Case
Sarah, 20 years of age, is a student who presented to her family doctor with a one-day history of vertigo and occipital headache. She denied photophobia, neck stiffness, or altered vision or hearing. Sarah had been admitted to a general hospital ward one week earlier with a diagnosis of viral gastroenteritis complicated by diabetic ketoacidosis (DKA). At her presentation one week earlier, her initial pH was 7.28, bicarbonate was 13 mmol/L and ketones were 4.4 mmol/L. She had an uncomplicated recovery with standard care, including fluid rehydration and an insulin infusion. Sarah’s medical history included type 1 diabetes mellitus, diagnosed at 8 years of age, with no previous DKA episodes or vascular complications. A recent glycated haemoglobin (HbA1c) measurement was 62 mmol/mol (7.8%). She self-administered insulin detemir twice daily and insulin aspart with meals. Sarah was not on any other regular medication, and there was no other significant personal or family medical history. She denied smoking cigarettes, use of alcohol or recreational drugs, including no cocaine or amphetamine use.
On examination, Sarah’s blood pressure was 130/70 mmHg, and she had a pulse rate of 70 beats per minute and regular. Neurological examination revealed subtle right beating nystagmus in all directions of gaze. Skew deviation and head thrust testings were unremarkable. Cerebellar testing revealed subtle dysdiadochokinesia and Sarah was unable to perform tandem gait. However, there was no dysmetria and ataxia, and Romberg’s test was negative. There were no other significant findings on the remainder of the neurological or physical examinations. Her family doctor ordered cerebral magnetic resonance imaging (MRI), and a representative image is shown in Figure 1. Sarah was referred to the neurology unit of a tertiary centre for further management.
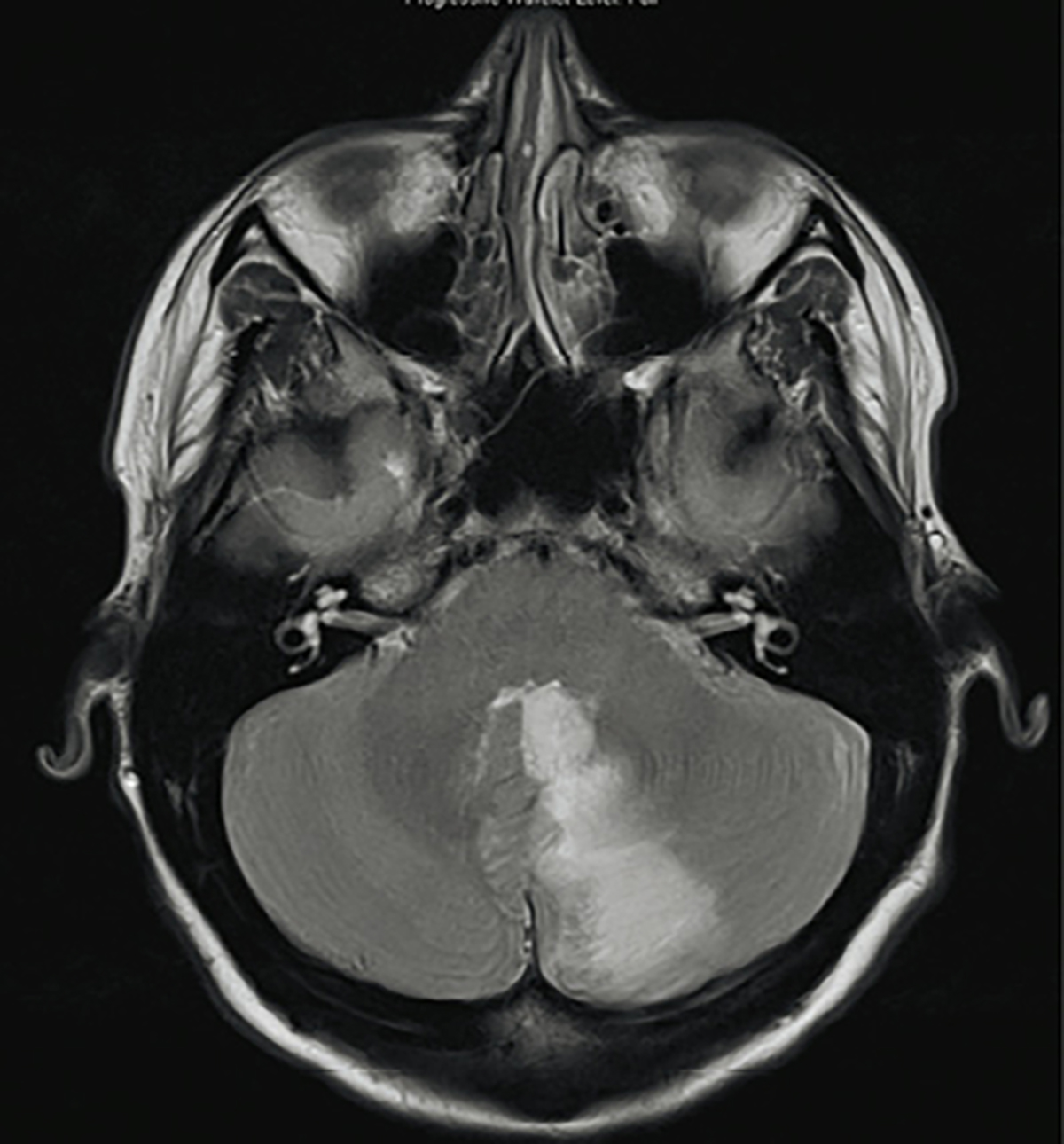
Figure 1. Cerebral magnetic resonance imaging scan for workup of vertigo
Question 1
What does the MRI show?
