Cervical screening reduces the incidence and mortality of cervical cancer.1 In Australia, doctors provide 80% of cervical screening, whereas in the United Kingdom female nurses perform 70–85% of Pap smears.2 Nurses have an important role in cervical screening as women prefer female practitioners to undertake their smears.3 Of the 43,000 general practitioners (GPs) working in Australia in 2011, 43% were women, whereas 90% of nurses were women.4 The role played by practice nurses and a team approach to sexual healthcare in Australian general practice is underdeveloped. Increased recognition and support of practice nurse roles in sexual health is needed, including supportive practice systems that facilitate team care.5
A number of models exist for cervical screening in Australia. The most common model has GPs performing Pap smears. Some general practices have a nurse available for cervical screening as one of their daily roles. Another model is team care where nurses working alongside GPs and the patient sees both health professionals. Nurse-led clinics outside of general practice occur where nurses perform the Pap smears; credentialing as a Pap smear provider is required for this6 with a doctor agreeing to be a support.
Team care
Team care in general practice can enhance healthcare delivery.7 Teamwork and collaborative practice that includes the delegation of care, rather than the delegation of tasks, is identified in the literature as desirable in the general practice workplace.8,9
Pap smear quality
Nurses collect smears that are of the same quality as nurse practitioners and physicians.10 The presence of endocervical cells in a cervical cytology sample indicates that the transformation zone, where most cervical cancer develops, is likely to have been sampled.11 In Victoria in 2012, the percentage of Pap smears with an endocervical component collected by nurses was 75.8% and by other provider types was 73.4%.12
A team care model in one general practice
This study is derived from a general practice within an outer suburb of a regional centre in Western Australia where the average age in 2012 was 31.8 years.13 Nine GPs were working at the clinic during the study period. Cervical screening was initially provided by two male GPs and reminder letters for follow-up tests sent. The practice wanted to improve access to cervical screening.
In 2006 a registered nurse with qualifications in performing Pap smears (Sexual and Reproductive Health from the Sexual Health and Family Planning Australia) was employed. Two years later a second nurse was employed and since then a Women’s Health Clinic (WHC) has been available on one morning per fortnight.
Invitation letters
In Australia women are sent a letter from the National Cervical Screening Program if the register has no record of a repeat cytology within 27 months of a previously negative cytology result.11 Reminder letters are not sent to those who have never had a Pap smear.11
The practice sent invitation letters for women with no record of a Pap smear from the start of the audit in 2010. Invitation letters have been shown to be effective in encouraging women to attend for a Pap smear, and letters from GPs and local authorities are favoured over other sources.14 Patient lists were generated using the Pen Clinical Audit Tool (CAT) for women aged 20–69 years, active (three or more visits in the last 2 years) and with no record of a Pap smear. The audit tool excluded those with a coded entry in the past history of hysterectomy, and patient notes were checked for any correspondence regarding a hysterectomy. The list was updated periodically and letters sent educating about the importance of cervical screening and inviting them to the WHC.
Attendance at the WHC
A visit comprised seeing a GP of choice and then the nurse who performed the smear. Since 2010 a shared electronic template in the form of a table was used for note-taking by GPs and nurses.
The table contained two columns, allowing both doctor and nurse to enter notes so each could see what was discussed. The information collected and discussed included cervical smear, menstrual, social and reproductive history, chlamydia screening, mental health, breast awareness education, and contraceptive and continence advice.
The nurses were given scope to assess these areas according to the patient’s needs. The GP had a supportive role for the nurse and was available for discussion during the clinic.
If the smear collected was normal a letter was sent to the patient informing them of the result and that a reminder would be sent for the next scheduled test. Patient reminders in the form of mailed letters increase the rate of cervical cancer screening.15
Data collection
Cervical screening data for the audit were collected from 2010 to 2014 to investigate the impact of invitation letters and monitor the effectiveness of the team care approach. This was a quality assurance study not requiring ethical approval. The PenCAT extracted data from the clinical desktop system Best Practice16 for the active female population aged 18–70 years.
The two nurses recorded the results of the smears, including whether endocervical cells were present. Combined cervical smear quality data for all practitioners (doctors and nurses) were obtained via the database search utility in Best Practice. This was compared with the National Cervical Screening Program.
The nurses involved and the two GPs who worked before and after the commencement of the dedicated WHCs were asked to comment on the impact of the clinics on their work.
Results
Table 1. Practice cervical screening data
|
|
|
Active women
aged 18–70 years
|
Pap smear
last 2 years
|
Pap smear
last 3 years
|
Pap smear recorded
|
Pap smear
not recorded
|
|---|
|
August 2010
|
1098
|
48.09%
|
53.55%
|
58.29%
|
41.71%
|
|
August 2011
|
1555
|
43.47%
|
51.25%
|
56.21%
|
43.79%
|
|
August 2012
|
1501
|
49.30%
|
57.36%
|
64.36%
|
35.64%
|
|
August 2013
|
1408
|
53.27%
|
63.99%
|
72.09%
|
27.91%
|
|
March 2014
|
1415
|
53.57%
|
62.97%
|
72.01%
|
27.99%
|
Over 45 months there was an 11% improvement in the biennial cervical screening rate from 48.09% to 53.57% (Table 1). The 2-year participation rate for the National Cervical Screening Program was 57.2% of women in the target age group in 2010 to 2011.11 The percentage of women in the practice with no Pap smear recorded decreased from 41.71% to 27.99% from 2010 to 2014.
