Cerumen impaction (also known as ear wax) is a common presentation to a general practitioner (GP). Ear syringing is often the treatment of choice, and most GPs see a minimum of two patients per week for ear syringing.1 It is considered by most to be effective and safe. However, 1 in 1000 patients experience major complications following syringing.1 As a consequence, one in five medico-legal cases involving GPs are related to ear syringing.1
This article will discuss the composition of ear wax, why it accumulates, treatment options and potential complications, to assist GPs in safely managing this condition.
Ear anatomy
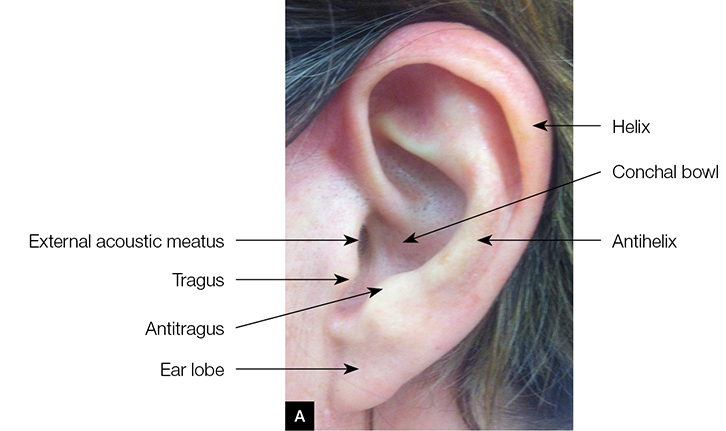
A knowledge and understanding of normal ear anatomy is essential in the correct management of impacted cerumen with the use of ear syringing. The following is a brief review of the external ear and tympanic membrane anatomy.
The external ear consists of the pinna, ear lobe, conchal bowl and external acoustic meatus (Figure 1A). The blood supply is from branches of the external carotid artery. Innervation of the ear is from multiple nerves including the cervical plexus, trigeminal nerve (CNV), facial nerve (CNVII), glossopharyngeal (CNIX) and vagus nerves (CNX). Side effects of ear syringing, which will be discussed later in this article, involve many of these nerves.
The tympanic membrane faces downwards and laterally (Figure 1B).
The external auditory canal (EAC) curvature is different in adult and paediatric patients. To visualise the EAC and tympanic membrane in the adult, the pinna should be gently pulled upwards and backwards. In paediatric patients, the pinna should be pulled downwards and backwards.
 |
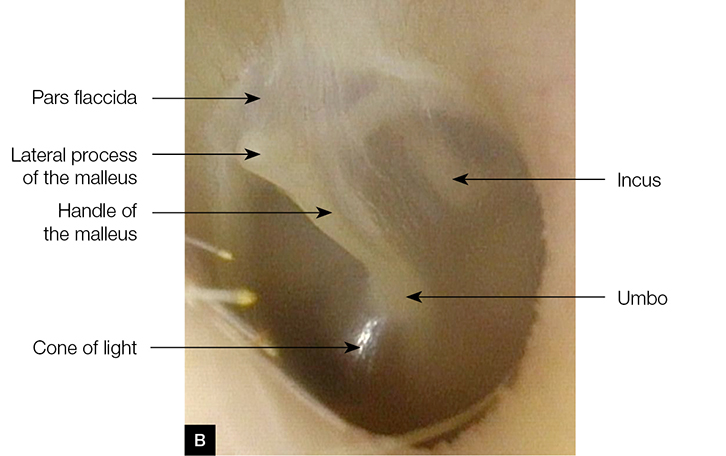 |
Figure 1. Ear anatomy
A. External ear
B. Left tympanic membrane |
What is ear wax?
