There has been significant attention in the medical literature and lay press about the increase in emergency department (ED) presentations in Australia.1 Questions have been raised as to whether all the presentations to the ED are true emergency services. It is thought some patients may be safely provided care in the primary care or less acute settings.2 Such settings may provide for a more efficient use of healthcare resources. Efforts to determine the magnitude of this potential group of patients have been the focus of much speculation and empirical research.3
One of the greatest challenges in determining the proportion of visits that may be conducted outside the ED is developing a workable and reliable method to identify these patients. The Australasian triage scale is used to triage patients presenting to the ED on a scale of urgency from 1–5, with categories 4 and 5 determined to be the least urgent.4 Some have suggested the least urgent presentations might be more appropriately treated in primary care settings. Others believe using the Australasian triage scale alone is too simplistic as it was developed to only assess urgency and not acuity of a specific patient presentation.3,5 Therefore, some patients may have a high complexity condition with a relatively low urgency, who may require specialised emergency care.
As such, some investigators have suggested additional exclusion criteria be applied to more selectively identify ED patients who may be safely treated in primary care settings.6,7 These have been termed ‘primary care type’ presentations. Although no classification system will have 100% specificity, such efforts would allow for a more nuanced view and determination of patients whose care may be safely provided outside the ED.
However, some of the proposed criteria for primary care type ED presentations may have age-specific variability.6 Assessment on the age-specific magnitude, due to the presence of specific criteria over time, have not been conducted. Such information is important to clearly identify potentially preventable ED presentations and develop strategies to provide care for patients in an out-patient setting. This is crucial because of the changing demography (eg ageing) in Australia, and the impact it may have on ED utilisation.8 Previous studies have not attempted to assess the magnitude of potential primary care type visits by age group. This can help to determine the true volume of such care so that efforts in improving ED care can be focused most effectively.
We conducted an analysis of the Victorian emergency minimum dataset (VEMD) using data from 2002–13 to provide such information. The VEMD contains comprehensive data on all ED presentations to public hospitals in Victoria, Australia.9
Methods
Data were obtained for the 2002–05, 2007–08 and 2010–13 financial years from the VEMD to provide a representative view of trends over time.9 The VEMD includes de-identified demographic and clinical data derived from presentations to all Victorian public hospitals with a 24-hour staffed ED. Currently, there are 38 hospitals providing data to the VEMD. Six began providing data in 2003, one in 2004 and one in 2011. A detailed description of ED presentations from the most recent data (2012–13) was conducted to illustrate the number of patients presenting to the ED and the manner in which primary care type visits were calculated.
Individuals presenting to an ED are first ‘triaged’ or assessed for objective clinical urgency by an ED staff member who is specifically trained for it. The triage category is assigned according to five categories in the Australasian triage scale.4
The Australasian triage scale classification system only includes determination of the urgency of a patient’s condition and not the severity of the condition. Categories 4–5 (lowest urgency) are grouped to contrast with categories 1–3 (highest urgency) in this study.
Five more data fields (referral source, arrival transport mode, inpatient bed request status, time first seen by doctor, time of departure) were also extracted from VEMD to categorise potential primary care type ED presentations.
We defined primary care type ED presentations in this study as those assessed as triage category 4 or 5, but excluding patients who were:
- admitted to the hospital from the ED
- transported by ambulance
- referred by a GP
- treated in the ED for more than12 hours, excluding time spent in the waiting room.
This definition is based on the work by Siminsky and others.6 The criteria are designed to assist with identifying patients who could most likely be treated safely outside of the ED because of the low urgency of their conditions. Identifying such individuals may allow for more specific strategies to be targeted at care provision for these individuals in the community.
Additionally, the data field ‘type of usual accommodation’ was extracted to enable analysis of presentations by patients who lived in residential aged care facilities.
Data were analysed using IBM SPSS Statistics Version 20 and Microsoft Office Excel 2003.
Results
Overall and primary care type visit volume for Victorians residents in 2012–13
In 2012–13 there were 1,448,171 ED presentations by Victorian residents. Of these, 812,963 (56.1%) were found to be in the low urgency triage category 4 or 5. After applying the exclusion criteria noted above to the low urgency presentations, we calculated the number of ED presentations that could be cared for safely in primary care settings. Of the 812,963 presentations designated at triage category 4 or 5, 108,291 were admitted to the hospital from the ED, a further 60,770 presented by ambulance, 39,120 were referred by a GP and 1517 remained in an ED under treatment for more than 12 hours. This left 603,265 (74.2% of all categories 4 and 5 presentations) that met our definition of a primary care type ED presentation.
Age-specific patterns of primary care type visits over time
An age-specific pattern emerged when examining the proportion of triage category 4 or 5 presentations that met the criteria for designation as a primary care type visit. This pattern was consistent across the 11-year period of our study. The proportion of triage category 4 or 5 ED presentations that met the criteria for primary care type visits was found to be greatest in the youngest age group (0–4 years of age), which consisted of 90% of such presentations (Figure 1). There was a continuous trend for a decreasing proportion of primary care type visits as age increased. The slope of the curve declined most steeply for those aged 65 years and older.
