The issue: dementia in Australia
Dementia is one of the fastest growing diseases in Australia. In 2013, 322,000 Australians were diagnosed with a dementia-related disease. The prevalence is expected to increase fourfold by 2050.1 Dementia has recently been listed as a national health priority area and a National Framework for Action on Dementia 2014–2018 is currently in development.2 The anticipated impact of the disease will have significant ramifications for Australia’s future health systems.3
General practitioners integral to dementia care
Dementia care in Australia is largely delivered by primary healthcare practitioners and general practitioners (GPs) have an essential role in the early identification of symptoms, of diagnosis in association with specialist support and in ongoing management. However, detecting and diagnosing dementia is complicated, as it does not have a unique set of presenting symptoms; this can lead to delays in prompt diagnosis.4–6 Other factors reported by GPs, including uncertainty of diagnosis, limited consultation times, denial of symptoms and distress by patients and families, may also reduce detection of the disease,7 leading to a significant time lag between symptom onset and diagnosis.6
In rural areas, where access to specialist dementia services is limited, primary health practitioners are integral to dementia diagnosis, ongoing patient support and management.8 However, GPs may experience difficulties with diagnosing dementia and in understanding the referral pathways for treatment and support. Currently, a ‘case-finding’ approach to diagnosis and ongoing care of patients with dementia ‘which involves assessing only those with symptoms or signs such as lost prescriptions and missed appointments, or other behaviours mentioned by family members…and others’9 resides with GPs through access to current information about the disease and use of suitable tools and assessments.9–11
The Australian Government’s Living Longer. Living Better initiative4 advocates that GPs and other health professionals should have greater access to training and education programs, to assist them with timely diagnosis of dementia.
Online resources
An online resource is one method by which GPs can access current information about diseases, treatment and diagnosis. Knowledge-based repositories are easily updated and provide wide access to vast sources of information. Despite a dearth of research examining GPs’ usage of online resources, the limited international research indicates that the internet is increasingly used by physicians to access health information (including online medical information searches, use of electronic healthcare records and electronic transfer of patient records)12 and has broad appeal for sourcing reliable and relevant documents to assist with day-to-day medical practice.13 However, caution is required when using online resources – and for the online developers – in considering e-health communications that are interoperable, easy to use, engaging, accessible and accurate.14
The Dementia Pathways Project in the Grampians
In 2012, extensive consultation with GPs and practice nurses across the Grampians region identified that there was an incomplete understanding of available dementia services in the region. There were no localised pathways to assist primary health practitioners with diagnosis, timely referral to specialist services for further investigation of dementia or local support options pre/post-diagnosis.
These outcomes prompted the Dementia Pathways project, aimed at providing primary health practitioners (primarily GPs and practice nurses) with access to online information to assist with diagnosis, referral and ongoing management of patients with dementia (or presenting with the symptoms of dementia) in accordance with evidence-based guidelines to local support services.
Developing the online knowledge repository about dementia for the Grampians
The Grampians is an area of 48,000 km2 that is largely rural but incorporates the larger regional service centres of Ballarat, Ararat, Stawell and Horsham. The population is approximately 223,000 and 14% are aged 65–84 years (compared with the state average of 12.1%).15 Approximately 354 GPs work within the region.16
An online repository for information and knowledge management was chosen above other ‘traditional’ methods of information as it enables large amounts of information, from multiple, reputable sources to be accessed via the internet. Online information is also available for GPs (who have internet access) across a diverse geographic region.
Another advantage of presenting information via an online repository is the capacity to quickly and efficiently update information. This is especially important given the dynamic nature of information now available and the increasing involvement of private, philanthropic and voluntary providers within the health service system. A similar tool for GP mental health care support has previously been implemented in the Grampians region and was found to be an important resource for accessing mental health information for GPs and allied health professionals.17 Some of the features of this earlier project helped inform the Dementia Pathways Tool, although the Dementia Pathways Tool was enhanced by the support and contributions of stakeholders during the design and development and content of the Tool.