Ear wax is the product of ceruminous and sebaceous gland secretions, mixed with exfoliated squamous epithelium. It forms a protective film, has antibacterial properties and provides lubrication to the ear canal. It is the ear’s self-cleaning mechanism, and traps dust and dirt, which are then excreted from the ear canal in a medial to lateral direction. This is aided by epithelial migration and movement of the jaw.2,3
Why does ear wax accumulate?
When the self-cleaning mechanism is disrupted, wax accumulates and can become impacted. Narrowing or obstruction of the ear canal, due to anatomical variations or infectious or dermatological diseases, can interfere with the normal migratory process.4
Irritation from foreign objects placed in the ear (eg cotton tips, hearing aids and ear plugs) can cause chronic changes to the skin of the ear canal and impair normal epithelial migration. Cotton buds also tend to push cerumen deeper into the ear canal, and hearing aids and ear plugs obstruct the ear canal and contribute to cerumen accumulation over time.4 Furthermore, the ceruminous glands atrophy with age and produce a drier wax that migrates more slowly.5 Cerumen impaction is present in up to 57% of older patients, compared with 5% of younger, healthy adults.6
Indications for treatment
Cerumen accumulation is normal and does not require treatment unless it is symptomatic. Wax is usually described as impacted if it obscures visualisation of the tympanic membrane and is associated with symptoms.7 Common symptoms include conductive hearing loss, ear pain, itching or fullness, dizziness, tinnitus or reflex cough.8 Consensus is that symptomatic cerumen generally warrants removal,9 although, notably, in up to one-third of cases, the cerumen will clear within five days without treatment.10 Removal is also often indicated to allow view of the tympanic membrane for diagnostic purposes or to allow audiometry.
Treatment options
The first-line option for treatment of symptomatic patients is cerumenolytics. The use of cerumenolytic agents, namely eardrops such as docusate sodium, increases the likelihood of cerumen clearance, compared with no treatment.10 However, there is no significant difference in effectiveness between water-based or oil-based drops.2,10 Patients should be discouraged from using cotton buds in the canal for cleaning. There is a very limited role for the use of cotton buds on the outer ear only. Patients with hard impaction or ear canal disease may require irrigation or manual removal under microscope by a trained doctor or an ear, nose and throat (ENT) specialist. The use of a cerumenolytic will improve success of subsequent irrigation.2,11
How to safely syringe ear wax
Irrigation, or ear syringing, should be performed only after taking a full history, doing an ear examination and explaining the potential complications to the patient. It is also important to ensure appropriate assembly and use of equipment.12
Gentle irrigation of the ear canal can be performed with a large syringe (20 mL) and warm water. The use of sterile water or saline as opposed to tap water or bacteriostatic agent (eg dilute hydrogen peroxide) can decrease the risk of infection.9
Direct visualisation of the ear canal is not necessary for safe and effective syringing. The tip of the syringe should not pass the outer one-third of the ear canal (approximately 8 mm)9 – the use of a rounded nozzle may assist with this. The jet of water should be aimed towards the edge of the cerumen to enable the debris to flow out of the ear canal. Cease immediately if the patient experiences pain or if bleeding occurs. Mechanical jet irrigators are available and some allow better control of water pressure and direction of spray (Figure 2). After syringing, examine the external canal and tympanic membrane. Document the patient’s consent, procedure, and pre- and post-examination findings.