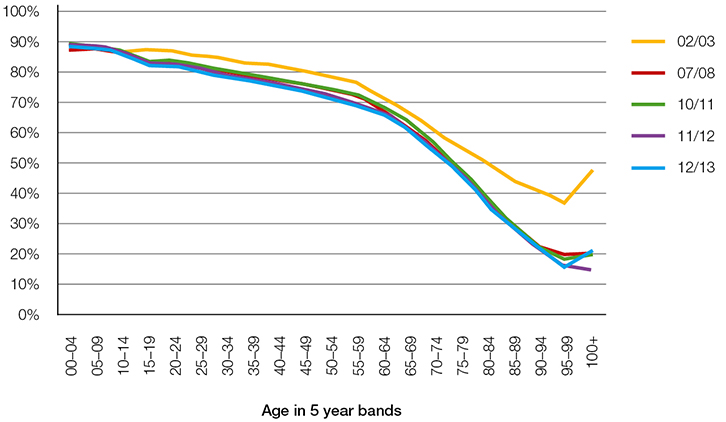 |
| Figure 1. Primary care-type visits as a percentage of triage 4–5 emergency department presentations |
Age-specific patterns of specific primary care type exclusion criteria
Figures 2 and 3 show two of the exclusion criteria from triage category 4 or 5 presentations by age. Figure 2 demonstrates that a very small proportion of younger patients considered to be triage category 4 or 5 were admitted to the hospital. Rates of admission increased slightly beginning at the 15–19 year age group and increased more steeply at the 60–64 age group. This pattern of increase continued until the 95–99 year age group.
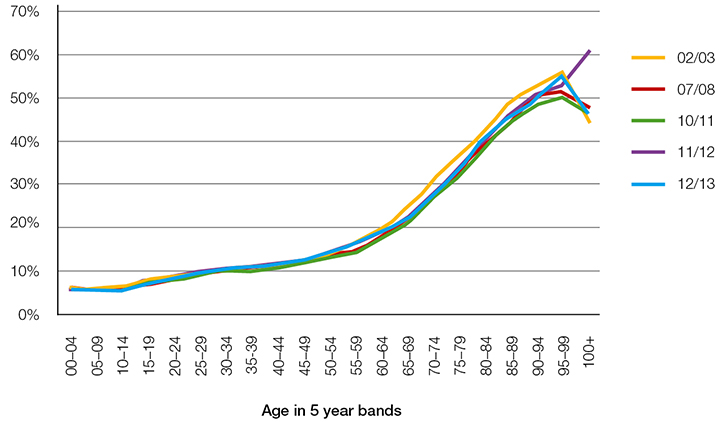 |
| Figure 2. Admitted to hospital as a percentage of triage 4–5 emergency department presentations |
Figure 3 illustrates a similar pattern when exploring ambulance arrivals for triage category 4 or 5 patients. This type of presentation was uncommon in the younger age groups and does not exceed 10% until the 50–54 age group. However, the proportion of such presentations climbed steeply to more than 70% for those aged >90 years. It is important to note that the rate of ambulance presentations for the first year of data examined (2002–03) was very low (<5%) for all age groups. These data were generated prior to a change in policy that provided for community ambulance cover (payments).
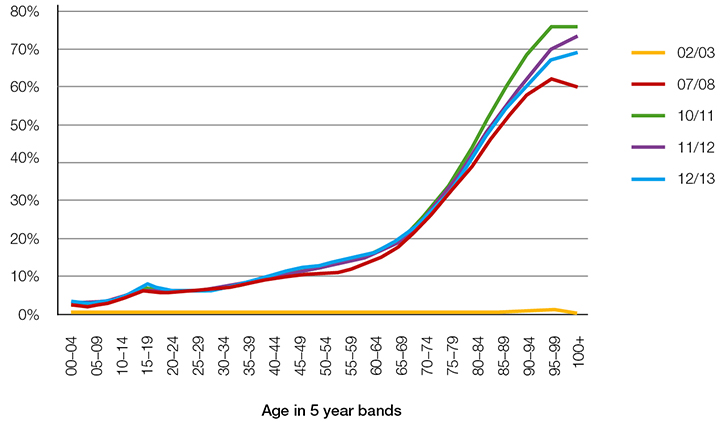 |
| Figure 3. Arrived by ambulance as a percentage of triage 4–5 emergency department presentations |
Primary care type ED presentations by residential aged care facility patients
Of the 296,376 ED presentations for those aged 65 years and older in 2012–13, 24,914 were patients from residential aged care facilities. The proportion of visits classified as triage category 4 or 5 was similar for those who were not from residential aged care facilities and those from these facilities (43.3% versus 39.2%, respectively). Some unique patterns emerged when examining the exclusion criteria for primary care type visits among the triage category 4 or 5 ED presentations for this patient population relative to others aged 65 years and older. Hospital admissions were similar for those who were not from residential aged care facilities and those from these facilities (34% versus 33%, respectively). However, the proportion arriving by ambulance was much greater for patients from residential aged care facilities. Only 32% of patients who were not from residential aged care facilities and categorised as triage category 4 or 5 arrived by ambulance, compared with 74% of those from residential aged care facilities.
