Asthma may be defined clinically as ‘the combination of variable respiratory symptoms (eg wheeze, shortness of breath, cough and chest tightness) and excessive variation in lung function.1 Asthma is common in Australia, with a prevalence of about 10%.2 Most cases of asthma have their onset during childhood and adolescent years. However, asthma may occur for the first time at any age. It is commonly overlooked or misdiagnosed in adults, particularly in those aged 65 years and older.3–5 Adult-onset asthma differs from asthma that first occurs in childhood as it is less well controlled, more likely to be non-atopic and associated with a faster decline in lung function.6,7 It often occurs in response to an external trigger (eg infection, aeroallergens, exposures to occupational or pharmaceutical agents) or a recurrence of childhood asthma. Adult-onset asthma will become more common because of the increasing longevity of the general population.8
Risk factors and triggers
The cause of asthma at any age is unclear. A number of risk factors for the development of adult-onset asthma have been recognised. These include exposure to sensitising or irritant substances, obesity, pharmaceuticals, rhinitis, environmental pollutants, respiratory tract infections and psychological stress.1 In Australia about 10% of adult-onset asthma cases are caused by occupational exposures.9 Indeed, 20–25% of adults with asthma report that their symptoms are worse at work.10,11 A thorough occupational history is important, especially noting the timing of symptoms and presence in the workplace. Initially, symptoms usually abate when not at work (eg weekends), but become more persistent with continued exposure. The onset of symptoms may also be delayed for a number of hours. Therefore, symptoms experienced after work (eg the evening or at night) may represent a delayed response to an occupational exposure. Common exposures include composite woods (eg chipboard, medium-density fibreboards), western red cedar, baker’s flour, epoxy resins, isocyanates and animal dander.12
Obesity and asthma are common disorders in the Australian community, and the latter has become more prevalent in past 20 years.2 Obesity is a well-recognised cause of breathlessness, but has also been found to be a risk factor in the development of asthma in adults,13 especially those with a body mass index (BMI) ≥30 kg/m2.13–15 Aspirin and beta-blocker medications are recognised trigger factors for asthma flare-ups and may unmask an underlying bronchial hyper-responsiveness in some individuals. Beta-blocking eye drops (used in the treatment of glaucoma) may cause wheezing, chest tightness or breathlessness in sensitive individuals.
Rhinitis is a risk factor in the development of asthma in non-atopic and atopic adults.16–18 However, the role of nasal polyposis and chronic rhinosinus disease is less clear. Environmental pollutants, and active and passive tobacco smoking have long been recognised as trigger factors in people with asthma. It is less well recognised that cigarette smoking is a risk factor for the development of asthma in individuals aged 7–33 years.18 There is a significant association between lower respiratory tract infections and the occurrence of adult-onset asthma, although its mechanism is unclear.19 Psychological stress has long been recognised as a trigger factor in asthma and is known to alter inflammatory responses in the airways. Stress has also been shown to have a significant association with the occurrence of asthma and hospitalisation in young adults.20
Clinical aspects – history and physical examination
The clinical presentation of asthma in adults is usually straightforward, and complaints of shortness of breath, cough, wheezing and chest tightness are common.
Coughing in isolation is usually associated with an infection, but the diagnosis of asthma should be considered if it is accompanied by wheezing, particularly at night. Recurrent respiratory tract infection should always raise the possibility of poorly controlled asthma. Breathlessness may be ignored or thought to be due to ‘old age’. As with other age groups, exercise-induced asthma needs to be considered in cases of breathlessness on exertion. Shortness of breath on exertion, and complaints of wheezing and coughing in the night should also alert the clinician to the possible alternative diagnosis of ischaemic heart disease, even in the absence of exercise-induced chest pain or discomfort. Enquiries should be made about precipitating and aggravating factors, and any relieving factors (eg use of bronchodilators). A family or past or concurrent history of atopy and a smoking history should be sought.
