When patients present with vertigo, a diagnosis that should not be missed is benign paroxysmal positional vertigo (BPPV). This can be identified clinically without the need for investigations and, more importantly, it can be easily treated in primary care. Unfortunately, assessment for BPPV is usually done poorly. A retrospective study found only 10% of dizzy patients seen at a medical centre were assessed for BPPV using diagnostic manoeuvres.1 For those referred for vestibular assessments and confirmed BPPV, an estimated 10% had the Dix-Hallpike manoeuvre performed beforehand.2 Another study into a tertiary centre clinic identified 85% of patients with BPPV had classic symptoms and findings. Patients waited an average of 93 weeks until review and treatment.3
Overview of BPPV
The pathogenesis of BPPV is essentially a disruption in the vestibular system resulting in vertigo.4 There are three semicircular canals in each inner ear that are organised at approximately right angles to each other to allow the body to identify three-dimensional angular acceleration. At the base of each canal is the ampulla, which contains the cupula. When the head turns, endolymph movement causes cupula deflection, translated into information on head motion and position via the vestibular nerve. Canaliths or calcium carbonate crystals are present within the endolymph occasionally, contributing to additional conflicting abnormal cupula deflection, causing vertigo.4
The classical presentation of BPPV is recurrent, brief (<1 minute) episodes of vertigo triggered by changes in head position. Diagnosis of BPPV involves the Dix-Hallpike manoeuvre to provoke symptoms. After a short latency or pause, rotational or horizontal nystagmus associated with vertigo symptoms confirms the diagnosis.5 This is easily treated with the Epley manoeuvre, which displaces canaliths out of the semi-circular canal.6
The Dix-Hallpike and Epley manoeuvres are highly effective in posterior and anterior canal involvement. BPPV may less commonly originate from the horizontal semi-circular canals, for which a different manoeuvre (Lempert roll) is useful but will not be discussed further.
Performing the Dix-Hallpike and Epley manoeuvres
Dix-Hallpike is the diagnostic component in assessment of BPPV. The patient is seated upright. Explain the manoeuvre to the patient so they know what to expect. Turn their head 30–45° to the side tested. Supporting their head, lie them backwards quickly, with the neck slightly hyperextended off the bed. Observe for nystagmus and symptoms, allowing up to 30 seconds for latency. Sit the patient up and consider assessing the opposite side if the patient tests negative.
