The estimated prevalence of diagnosed GORD in patients attending general practice in Australia is 11.6% (95% confidence interval [CI], 10.5–12.6) and 7.5% (95% CI, 6.8–8.2) in the Australian population.5 These estimates do not include the presumably large pool of people with undiagnosed GORD in the community. A meta-analysis of the epidemiology of GORD suggests the community prevalence is 10–20% of the population in the Western world.6
Recently, some concern has been expressed about the volume of prescribing of proton pump inhibitors (PPIs), mostly for GORD, in Australia.7,8 The Royal Australian College of General Practitioners (RACGP) has recommended, as part of the Choosing Wisely Australia campaign, that doctors ‘don’t use proton pump inhibitors (PPIs) long term in patients with uncomplicated disease without regular attempts at reducing dose or ceasing’.9 Similar concerns by the Department of Veterans’ Affairs led to the release of a Therapeutic Brief on PPIs in 2012.10
Miller and Pan have previously reported changes in the management rate, investigations and treatment of GORD between 1998 and 2008 in response to altered treatment guidelines and regulatory changes.11 Our study investigated the extent to which there have been changes in the management of GORD since our previous report in 2009.11
Methods
This was a secondary analysis of data from the Bettering the Evaluation and Care of Health (BEACH) program. BEACH methods have been described in detail elsewhere.12 In brief, approximately 1000 randomly sampled, currently active, recognised general practitioners (GPs) participate in the BEACH program each year. Each GP records the details of 100 encounters with consenting unidentified patients on structured paper forms. BEACH has been running continuously since 1998.
All problems managed were classified according to the International Classification of Primary Care, Version 2
(ICPC-2 PLUS), through the ICPC-2 PLUS clinical terminology.13 Medications were coded using an in-house pharmaceutical terminology called the Coding Atlas of Pharmaceutical Substances (CAPS), which is classified according to the World Health Organization’s Anatomical Therapeutic Chemical (WHO’s ATC) classification.14
We extrapolated our results to provide national estimates using the total Medicare GP consultation items claimed in the selected years. The method is detailed in the BEACH annual report.15
The BEACH encounters analysed in this study were restricted to those with patients aged 15 years or older and recorded during two periods, April 2006 to March 2008 (n = 163,400) and April 2012 to March 2014 (n = 170,300).
Ethics approval for the BEACH program was obtained from the Human Research Ethics Committee of the University of Sydney (approval number HREC 2012/130).
Results
In 2006–08, GORD was managed at 4019 encounters in the BEACH sample, at a rate of 2.4 (95% CI, 2.3–2.5) per 100 encounters. In 2012–14, it was managed at 4767 encounters, at a rate of 2.8 (95% CI, 2.7–2.9) per 100 GP encounters, an increase of about 15% (Figure 1). There were significant increases in management rates of patients in the 15–24 and 65–74 age groups, and in both male and female patients. There was a low incidence of new GORD cases, being less than 0.4 per 100 encounters (Figure 1). Extrapolating these results to national estimates meant there were approximately 962,000 more encounters per year in 2012–14 at which GORD problems were managed in patients 15 years and older than there were in 2006–08.
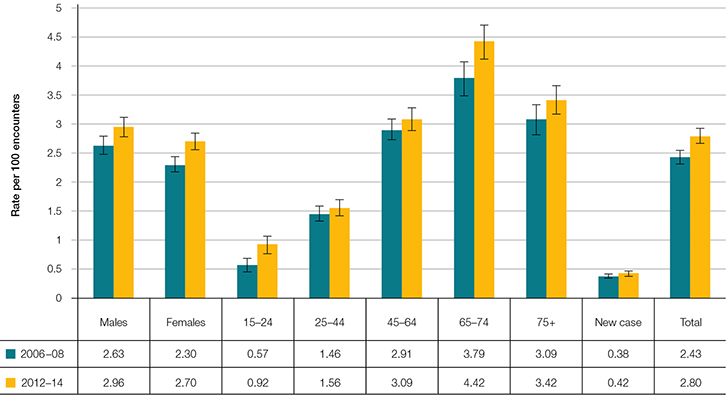 |
| Figure 1. Age-specific and sex-specific management rates of GORD in 2006–08 and 2012–14 (95% CI) |
Pathology orders for GORD increased from 10.9 (95% CI, 8.9–12.9) per 100 GORD problems in 2006–08 to 15.5 (95% CI, 13.1–17.9) per 100 in 2012–14. The rate of imaging orders remained static at about 2 per 100 GORD problems managed. Specialist referrals also remained static at about 4 per 100, and the majority (approximately 80%) of referrals were to a gastroenterologist or for endoscopy.
Medication rates remained constant at about 95 medications prescribed, supplied or advised per 100 GORD problems managed. Provision of PPIs increased from 78.0 (95% CI, 76.5–79.5) per 100 GORD problems in 2006–08 to 83.1 (95% CI, 81.9–84.3) per 100 in 2012–14. There was a reciprocal decrease in histamine-2 receptor antagonist (H2RA) provision from 6.0 (95% CI, 5.1–6.9) per 100 GORD problems in 2006–08 to 3.5 (95% CI, 3.0–4.1) per 100 in 2012–14 (Figure 2). There was no change in the prescribed daily dose of PPIs or H2RAs over the two data periods. In 2012–14, esomeprazole, the most commonly ordered PPI, was prescribed at a mean daily dose of 33.3 mg per day (95% CI, 32.7–33.9), with a median prescribed daily dose of 40 mg (results not tabled).