Question 2
Could this lesion be associated with her recent episode of DKA?
Question 3
How does DKA increase the risk of stroke?
Question 4
How should Sarah be managed? Is there a role for anticoagulation?
Answer 1
Sarah’s cerebral MRI shows a left-sided inferomedial cerebellar infarct in the territory of the posterior inferior cerebellar artery. This lesion would account for her vertigo and nystagmus.
Answer 2
The lesion on Sarah’s cerebral MRI could be associated with her recent episode of DKA, which is associated with a range of neurological complications. The most common complication is cerebral oedema, occurring in 6.8 per 1000 episodes of DKA.1 Less commonly, various stroke subtypes, including arterial thrombus, arterial embolus, venous thrombosis and intracerebral haemorrhage, have also been described in patients with DKA.2
Answer 3
Several mechanisms contribute to stroke in patients with DKA. These include deficiencies in proteins C and S; elevated levels of factors V, VIII and Von Willebrand factor; abnormal platelet aggregation; impaired fibrinolysis; and diffuse vascular injury secondary to systemic inflammation.3
Answer 4
Previous case reports have largely focused on the paediatric population and, therefore, management considerations and outcomes may differ for young adult patients. While strokes in infants and young children may initially present with non-specific symptoms prior to the development of focal signs,4,5 clinicians should have a low threshold for timely neuroimaging in older patients with new focal neurological deficits following DKA. It may also be beneficial to educate patients to recognise that such symptoms may be indicative of a stroke in order to maximise the window for effective thrombolysis. Prophylactic anticoagulation has been posited as a measure to reduce the risk of stroke in DKA,5 although there are no randomised controlled studies to date to evaluate the efficacy of this. Moreover, strokes have been described to occur from several hours up to several days after the presentation of DKA.4 It is unknown how long anticoagulation should be continued before the risk of haemorrhage outweighs potential benefits.
Case continued
Sarah also had a fasting lipids study, vasculitic screen, transthoracic and transoesophageal echocardiograms, and carotid artery ultrasound to check for other stroke risk factors. These tests were all within normal limits.
She was commenced on lifelong aspirin and an angiotensin-converting enzyme (ACE) inhibitor for secondary stroke prevention. A statin was considered, but not prescribed, as Sarah had a normal lipid profile, and lifetime use at such a young age would increase the chance of medication side effects. Sarah underwent rehabilitation and made a complete neurological recovery, returning to full-time study.
Key points
- DKA is a risk factor for several neurological complications, including stroke, which can occur hours to days following an episode of DKA.
- Cerebellar strokes typically present with sudden onset of symptoms, severe ataxia, and direction changing nystagmus. However, some presentations are far more subtle.
- As such, clinicians should have a low threshold for ordering neuroimaging on patients who present with a sudden onset neurological deficit in the context of recent DKA. MRI has a higher sensitivity than computed tomography for detecting acute ischaemic strokes (83% versus 26% respectively),6 and is the definitive modality for imaging the posterior fossa.
- Management includes optimising stroke risk factors and consideration of secondary stroke prevention therapy: antiplatelet agent, statin and ACE inhibitor.
Authors
Emma Foster MBBS (Hons), Neurology registrar, Neurosciences Department, Alfred Health, Prahran, Vic. dr.ecfoster@gmail.com
Phoebe Gao BMedSc (Hons) MBBS (Hons), Neurology resident, Neurosciences Department, Alfred Health, Prahran, Vic
Jorge Zavala MD, Consultant Neurologist, Neurosciences Department, Alfred Health, Prahran, Vic
Competing interests: None.
Provenance and peer review: Not commissioned, externally peer reviewed.