Perform the Epley manoeuvre for BPPV treatment after nystagmus stops if the patient tests positive. Turn their head to the opposite direction. The patient should rotate their body, facilitating further head rotation to 90°. This may trigger further nystagmus and symptoms. When the nystagmus and symptoms stop, return the patient to the seated position. This process can be repeated to increase the likelihood of symptom resolution or confirm BPPV termination.
The Dix-Hallpike and Epley manoeuvres are shown in Figure 1.
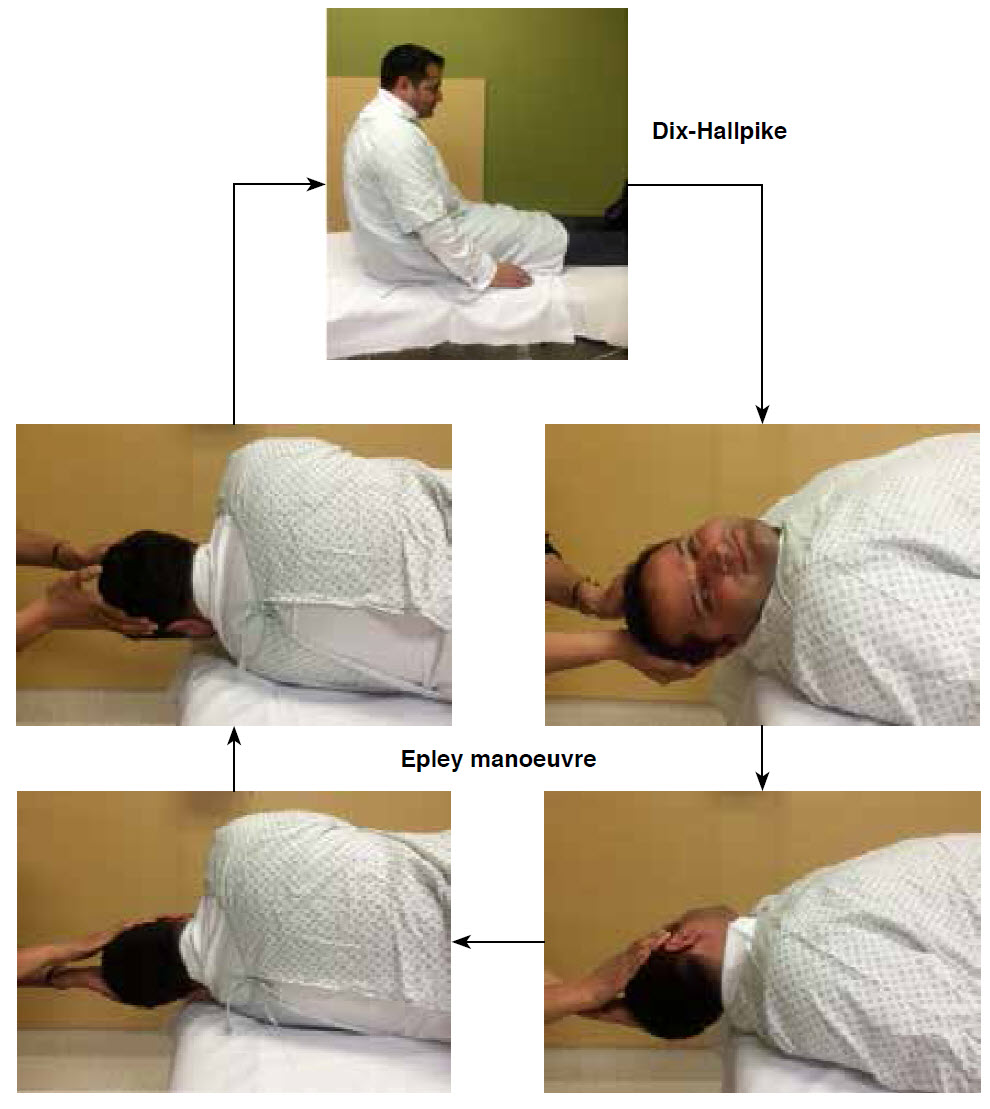 |
| Figure 1. Dix-Hallpike and Epley manoeuvres |
Why learn the Semont manoeuvre?
Physical limitations may prevent even the most practiced from performing the Dix-Hallpike and Epley manoeuvres. When assessing patients with vertigo, challenging aspects include anxiety and non-compliance. The rapid backward movement during the Dix-Hallpike manoeuvre can be challenging for those with osteoarthritis or who have had previous head or neck procedures and injuries limiting cervical spine movement, especially hyperextension. These have been noted particularly when assessing elderly patients. Elderly patients may be more frequently encountered over time with BPPV as their prevalence approaches 9%.7 For these patients, the Semont and liberatory manoeuvres are an alternative to the Dix-Hallpike and Epley manoeuvres, and may be easier to perform.
Performing the Semont and liberatory manoeuvres
The Semont manoeuvre is the diagnostic component in assessing elderly patients with BBPV. The patient is seated upright. Explain the manoeuvre to the patient so they know what to expect. Turn their head 45° away from the tested side. Move their upper body laterally towards the tested side (ie when testing for right posterior canal BPPV, rotate the head to the left, then their upper body laterally to the right). The patient should now be lying on their side facing towards the ceiling. Observe for nystagmus and symptoms, allowing up to 30 seconds for latency. Sit the patient up and consider assessing the opposite side if the patient tests negative.
Perform the liberatory manoeuvre for BPPV treatment after nystagmus stops if the patient tests positive. While lying on the tested side, the patient is moved quickly through 180° while maintaining the original head position to lie face down on the opposite side. This may trigger further nystagmus and symptoms. Return the patient to the seated position when nystagmus and symptoms stops. This process can be repeated to increase the likelihood of symptom resolution or confirm BPPV termination.
Semont and liberatory manoeuvres are shown in Figure 2.