Staged development of the Dementia Pathways Tool
Partner organisations for the Dementia Pathways project included:
- Department of Health (Grampians) and project funder
- Grampians Medicare Local
- Federation University Australia’s Centre for eResearch and Digital Innovation (CeRDI).
The regional dementia project officer guided the project and adopted an inclusive management approach involving wide consultation with stakeholders. Subsequent development of the Dementia Pathways Tool comprised five stages, each building on the previous stage, requiring commitment to input in the development to successfully achieve the required outcomes. These stages are outlined in Table 1.
Table 1. The stages comprising the development of the Dementia Pathways Tool
|
|
Staged development of website
|
|---|
|
Stage and focus
|
Input
|
Outcome
|
|
Stage 1: Identifying the barriers to dementia diagnosis for GPs in the Grampians.
|
Extensive consultation of health service providers in the region was achieved through a survey that was developed in consultation with GPs, practice nurses and other health service providers.
|
The barriers in the Grampians to dementia diagnosis and management were identified as: incomplete understanding of available dementia services in the region; no localised pathways to assist primary health practitioners with diagnosis, timely referral to specialist services for further investigation of dementia, and local support options pre/post-diagnosis.
|
|
Stage 2: Steering the project.
|
A steering group (n = 12) was established comprising ‘stakeholders’; GPs and practice nurses.
|
The steering group met regularly and identified their preferences for visual display and presentation; navigational/pathway flow (and ease of use of online resource); website features, and content (prioritising what information was required about dementia, diagnosis, management, relevance of content, amount of information).
Discussion about the content of the Pathways Tool with the steering group was prompted by a series of scenarios and associated questions about doctor-patient consultations for dementia. Examples of other web-based dementia navigation tools from Australia and overseas were also presented to stakeholders to identify particular preferences for the display and content.
Stakeholders prioritised the content to be included in the Tool: clinical and management knowledge-base and tools; evidence-based guidelines and consultation checklists; screening tools, links to local dementia resources and services and referral options.
|
|
Stage 3: Provision of expert advice on the content of the Tool
|
Expert advice on the content for the Dementia Pathways Tool was provided by a Consultant Physician in Geriatric Medicine. Essential content, including national and international resources, was sourced.
|
Content for the Tool included: pathways for local referrals and supports; local resources; recommended assessments; investigation and review of cognitive decline (including key decision points for specialist referral or continued assessment/support); contact details about local support services for patients and carers; information about advance care plans.
|
|
Stage 4: Developing the Tool:
|
An interactive web-based tool was designed and developed following input at Stages 1–3.
|
Key features of the Tool:
- A split-screen and toggle menu to facilitate navigation of the Tool and enable access to relevant information via five key menu options (Awareness and recognition of significant symptoms; Diagnosis; Ongoing management and care; Palliative and end-of-life care; Family support). Users can access the menu items (located on the left of the split screen) through a pathway that branches out into successive, secondary menu items (See Figure 1 for example).
- A comprehensive keyword search and expandable information layers to provide additional options to search and retrieve specific content. Users can navigate quickly through the pathway using the menu items as a logical guide.
- Additional features of the website include: an interactive pathways map; a support tool and service directory of local contacts; referral pathways; links to other resources and websites; embedded assessment tools; and resource pages (includes MBS items).
|
|
Stage 5: Trial and launch of the Tool
|
|
Steering group members were invited to review the online Dementia Pathways Tool and provide feedback on all components of the Tool, including the visual display, pathway flow (consistency, ease of navigation), and content (relevance, language, sufficiency of information).
Feedback during the trial period enabled further changes and improvements to the Tool prior to its official launch in August 2013.
Informal, anecdotal feedback from steering group members during the trialling of the pathways was positive (‘The pathway software and information are absolutely brilliant’; ‘It is excellent’).
