Varicose veins are a common reason for presentation to general practitioners. Clinically significant venous disease can cause symptoms such as aches and pains, cramps, restlessness and heaviness in the lower limbs. Swelling or skin damage secondary to chronic venous insufficiency occur in about 15% of the population and varicose ulcers develop in approximately 1% of the population. With increasing levels of obesity in the community, and an ageing population, venous disease is expected to place an increasing burden on the Australian healthcare system in the future.
International guidelines for the management of varicose veins
Recent international guidelines for the management of varicose veins have been issued in the UK, US and Europe. These guidelines recommend that endovenous thermal ablation (laser or radiofrequency) should be offered before surgery for the treatment of great saphenous vein reflux (Table 1).1–3
Table 1. Excerpts of guidelines from the UK, US and Europe
|
UK – 20131
Reproduced with permission from the National Institutes of Health and Care Excellence
|
|
US – 2011
The American Venous Forum and the Society for Vascular Surgery
Key recommendations:
For treatment of the incompetent GSV, endovenous thermal ablation (radiofrequency, RF, or endovenous laser therapy, EVLT) is recommended over high ligation and stripping of the saphenous vein to the level of the knee. Recommendation:
GRADE 1 (strong), level of evidence: B (medium quality).2
|
|
Europe – 2015
Clinical practice guidelines of the European Society for Vascular Surgery
Recommendation 43:
For the treatment of great saphenous vein reflux in patients with symptoms and signs of chronic venous disease, endovenous thermal ablation techniques are recommended in preference to surgery3
Class 1, Level A3
|
Treatment of saphenous reflux
Truncal reflux from incompetence of the great or small saphenous veins is a major contributor to clinically significant venous pathology.
Conventional surgery
High ligation, stripping and avulsion has been the standard method of removing saphenous veins for at least half a century. Surgery requires general anaesthesia and hospitalisation, and some significant degree of post-operative morbidity is not uncommon. Recurrence of varicose veins after surgery is a long‑recognised complication with incidence rates of 25–50% within five years.4–6 Neovascularisation due to regrowth of new veins in the saphenofemoral junction (Figure 1) is thought to be a significant cause of recurrence of varicose veins after surgery.7–9 Other causes may include incomplete, inappropriate or inadequate surgery or re-endothelialisation of the stripped great saphenous vein track within the saphenous compartment.
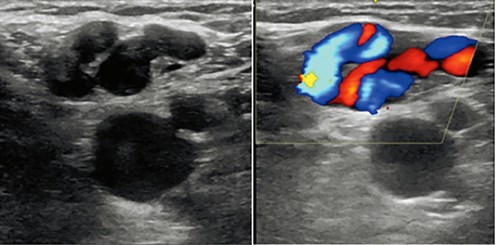
Figure 1. Colour Doppler ultrasound appearance of venous reflux in the saphenofemoral junction resulting from post-surgical neovascularisation
Endovenous thermal ablation
International guidelines now recommend endovenous thermal ablation as first-line treatment for the elimination of saphenous vein reflux.1–3 Endovenous thermal ablation causes an irreversible thermal injury in the vein wall, leading to fibrosis and, eventually, complete resorption over several months (Figure 2).

Figure 2. Ultrasound appearances of the great saphenous vein prior to and following endovenous laser ablation at one week and seven months
Two methods of endovenous thermal ablation are available: radiofrequency ablation10 and endovenous laser ablation,11 which was first performed in Australia in 2002. The success rate for both procedures is reported to be in the vicinity of 95%.