A reduction in the percentage of women with no Pap smear recorded occurred across all ages; the greatest reduction was seen for those aged 50–59 years. In the 18–29-year age group, the percentage with no Pap smear recorded increased in the last 6 months of the study by 6% (Figure 1).
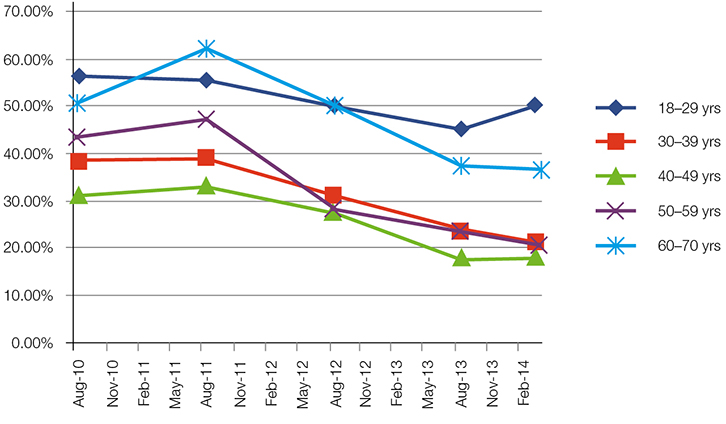 |
| Figure 1. Percentage of women with no Pap smear recorded |
Of the 488 smears taken by nurses, 390 had an endocervical component (79.91%). A total of 1575 smears was taken at the practice from 2008 to 2014 by all practitioners (doctors and nurses) and 62.92% had an endocervical component. In Australia in 2011, of the 2,065,618 cytology tests performed for women aged 20–69, 78.6% of cytology results had an endocervical component.11
In response to the question, ‘What is the impact of WHCs on their work?’, one doctor said, ‘I think the clinic has been time-saving for me and given opportunities to explore women’s health-related preventive activities with patients’. Female GPs who worked in the practice reported a reduction in the number of smears they were asked to perform.
One nurse reported, ‘there was a doctor available for that consult if I was concerned about abnormalities, and it provided the option for women to ask further questions if they didn’t feel comfortable talking about this with the doctor’.
Both nurses identified that one difficulty with the WHCs was managing the waiting time for the patients, particularly if a doctor was behind schedule. The nurse could see the patient first, but sometimes the waiting times were not ideal. There were a few patients with a history of hysterectomy who received invitation letters. Some patients reported they had a smear outside of the practice. This was noted and the data recorded.
The service was considered financially viable as the WHCs were generally well booked and mixed billing occurred.
Discussion
The practice cervical screening rate improved throughout the audit. There was an improvement in the percentage of women having a smear in the previous 2 years, as well as a reduction in the percentage of women with no recorded cervical screening. Factors other than invitation letters and team care with nurses may have contributed such as the service provided by the female GPs. There was one female GP at the practice in 2010 and four in 2014, and the number of smears taken by them was not recorded.
The smears taken by nurses had a higher proportion of endocervical cells than the nationwide average. This supports other data that nurses are highly effective in collecting Pap smears.10,17 The quality of smears taken by the nurses was higher than the practice average (doctors and nurses combined).
Summary
The article provides an example of a team care model of cervical screening in general practice. The model of care consisted of the nurse’s role extending further than performing Pap smears with the support of GPs. There was delegation of care to the nurses rather than delegation of task. Time saving for GPs was reported. Invitation letters for women with no record of a Pap smear contributed to improved cervical screening. Nurses were highly effective team members in the collection of Pap smears.
Authors
Darryn Rennie MBBS, FRACGP, DipACSCM, General Practitioner, Dalyellup Family Medical Centre, and Clinical Senior Lecturer School of Primary, Aboriginal and Rural Health Care with the University of Western Australia, Dalyellup, WA. drennie@westnet.com.au
Jennifer Boxsell BNurs, Post Grad Dip Ed, Lecturer, South West Institute of Technology, and Nurse, South West Gynaecology Women’s Health Clinic and Dalyellup Family Medical Centre, Dalyellup, WA
Kaye Pedretti Dip Nurs, Dip Midwifery, Prostate Cancer Specialist Nurse, SJOG Hospital, Bunbury Women’s Health Clinic and Dalyellup Family Medical Centre, Dalyellup, WA
Competing interests: Darryn Rennie is a director of DFMC Pty Ltd, which is a trustee of a service trust that provides administrative services to the doctors at DFMC. He receives distributions from the service trust.
Provenance and peer review: Not commissioned, externally peer reviewed.
Acknowledgement
The authors thank Associate Professor Andrew Kirke and Dr Ivan Jansz for their assistance with the article.