The Tool is available on the Grampians Medicare Local website: http://www.grampiansml.com.au/dpp/
|
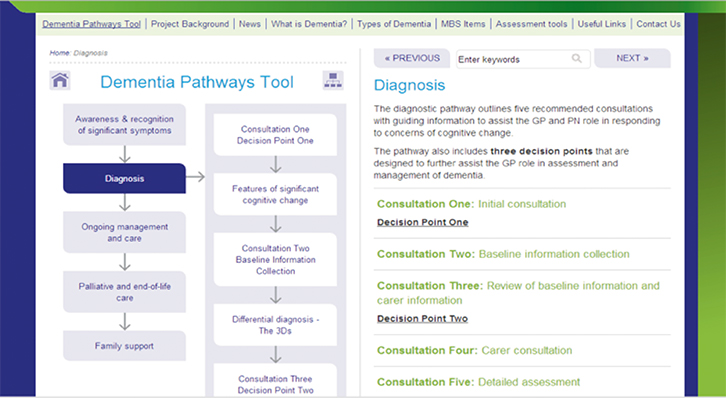 |
| Figure 1. Dementia Pathways Tool menu, ‘Diagnosis’ page |
Local uptake of the Dementia Pathways Tool
Preliminary feedback and visitor statistics to the website in the 9 months since the launch of the Dementia Pathways Tool have been positive. The number of page views has been constant, averaging approximately 500 page views per month since its launch in August 2013. The average time visitors spent on each page was 2 minutes and 6 seconds, and just under half of the recorded page views (1900) were of the main Dementia Pathway Tool content pages.
Other frequently visited pages included how to use the tool, assessment tools, project background, useful links, Medicare Benefits Schedule items and types of dementia.
Broader practice benefits
Although the Dementia Pathways Tool was designed and developed specifically for practitioners in the Grampians region and contains a host of local resources, the website has much broader appeal. As a publically accessible resource it offers all GPs and health professionals a web-based repository of dementia-related information, tools and resources to guide and enhance current assessment and referral practices.
This resource now enables dementia diagnosis to be made over a number of months, allowing the process to be broken into steps that are manageable within the primary care setting. The Tool facilitates informed management of the complexities and identified barriers to dementia diagnosis.
Furthermore, the quality of content, presentation and style has value for a range of other audiences (patients and carers), while the functionality of the Tool has the potential to be adapted for use in other areas of health, such as for cancer or diabetes, or with other mental health initiatives.
Conclusion
The provision of online information to support health providers within the practice setting should complement rather than supersede the knowledge of qualified and experienced health professionals about disease diagnosis and management.
The literature suggests that for many practitioners, including GPs in rural settings, barriers exist that limit timely diagnosis and affect ongoing management of dementia.5,7 The challenge of this project was to develop a tool that could address some of these identified barriers by consolidating knowledge through an internet tool that aids professionals’ development and practice.
Online support tools offer a means of gaining disease-specific and localised referral pathways that meet the needs of health professionals, irrespective of geographic location, and may overcome some of the barriers in dementia diagnosis for GPs in rural and regional areas.7,10,13 The Dementia Pathways Tool provides information about region-specific, specialist dementia services and supports, together with current, accurate and relevant information about dementia to assist GPs in their practice, providing information to aid in assessment and diagnosis, referral, management and ongoing care. Access to an intuitive, online resource may also address the time restraints that some rural practitioners have identified as limiting their capacity to detect dementia.7
The next stage in the continued development of this Tool is to conduct a formal evaluation. This is now being planned using qualitative and quantitative data collection methods that will provide insights into the use of the Tool within the rural and regional practice setting and to identify how GPs and practice nurses access and use this online repository.
Author
Alison Ollerenshaw MAppSc, DipPM, Grad Dip AppSc (Prof Psychology), BA, Research Fellow, Centre for eResearch and Digital Innovation, Federation University Australia, Ballarat, VIC. a.ollerenshaw@federation.edu.au
Competing interests: None.
Provenance and peer review: Not commissioned, externally peer reviewed.
Acknowledgements
The author wishes to acknowledge the support received from staff at each of the partner organisations collaborating on this project. Particular thanks are extended to Carolyn Gargiulo (Department of Health, Grampians), Associate Professor Mark Yates (Deakin University and CDAMS, Ballarat Health Services), Heather Campbell (Grampians Medicare Local) and Dr Helen Thompson (Centre for eResearch and Digital Innovation, Federation University Australia) for ongoing support throughout this project and in providing valuable feedback on the development of this manuscript.