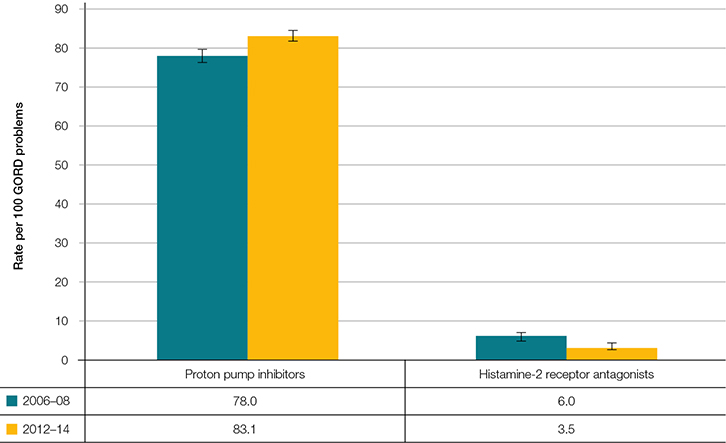 |
| Figure 2. Medication rates for GORD in 2006–08 and 2012–14 (95% CI) |
There was a significant increase in overall prescribing of PPIs for patients 15 years and older between the two data periods, from 3.1 (95% CI, 3.0–3.2) per 100 encounters in 2006–08 to 3.7 (95% CI, 3.6–3.8) in 2012–14. Extrapolating these results to national estimates meant there were approximately 1,339,000 more prescriptions for PPIs in patients 15 years and older per year in 2012–14 than there were in 2006–08. PPIs constituted 3.5% of all medications prescribed, supplied or advised by GPs for patients aged 15 years and older in 2012–14. GORD problems accounted for 64.9% (95% CI, 63.2–66.7) of PPI orders in 2012–14, and for 51.0% (95% CI, 45.4–56.6) of H2RA orders.
Discussion
This study shows that changes in the management rate and treatment of GORD between 1998 and 2008, reported earlier,11 have continued. Management rates have continued to rise, possibly reflecting unmet needs rather than an increased prevalence in the community. PPIs have continued to replace H2RAs as the medical management of choice, now making up 91% of prescribed medications for GORD. The prescribed daily dose of PPIs and H2RAs, and referral rates to specialists for GORD, remained static.
While BEACH is a cross-sectional, encounter-based study and we cannot report management changes over time in individual patients, the small proportion of new cases managed and the high prescribing rate for GORD suggests long-term medication use in many patients. The availability of over-the-counter H2RAs means that usage rates may be under-reported in this study.
GORD causes a significant reduction in health-related quality of life, particularly in the more severe ‘disruptive’ form of the condition.4 Acid suppressant therapy is effective in controlling the symptoms of GORD, but does not cure the disease. Relapse is common on withdrawal of therapy, which may explain why many patients continue on long-term therapy. Variation in severity means that therapy needs to be tailored to the individual patient.4
The risk of adverse drug events is an important consideration in drugs that are prescribed for long periods. PPIs constituted 3.5% of all drugs prescribed to patients aged 15 years and older in 2012–14; however, they constitute only 2.0% of adverse drug events reported in a BEACH study in 2007–10.16 Of PPI adverse drug events reported in that study, 39% were mild, 44% moderate and 6% were severe. These figures demonstrate a relatively good safety profile for PPIs, compared with other commonly prescribed medications.
Concern has been expressed regarding the economic burden of GORD management.7 The cost of PPI prescriptions to the Pharmaceutical Benefits Scheme (PBS) in 2006–08 was estimated to be $400 million per annum,11 which was reduced to $200 million per annum in 2013–14,7 probably because of the reduced cost of generic PPIs. Only 65% of PPIs ordered by GPs in the BEACH study were for the management of GORD. Those concerned with the economic cost of management should also consider the known economic cost of undertreated GORD to the individual and the community.17
Conclusion
GORD is an increasing health burden on the community and a significant cause of reduction in health-related quality of life for the individual patient. GP management advice to patients in Australia broadly conforms with established guidelines. As with all long-term medications, regular review of the need for PPIs and their dosage is an essential part of GP management.
Authors
Graeme Miller MBBS, PhD, FRACGP, Associate Professor and Medical Director, Family Medicine Research Centre, Sydney School of Public Health, Sydney Medical School, University of Sydney, NSW. graeme.miller@sydney.edu.au
Carmen Wong BHlthSci MHlthInformatics, Research Assistant, Family Medicine Research Centre, Sydney School of Public Health, Sydney Medical School, University of Sydney, NSW
Allan Pollack MB BS (Hons), MBiomedE, FRACS (Orth), Research Assistant, Family Medicine Research Centre, Sydney School of Public Health, Sydney Medical School, University of Sydney
Competing interests: None.
Provenance and peer review: Commissioned, externally peer reviewed.
Acknowledgements
We wish to thank the GPs who participated for their generosity. During the data collection period of this study, the BEACH program was funded by the federal Department of Health, AstraZeneca Pty Ltd (Australia), Novartis Pharmaceuticals Australia Pty Ltd, bioCSL (Australia) Pty Ltd, Merck Sharp & Dohme (Australia) Pty Ltd, Pfizer Australia Pty Ltd, Sanofi-Aventis Australia Pty Ltd, GlaxoSmithKline Australia Pty Ltd, National Prescribing Service Ltd, Janssen-Cilag Pty Ltd, Abbott Australasia Pty Ltd, Roche Products Pty Ltd, Bayer Australia Ltd, Wyeth Australia Pty Ltd and the federal Department of Veterans’ Affairs.