Endovenous thermal ablation requires ultrasound guidance and, with the use of topical, regional and tumescent anaesthesia, can be performed while patients are awake. A desirable advantage of this method is that patients can be treated in an office-based setting and then walk out following the procedure. Any prolonged period of immobility in hospital raises the risk of venous thromboembolic disease.12
Ultrasound-guided foam sclerotherapy
The use of ultrasound-guided foam sclerotherapy for the successful abolition of saphenous vein reflux was first reported in 1996.13 Efficacy and safety of ultrasound-guided foam sclerotherapy is now well established.14 The National Institute for Health and Care Excellence (NICE) guidelines (Table 1) recommend offering ultrasound-guided foam sclerotherapy before surgery for treatment of saphenous vein reflux.1 Catheter-directed sclerotherapy, which was first described in Australia,15,16 is a modification of ultrasound-guided foam sclerotherapy. The saphenous trunk is initially catheterised and perivenous tumescent anaesthetic is then injected under ultrasound guidance to collapse the vein and remove intraluminal blood, which strongly inactivates sclerosant.17 The removal of blood means that only small doses of sclerosant are needed to treat extensive networks of varicose veins (Figure 3).
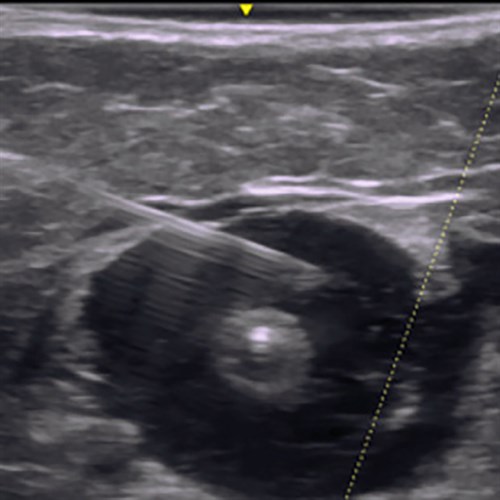
Figure 3. Ultrasound-guided injection of peritumescent anaesthetic compressing the great saphenous vein
Endovenous adhesive ablation
Injection of adhesive cyanoacrylate glue via an elaborate catheter system is a recently introduced technique with early success in ablation of saphenous trunks, although long-term safety and efficacy data are currently lacking.18 Compression stockings are not required following the procedure and only a single injection of local anaesthetic is required at the insertion site. The procedure time is relatively short and both legs can be treated in one sitting. Cyanoacrylate glue triggers an inflammatory reaction in the vessel wall causing fibrosis and occlusion.
Endovenous mechanicochemical ablation
Clarivein is a mechanicochemical ablation technique. The system simultaneously injects a sclerosant solution while at the same time scouring the internal wall of the vein with the tip of a rotating wire. Mechanicochemical ablation induces more endothelial damage, compared with liquid sclerosants, but no comparison has been made with foam sclerosant. Long-term safety and efficacy data are also lacking.
Treatment of tributary veins
Surgery and ultrasound-guided foam sclerotherapy are different methods of removing tributary veins that appear as varicose veins on the surface of the legs distal to the saphenous veins. Endovenous thermal ablation, mechanicochemical ablation and cyanoacrylate glue, which are designed to abolish saphenous vein reflux, are not suitable techniques for removal of tributary veins.
Surgery
A refined method of surgically avulsing tributary veins is ambulatory phlebectomy, which can be performed under local anaesthetic. The vein is extracted through a series of small incisions using a specialised hook. Long segments of vein can be removed through one incision. Not all areas of the lower limb are suitable for ambulatory phlebectomy because of thick skin or underlying fibrous tissue, such as the knee, or in areas of previous surgery. Ambulatory phlebectomy is often not suitable over the shin or foot areas because of a lack of subcutaneous fat, which makes it difficult to hook the vein. Ambulatory phlebectomy is not a suitable technique to remove the great or small saphenous vein.
Ultrasound-guided foam sclerotherapy
Large and small tributary veins in all anatomical positions of the lower limb can be targeted with ultrasound-guided foam sclerotherapy. The 2015 European guidelines recommend foam sclerotherapy for all types of vein disorders, including incompetent saphenous veins, as well as all incompetent tributaries.3,19–21 Injury to arteries and nerves is minimised because these structures are visible on ultrasound.
Treatment of recurrent varicose veins after surgery
Recurrence of varicose veins after surgery may present as severe disease with large tortuous varicose veins extending distally from the proximal site of the surgical incision in the groin or popliteal fossa. Extensive surgical re-exploration and excision are no longer indicated, but ambulatory phlebectomy is suitable with more limited disease.
