Case study
A young man presents with a tumour of the skin on the volar side of the distal phalanx of his right ring finger. One month ago, he punctured a blister filled with blood, which was caused by a superficial burn. The tumour has since been growing rather rapidly. The man reported that it was not painful.
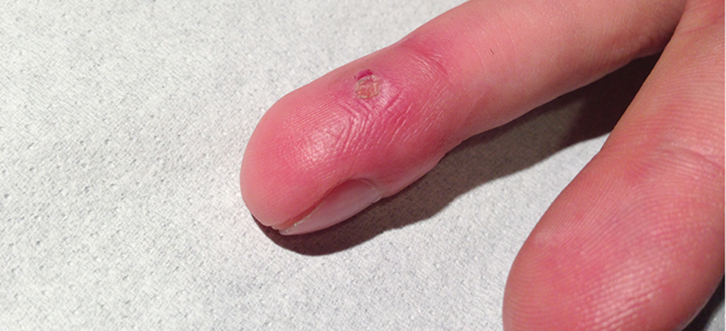
Examination revealed a red-purple, tinted glistening tumour with a diameter of approximately 6 mm (Figure 1).
 |
| Figure 1. A red-purple tumour on the volar side of the distal phalanx of the right ring finger |
Question 1
What is the most likely diagnosis?
Question 2
What are the differential diagnoses?
Question 3
What is the aetiology of this condition?
Question 4
How is it diagnosed?
Question 5
What is the appropriate management of this condition?
Answer 1
The most likely diagnosis is pyogenic granuloma, also known as granuloma telangiecticum. This is a common, benign vascular proliferation that occurs on the mucosa and skin. Patients usually present with a painless, smooth, red-purple sessile or pedunculated lesion. The lesion has a history of rapid growth, mostly within some weeks, and bleeds easily. Predilection sites are the head and neck area, and the upper limb, especially the fingers.1,2
Answer 2
Differential diagnoses of a pyogenic granuloma of the skin include haemangioma, Spitz naevus, basal cell carcinoma, non-pigmented melanoma, Kaposi sarcoma and skin metastasis.3
Answer 3
The precise aetiology of pyogenic granuloma is unknown. It develops more frequently during pregnancy and within pre-existing vascular lesions (eg trauma or insect bites), which suggests a role for angiogenic factors and hormonal stimuli.4 Isotretinoin therapy may predispose to pyogenic granuloma.5 However, the majority of patients with pyogenic granuloma have no predisposing factors.6
Answer 4
Most pyogenic granulomas are of textbook appearance. Experienced doctors may diagnose this condition at a glance, particularly in combination with a history of a fast-growing lesion after trauma.
Answer 5
A systematic review summarised the evidence on treatment modalities for pyogenic granuloma.1 This review included 34 observational studies on 1162 cases of pyogenic granulomas that were treated with 19 different modalities. The number of patients varied from a few patients in case reports to large retrospective studies that consisted of 408 patients. The age of the patients ranged from 3 months to 90 years, and the follow-up time varied from 3 weeks to 18 months. The majority (65%) of lesions were treated surgically. This included surgical excision (44%) or by curettage or shave excision with or without cautery, or cautery alone (17%). These treatments were found to be effective and recurrence rates were low. Recurrences were found to have occurred more frequently after curettage or shave excision (10%) when compared to surgical excision (3%). The most commonly applied non-surgical treatment modalities were cryotherapy with liquid nitrogen (16%), CO2 laser ablation (9%) and pulsed dye laser therapy (6%). More than one treatment session is often needed with cryotherapy and pulsed dye laser therapy.6–9 Recurrence rates of these non-surgical treatment options were comparable with those after surgical excision. The experience with other non-surgical treatment options (eg applying imiquimod or sclerotherapy) is very limited. The same applies to topical treatment with timolol, about which some case reports were published recently.10–12 In four pyogenic granulomas, watchful waiting showed that these granulomas spontaneously regressed within 6–18 months.1,2
In conclusion, surgical excision is considered first-line treatment because of its effectiveness and low recurrence rates. The other advantage of surgical treatment is the opportunity to send the lesion for histopathological analysis. Non-surgical treatment with cryotherapy or laser therapy may be options for lesions on cosmetically sensitive areas and may be the preference of some patients. The option of watchful waiting should also be discussed with the patient.
Case study follow-up
The tumour was removed by curettage with cautery. A digital nerve block anaesthesia was given and the procedure was performed in a bloodless field. This is recommended as pyogenic granuloma tends to bleed profusely. Histopathological examination confirmed the clinical diagnosis of pyogenic granuloma. Figure 2 shows the lesion 4 weeks after treatment.
 |
| Figure 2. The same finger 4 weeks after treatment with curettage and cautery |
Authors
Zamire Damen-van Beek MD, general practitioner, Dutch College of General Practitioners, Utrecht, The Netherlands. z.damen@nhg.org
Wim Opstelten MD, PhD, general practitioner, Dutch College of General Practitioners, Utrecht, The Netherlands
|
Competing interests: None.
Provenance and peer review: Not commissioned, externally peer reviewed.