Case study
A healthy woman, 29 years of age, presented with a 10-month history of asymptomatic, progressively enlarging ‘bumps’ on her fingers. Physical examination revealed the presence of well-defined, flat-topped, slightly erythematous nodules, symmetrically located over the extensor surface of the second and third proximal interphalangeal (PIP) joints of both hands (Figure 1), and the PIP joint of her fourth right-hand finger (Figure 2). There was no history of previous local injuries and the symptoms were not suggestive of underlying articular disease. There was no family history of similar lesions.
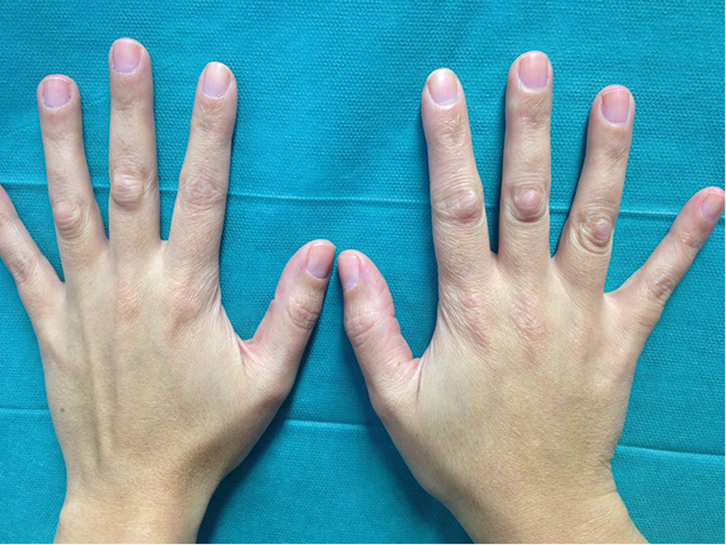 |
| Figure 1. Bilateral and symmetrical subcutaneous nodules on the knuckles of an otherwise healthy young woman |
|
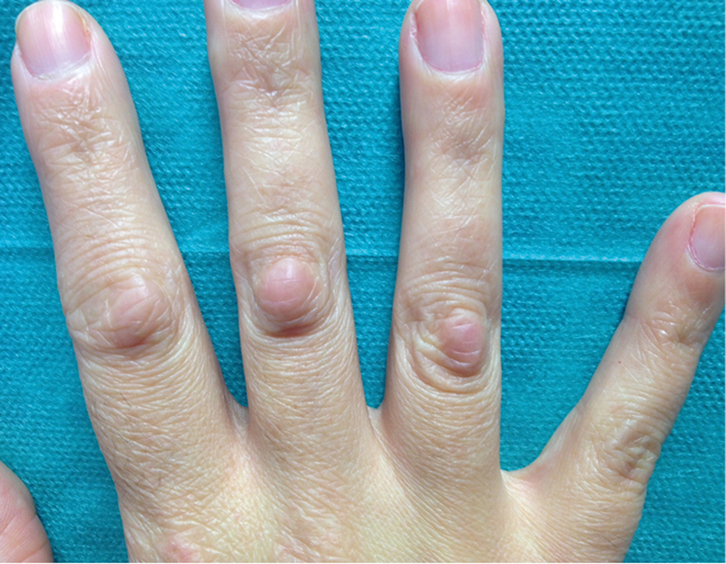 |
| Figure 2. Clinical detail of cutaneous lesions showing round-shaped pinkish subcutaneous nodules overlying the extensor surface of proximal interphalangeal joints from second to fourth right-hand fingers |
|
Question 1
What is the most likely diagnosis?
Question 2
How could you confirm this diagnosis?
Question 3
What are the most common disorders related to this diagnosis?
Question 4
What is the differential diagnosis?
Question 5
What is the most appropriate management?
Answer 1
Given the patient’s history and clinical findings, the diagnosis of idiopathic knuckle pads was made. Originally described by Garrod more than 100 years ago, this entity has subsequently received minimal attention in the dermatology literature and often remains a challenging diagnosis in daily practice.1 Knuckle pads (also known as helodermia, keratosis supracapitularis, pulvinus and subcutaneous fibroma) are a benign cutaneous disorder characterised by the progressive appearance of solitary or multiple thickened, callous-like, skin-coloured or slightly rosy papules and nodules overlying the metacarpophalangeal, distal interphalangeal and, more commonly, (PIP) joints.2 Hyperpigmented and hypopigmented variants have also been reported, especially among darker skin types.3 The pads may range from a few millimetres to several centimetres in diameter, and are often asymptomatic. Although available data on knuckle pads are scarce, it is often an inherited autosomal dominant trait that usually develops in teenage years and tends to persist throughout adulthood. In the largest epidemiological study to date, Paller et al found that this condition affected about 9% of almost 1900 people evaluated in Norway.4
Answer 2
Diagnosis of knuckle pads is mainly based on the morphological features of clinical lesions.1–5 A skin biopsy may also be performed in cases of atypical presentations, and to differentiate them from other similar-looking dermatoses. Histological examination usually shows hyperkeratosis and acanthosis, along with a dense noncicatricial dermal proliferation of fibroblasts within loose bands of collagen.6 Spindle-shaped fibroblasts, seen by electron microscopy, are considered distinctive.3 Occasionally, musculoskeletal ultrasonography may be necessary to exclude underlying synovial proliferation.7
Answer 3
Although most cases of knuckle pads have an idiopathic origin, several dermatological and systemic disorders have been associated with this disease.2,3,8,9 Therefore, once the diagnosis is established, physicians should consider an additional clinical assessment of the following entities (Table 1).