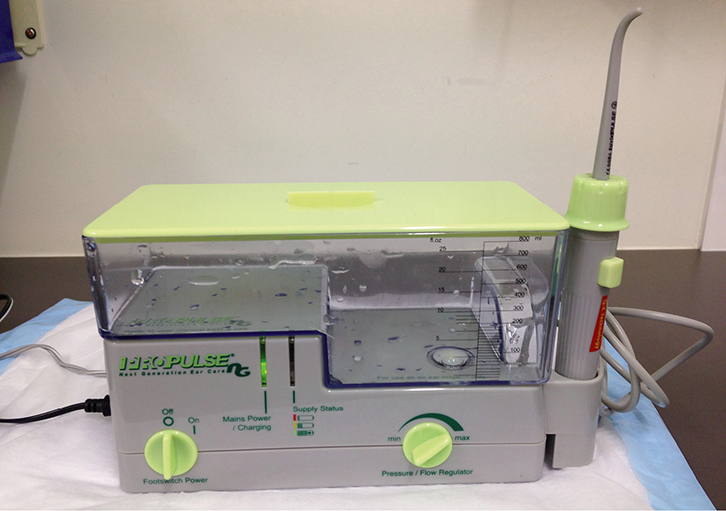 |
| Figure 2. Mechanical jet ear irrigation system |
Contraindications
Ear syringing is contraindicated if there are any signs or symptoms of current otitis externa or otitis media, past or present tympanic membrane perforation, history of ear surgery or unilateral deafness.12 In a patient whose hearing is impaired, the only, or better, hearing ear should not be syringed. Avoid syringing uncooperative patients (eg children). Caution should also be taken if there is a history of recurrent otitis externa or tinnitus, as syringing may aggravate these conditions.12 Care should also be taken with patients who are immunocompromised and at increased risk of infection.9
Side effects and complications
Syringing can damage the delicate skin of the ear canal and the tympanic membrane itself. Irritation to nerves can sometimes lead to severe, although temporary, side effects. Patients can often cough during the procedure (CNIX and X) and can experience significant tinnitus or vertigo. Much less common but clinically significant complications (eg tympanic membrane perforation or EAC trauma) can also occur. Syringing also predisposes patients to infections, namely otitis media and otitis externa,6 and retention of water behind incompletely removed cerumen increases the risk.2
In the majority of cases, traumatic tympanic membrane perforations will heal without any treatment. Perforations can often become infected and may be safely treated with ciprofloxacin-based topical drops. Patients may need audiology and consideration of referral to an ENT specialist if there is concern regarding hearing.
Other options for mechanical removal
Other options for mechanical removal include microsuction, with or without curettage, under microscope. Unfortunately, this is usually only available in dedicated ENT outpatient clinics. Microsuctioning is generally well tolerated, safe and efficacious.13 It also has the advantage of not exposing the ear to moisture and thus has fewer contraindications and is associated with a lower frequency of infections.9 Discomfort due to noise is the greatest complaint. However, there is no clinical evidence that this affects hearing.14
When to refer?
Referral to an ENT specialist is rarely needed for cerumen management alone. Referrals should be made in the following situations:
- pain or bleeding on syringing
- failure to remove cerumen after multiple attempts of syringing, preceded by wax-softening drops
- persistence of symptoms despite successful removal of cerumen
- chronic cerumen impaction
- contraindications, especially perforated tympanic membrane, prior ear surgery or cerumen impaction in the only or better hearing ear
- abnormal tissue in the ear canal
- any other concerns.
Key points
- Patients should be educated about the ear’s self-cleaning mechanism and discouraged from using anything to remove wax from the ear canal.
- Patients should first be encouraged to use eardrops to soften wax and facilitate self-cleaning for symptomatic wax accumulation.
- Ear syringing can be performed by trained staff if first-line treatment fails.
- Patients should be referred for specialist ENT assessment if there are any contraindications to syringing, syringing fails to remove wax or resolve symptoms, or for any other concerns.
Authors
Skye Poulton BHlthSc (Nutr), MBBS, Junior House Officer, Ipswich Hospital, Ipswich, QLD. skyepoulton@hotmail.com
Stephanie Yau MBBS, ENT Principal House Officer, Townsville Hospital, QLD
Daniel Anderson BAppSc (EXSS), MSpMed, MBBS, ENT Registrar, Ipswich Hospital, Ipswich, QLD
Daniel Bennett MBBS FRACS, ENT Consultant, Ipswich Hospital, Ipswich, QLD
Competing interests: None.
Provenance and peer review: Not commissioned, externally peer reviewed.