Ultrasound-guided foam sclerotherapy is now the most widely used method of treating recurrence of varicose veins after surgery and is the treatment of choice especially in the popliteal fossa where nerves are vulnerable to injury.22–24 Catheter-directed sclerotherapy is a more suitable method for larger varicose veins if the maximum safe volume of sclerosant foam (20 mL) is likely to be exceeded.
Treatment of non-saphenous reflux
Non-saphenous vein reflux causes approximately 10% of venous disease. Common sites of non-saphenous vein reflux are the buttock, perineum, posterolateral thigh, posterior distal thigh and the knee. These veins have a tendency to be tortuous, with complex tributaries, and ache is a frequent symptom.25
Non-saphenous vein reflux presenting as gluteal, vaginal or pudendal veins is treatable with ultrasound-guided foam sclerotherapy.26 If reflux occurs from more than one of these sites simultaneously, pelvic vein reflux should be suspected and further investigation undertaken to look for evidence of ovarian vein incompetence. Rare causes include conditions that impede venous return, such as iliac vein thrombosis, retroperitoneal tumours, Nutcracker syndrome (compression of the left renal vein) and May–Thurner syndrome (right common iliac artery compressing the left common iliac vein).
Discussion
International guidelines currently recommend endovenous thermal ablation as first-line treatment for saphenous vein incompetence, but levels of evidence within the different guidelines should be highlighted. The NICE guidelines are based on low and very low levels of evidence.27 The level of evidence used by the American Venous Forum and Society for Vascular Surgery Guidelines2 is high for early efficacy but low for long-term efficacy.
There have been a number of randomised controlled trials (RCTs) comparing surgery and endovenous thermal ablation, looking at outcome measures such as recurrence, neovascularisation, post-procedural complications and quality of life.28,29
A systematic review of RCTs in 2012 found primary and recurrence rates to be no different after endovenous thermal ablation or surgery, but that endovenous thermal ablation had a lower rate of complications, such as wound infection and haematoma, as well as less pain and a faster return to work.30
Causes of recurrence common to all procedures include a pelvic origin of reflux or new reflux developing from other saphenous veins. Recurrence due to neovascularisation is less commonly seen after endovenous laser ablation than after surgery and is most likely to be due to new reflux in other saphenous veins.29,31
Higher rates of recurrence for treatment of saphenous vein incompetence are reported with ultrasound-guided foam sclerotherapy than with endovenous thermal ablation and surgery,32 but data from these studies tends to be confounded by the non-standardised nature of ultrasound-guided foam sclerotherapy, which has multiple variables associated with the technique. An advantage that ultrasound-guided foam sclerotherapy offers is that it is a relatively quick procedure to perform, does not require anaesthesia and, unlike endovenous thermal ablation and surgery, can be performed repeatedly.
Conclusion
Venous disease is a common medical condition that can progress, resulting in significant morbidities, such as leg ulcers, superficial vein thrombosis and venous thromboembolism. Early intervention and treatment of venous disease will help prevent these complications. The types of intervention available for the treatment of venous disease have increased dramatically in the past 20 years. Surgery, which has been considered first-line management, is now being displaced by minimally invasive techniques with claimed benefits of improved early quality of life, less morbidity and faster recovery times, allowing an earlier return to work and resumption of normal activities.
It should be noted, however, that international guidelines have not used high levels of evidence in making their recommendations. A Cochrane review in 2014, which the authors highlight is not a guideline, did not find sufficient evidence to support one method over another.
To date, incompatibility between studies has tended to limit interpretation of results. Results of more appropriately powered RCTs are expected to be reported in the next few years so that efficacy outcomes for the different modalities of treatment can be more accurately determined.
Author
Nicholas Kemp, MBBS, FRACGP, DRACOG, FACRRM, Dip Procedural Phlebology (ACP), GradCertHlth Sci Medical Sonography (Sydney), Auchenflower, Qld. nick@thelegveindoctor.com
Competing interests: None
Provenance and peer review: Not commissioned, externally peer reviewed