Table 1. Conditions associated with knuckle pads
|
|
Fibrosing conditions
|
Peyronie´s disease
Ledderhose disease
Dupuytren´s contracture
|
|
Fibromatosis
|
Pachydermodactyly
|
|
Genetic disorders
|
Bart-Pumphrey syndrome
Acrokeratoelastoidosis costa
Keratoderma hereditaria mutilans
Pseudoxanthoma elasticum
|
|
Other
|
Seborrhoeic dermatitis
Clubbed fingers
Oral leukoplakia
Glossitis
Avitaminosis A
Oesophageal cancer
Phenytoin treatment
|
The majority of knuckle-pad-related dermatoses are fibrosing conditions, including:10–14
- Peyronie’s disease – thickening of the tunica albuginea
- Ledderhose disease – thickening of the plantar aponeurosis
- Dupuytren’s contracture – thickening of the palmar aponeurosis, which remains the strongest association.
An increased familial predisposition to knuckle pads has been observed in other fibromatosis and genetic disorders, including:15-–17
- pachydermodactyly – fibromatosis of the radial and ulnar regions of the proximal interphalangeal joints of the hand fingers
- Bart-Pumphrey syndrome – leukonychia, palmoplantar keratoderma and deafness
- acrokeratoelastoidosis costa
- keratoderma hereditaria mutilans
- pseudoxanthoma elasticum.
Less commonly, the following conditions have also been described in patients with knuckle pads:3,18
- seborrhoeic dermatitis
- clubbed fingers (swelling of the soft tissues in the terminal phalanx of digits frequently seen in bronchopulmonary disease, cyanotic congenital heart disorders, cirrhosis and Crohn’s disease)
- oral leukoplakia
- glossitis
- avitaminosis A
- oesophageal cancer
- phenytoin treatment.
Answer 4
Knuckle pads need to be differentiated from other clinically similar lesions that may require specific treatments or are related to important underlying pathology.
Pseudo-knuckle pads are callus-like thickenings caused by repeated frictional trauma that have been linked to obsessive-compulsive behaviours in children (chewing pads), and occupational (eg carpet layers, tailors, live-chicken hangers, sheep shearers) or sporting activities in adults.5,9,18–21
A positive history of articular problems suggests possible differential diagnoses, such as rheumatoid (subcutaneous skin-coloured masses in patients with rheumatoid arthritis or systemic lupus erythematosus), Heberden’s or Bouchard’s nodes (bony growth of the distal and proximal interphalangeal joints in patients with arthrosis), gouty tophi (inflammatory nodules secondary to precipitation of monosodium urate crystals), synovitis (inflammation of synovial membrane due to synovial fluid buildup), and reactive hyperplasia of the paratenon (hypertrophic scar tissue on the extensor tendon) from knuckle pads.3,22
Erythema elevatum diutinum (an unusual type of leukocytoclastic vasculitis, which causes purplish nodules on extensor surfaces) and granuloma annulare (an inflammatory skin condition that presents with ringed papules on the dorsum of hands) may be clinically identical to knuckle pads and requires a skin biopsy to establish the diagnosis.23
Answer 5
Reassuring patients about the benign nature of the condition is mandatory. Topical treatments are usually ineffective and excision is not recommended because of the high risk of recurrence and scarring.3
Authors
Lidia Maroñas-Jiménez MD, Dermatologist, Hospital Universitario 12 de Octubre, Madrid, Spain. lydia.maroasjimenez@gmail.com
Ramon Pigem MD, Dermatologist, Hospital Clínic, Barcelona, Spain
Diana Menis MD, Dermatologist, Hospital Universitario 12 de Octubre, Madrid, Spain
Aurora Guerra-Tapia MD, PhD, Dermatologist, Hospital Universitario 12 de Octubre, Madrid, Spain
Competing interests: None.
Provenance and peer review: Not commissioned, externally peer reviewed.