thickness loss of around 20%)
- decreased collagen content (decreasing by around 1% per year through adult life)
- decreased efficacy of skin functions (eg thermoregulation, secretion), some by as much as 50–60%
- reduction in vascular supply
- decreased immune response
- decreased vitamin D synthesis
- impaired barrier function.
The skin becomes more fragile and prone to tearing as a result of significant epidermal and dermal atrophy, and decreased collagen content. Reduced vascular supply, cellular turnover and immunity also contribute to slower healing.
Answer 3
The wound may be managed conservatively by allowing healing through secondary intention. This is by far the simplest approach, but it has various potential problems that must be considered:4
- Healing may take several weeks to months.
- Dressings may be difficult for the patient to manage and keep in place, and may be expensive.
- The wound may be painful until healing occurs.
- There is a greater tendency for normal, hypertrophic and keloid scarring, tissue contracture, and an unstable scar (which is prone to constant break down).
- Healing by secondary intention should be avoided if the wound contains important structures such as tendons, which are prone to infection and damage.
Answer 4
There are several methods in the surgical management of this wound:
- Fragile skin excision defects are most commonly encountered on the lower leg. These may be repaired by split skin graft. However, the procedure requires training and experience, creates a secondary wound at the site of skin harvesting, is time consuming, and usually requires hospital admission.
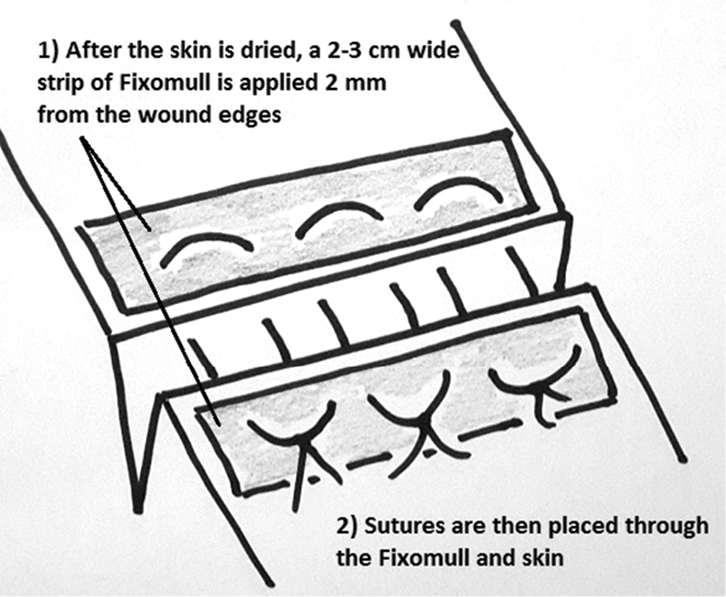
- Suturing fragile skin can be assisted by applying adhesive strips or tape (eg Steri-Strips or Fixomull)5,1 on either side of the wound (adjacent to and parallel to the wound edges) and then suturing through the tape and skin with simple or horizontal mattress sutures (Figure 2). The tape can be removed at the time of suture removal with the aid of a solvent or simple vegetable oil.
- In this case, a horizontal mattress suture with bolsters at either end was used to help repair the wound. This is described below in detail.
Methods 2 and 3 are considered mechanical and are similar. Method 2 is more suitable if the entire skin edge requires support from damage caused by sutures. Method 3 is more suitable if only 1–2 suture(s) are required to oppose the wound edges, allowing completion of wound closure with simple suturing.
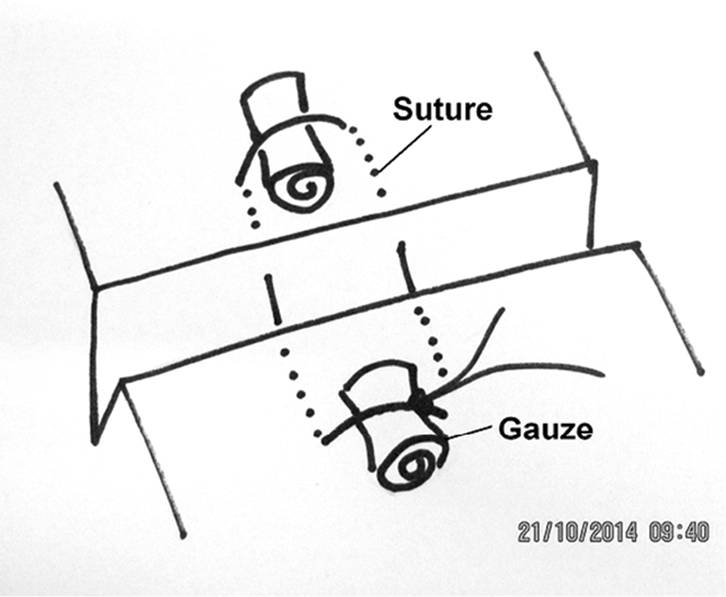
Using horizontal mattress sutures with bolsters inserted to help protect the skin is a simple and effective way to suture fragile skin (Figure 3).
The horizontal mattress suture reduces the risk of tearing as it distributes the force on the skin over a broad area. This type of suture also assists in everting thin and fragile skin edges, which have a tendency to invert with simple interrupted sutures. The skin may be further protected by placing padding, such as rolled up impregnated gauze (eg Cuticerin), beneath the loops of the suture (Figure 4).6 Substantial force can then be applied to the skin without tearing it (Figure 5). The wound can then be closed with simple suturing under little or no tension (Figure 6).
The horizontal mattress suture can be removed 3–4 days after the procedure to prevent pressure necrosis beneath the bolster if the skin is overly fragile, or if the suture is under excessive tension. The rest of the sutures are then removed around 10 days after the procedure. The practitioner must be made aware of any early signs of infection and wound breakdown, given the fragile nature of the skin and the potential for poor healing. These potential problems should be adequately communicated to the patient. It is prudent to review the patient 2 days post-operatively, at which stage the dressing can be removed and the wound reviewed for complications. Figure 7 shows the wound at 11 days post-operative, just after the sutures were removed.
 |
 |
 |
| Figure 2. Steri-strips applied to assist wound closure |
Figure 3. Horizontal mattress suture supported by bolsters |
Figure 4. Horizontal mattress suture with bolsters in place |
 |
 |
 |
| Figure 5. Wound closed without tearing by tightening the central suture |
Figure 6. Final wound closure using a simple continuous suture |
Figure 7. Wound 11 days post-operative, just after suture removal |
Summary
Fragile skin can be difficult to repair due to tearing. Horizontal mattress sutures with bolsters placed at either side can prevent skin tearing and allow effective wound closure.
Author
Steven Tomas MBBS (Hons), MMed, Clinical Lecturer, University of Sydney; and GP, Gumtree Medical Practice, Dubbo, NSW
Competing interests: None.
Provenance and peer review: Not commissioned, externally peer reviewed.