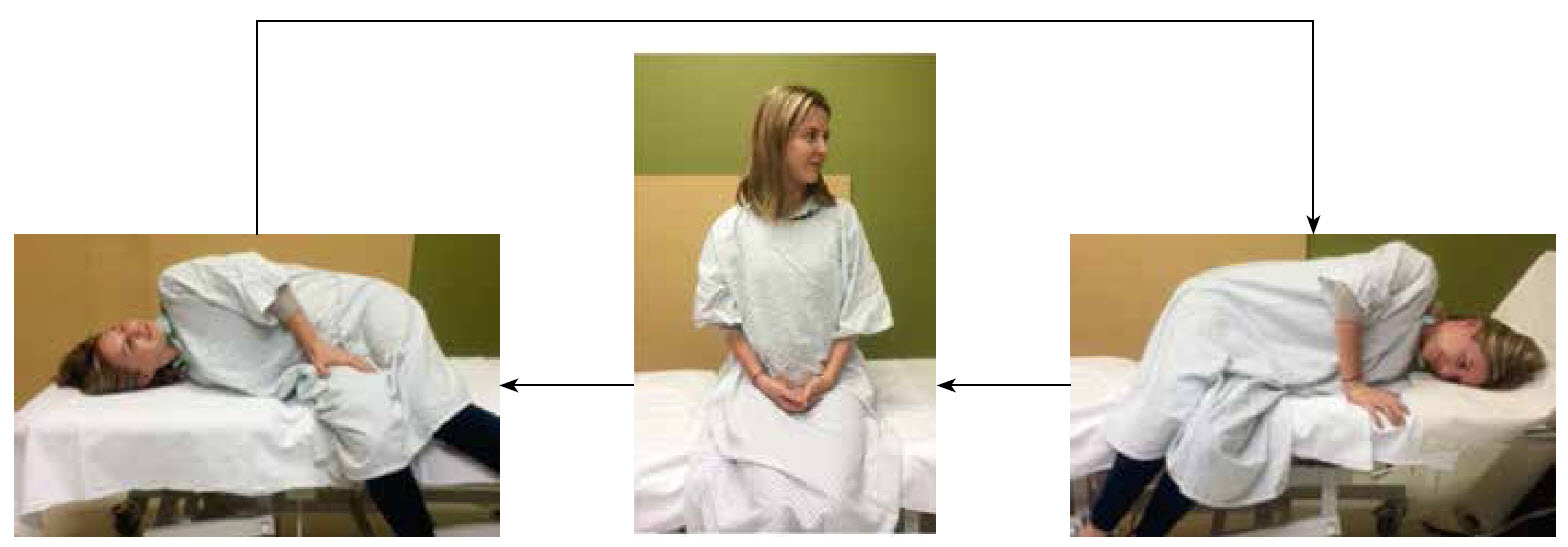 |
| Figure 2. Semont and liberatory manoeuvres |
Efficacy of Semont and liberatory manoeuvres
A randomised controlled trial found 86.8% patients recovered fully from vertigo after the Semont and liberatory manoeuvres, whereas none of those who had a sham manoeuvre recovered.8 Another similar trial found complete resolution in 84.6% with the Semont and liberatory manoeuvres when compared with 14.3% in a control group.9 A retrospective study comparing Epley, and Semont and liberatory manoeuvres did not identify statistically significant differences in treatment outcomes between the two groups.10 When reviewing the likelihood of canal conversion after repositioning, 7.8% with the Epley manoeuvre converted to horizontal canal BPPV. This is compared with none with the Semont manoeuvre. This is possibly due to a higher number of steps where the head is dependent during the Epley manoeuvre.11
A review of repositioning manoeuvres concluded that as the therapeutic efficacy is comparable, ‘the choice of treatment is generally based on clinician preference, complexity of the manoeuvres themselves, poor treatment response to specific manoeuvres and musculoskeletal considerations such as arthritic changes and range of motion of the cervical spine’.12
Conclusion
As the Semont and liberatory manoeuvres are simple, compared with the Dix-Hallpike and Epley manoeuvres, they should be part of the routine diagnostic process in assessing patients with vertigo and treatment in those with confirmed BPPV.
Author
Shyh Poh Teo MBChB, FRACP, Consultant Geriatrician and Physician, Older Persons and Rehabilitation Services, Hutt Valley DHB, Lower Hutt, New Zealand. shyhpoh.teo@gmail.com
Competing interests: None.
Provenance and peer review: Not commissioned, externally peer reviewed.
Acknowledgements
The author would like to thank Dr Enver Yousuf and Dr Jordon Wimsett for use of their images in this publication.