The greater proportion of patients from residential aged care facilities who arrived by ambulance resulted in a much smaller proportion of triage category 4 or 5 presentations who met the criteria for primary care type visits. Only 8.5% of patients from residential aged care facilities were primary care type visits, compared with 25% who were not.
Discussion
The marked difference in age in the proportion of triage category 4 or 5 ED presentations that met the criteria for primary care type visits was among the most important findings in the study. This finding is predominantly a result of older patients who arrived by ambulance, or triaged in the ED as non-urgent with subsequent admission to the hospital. These results indicate that it is primarily younger patients who present to the ED with non-urgent conditions and might be most able to safely receive care in a primary care setting. Although the findings in this study are consistent with Siminski’s 2005 study,6 it appears that the magnitude of primary care type ED presentations by children has increased.
The other main finding is the high proportion of patients from residential aged care facilities who arrived by ambulance for triage category 4 or 5 (non-urgent) conditions. This may be the result of a lack of primary care services at the residential aged care facility, a lack of other transportation to the ED or a sense of greater complexity associated with the patient’s problem. Regardless, it appears that there was significant utilisation of ambulance services for low-urgency patients, which may be unnecessary. This should be assessed further.
There has been a recent focus on improving the efficiency of emergency services in Victoria and eliminating unnecessary ambulance use.10,11 Our data suggest greater availability of general practice services in the residential aged care facilities is likely to have a positive impact in this regard. Small studies of such interventions have proven to be effective in decreasing ED presentations.11–13 In addition, for those situations where general practice services for non-urgent conditions are not available, an evaluation at an ED would still be required. The development of alternative transportation strategies other than ambulances would be beneficial in facilitating this.14
Increased patient volumes in the ED have been an ongoing vexation for hospital administrators, physicians, patients and policymakers. The six hospitals added to the VEMD in 2003 may be important, but it does not account for the entire increase in presentations observed.
Multiple efforts have been made to identify specific patients, or groups of patients, presenting to the ED who could be safely cared for in primary care settings.1,3 Understanding the magnitude of the volume of these patients would help to determine the true needs of ED capacity. A current understanding of why patients of different age groups present to the ED, rather than to a general practice, is also essential. Previous studies on this topic have been limited by scope, location or sample size.13,15–18 Additional studies to assess these factors, across all age groups, are urgently needed in Australia.
There have been many attempts to develop systems to identify patients, or groups of patients for whom care could be safely provided in primary care settings. Most of the previous investigators have posited that simply relying on the Australasian triage scale alone is inadequate.3,5 Although no system will have the perfect sensitivity and specificity, we believe the criteria chosen, based on previous work, provide helpful data for those looking to better understand the nature and volume of patient presentations to EDs. Our exclusion of patients who presented by ambulance or spent more than 12 hours in the ED provided a more conservative assessment of those who might be able to safely receive care in less acute settings. However, even with this more conservative approach, the growth of primary care type ED presentations and the burden they place on the healthcare system warrants evidence-based policy actions.
Although several studies have attempted to gain information on the reasons for primary care type ED presentation, these often have not targeted age groups with the highest proportion of primary care type visits. This may be because of a pre-determined focus on Australia’s ageing population, which unintentionally overlooked the magnitude of presentations by paediatrics and young adults to EDs.
Our data show that the greatest impact will be made if children and younger adults with primary care type ED presentation are encouraged to visit general practices. Heretofore, this age group has not been the primary focus of such efforts. Studies to date on ED utilisation by this population have been small, and have usually involved only single sites of care.18–21 Greater attention needs to be placed on understanding the healthcare seeking behaviour of this population to have a greater likelihood of impact on total ED volume of patients.
Limitations
One potential limitation of all studies utilising the VEMD is the change in the number of participating hospitals over time. Although there were additions to the number of hospitals providing data to the VEMD over the time of the study (as noted in the Methods section), all but one was added over a decade ago. The overall trends over time observed in our data are therefore consistent regardless of those additions.
Conclusion
Structural issues frequently have an impact on ED utilisation by those who may safely be cared for in other settings. Availability of after-hours primary care and the availability of same-day general practice appointments have been reported to be problematic. Development and/or expansion of ED-based general practice services may be one of many potential solutions. However, using data to help drive decision-making will ensure the highest likelihood that any investment in health system resources, or health services, will have the greatest potential to result in the desired outcomes.
Authors
Gary Freed MD MPH, Professor, Director, Health Systems and Workforce Unit, Center for Health Policy, Center for Health Policy, The University of Melbourne, Parkville, VIC. gary.freed@unimelb.edu.au
Sarah Gafforini MBA, Research Project Coordinator, Health Systems and Workforce Unit, Centre for Health Policy, Melbourne School of Population and Global Health, Carlton, VIC
Norman Carson MS, Biostatistican, Inner North West Medicare Local, VIC
Competing interests: None.
Provenance and peer review: Not commissioned, externally peer reviewed.