Asthma that presents for the first time in cigarette smokers with established chronic airflow limitation may be difficult to detect or differentiate from chronic obstructive pulmonary disease (COPD). Other conditions with similar symptoms need to be considered. This includes cardiac disease, pulmonary hypertension, poor cardiopulmonary fitness and other respiratory conditions. Laryngeal disorders (eg vocal cord dysfunction syndrome) should be considered in those who present with normal expiratory spirometry, appear well and who have an upper airway stridor. Symptoms of asthma may be the presenting features in some other conditions. Nocturnal wheeze may be due to gastro-oesophageal reflux, particularly when associated with cough. Churg-Strauss syndrome may present as severe asthma in adults.
In general, asthma is more likely to be the explanation if the presenting symptoms are recurrent or seasonal, worse at night or in the early morning, prompted by recognised triggers and rapidly relieved by short-acting beta-2 agonists. Auscultatory findings of wheezing, unexplained reductions in forced expiratory volume in 1 second (FEV1), peripheral blood eosinophilia and/or total immunoglobulin E (IgE) level are supportive in making the diagnosis.1 Objective lung function response to inhaled beta-2 agonists remains the gold standard for diagnosis.
A reduction in symptoms, and an increase in FEV1 and peak expiratory flow rate (PEFR) should be expected following standard asthma therapy. Slow responses to appropriate therapy may occur in those with longstanding, poorly managed asthma as a consequence of airway remodelling resulting in a degree of fixed airways obstruction. Slow responses and absence of improvement should prompt a careful review for alternative diagnoses.
Special investigations
Clinical recognition of asthma requires the objective measurement of reversible airflow obstruction (spirometry), demonstrated by an increase in FEV1 of at least 200 ml or ≥12% following inhalation of a short-acting beta-2 agonist (eg salbutamol).1,21 The absence of reversibility does not necessarily disprove the diagnosis – in some longstanding cases, reversibility is slow and may only be demonstrated by an improvement in lung function over a period of 3–4 weeks on standard asthma treatment. In those cases where spirometry is normal or relatively so, bronchial provocation testing should be considered but should only be performed in recognised pulmonary function laboratories.
Induced sputum eosinophil counts and the measurement of expired nitric oxide are undertaken in some centres. However, these are not recommended in routine clinical practice. Spirometry and PEFR remain the first-line measurements in most cases.22 Chest X-rays or computed tomography (CT) chest scans are not needed, but may sometimes be advisable if an alternative diagnosis is being considered.
Overview of management
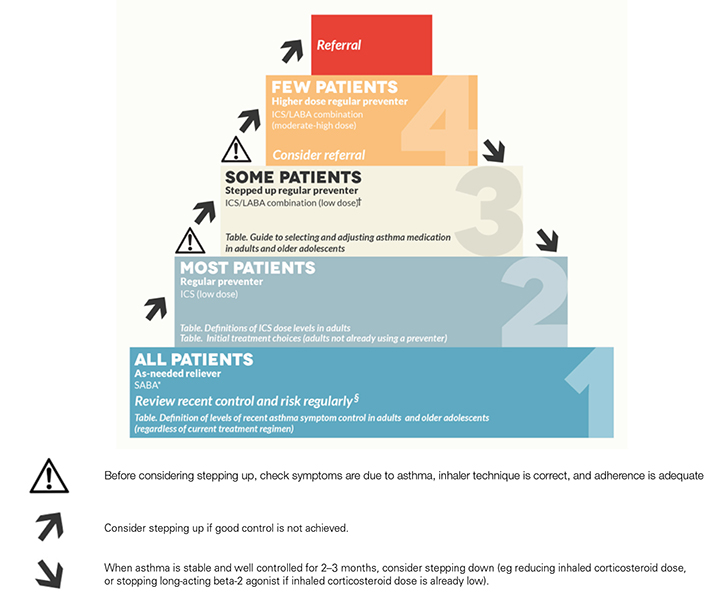 |
Figure 1. Stepped approach to adjusting asthma medication in adults
ICS, inhaled corticosteroid; SABA, short-acting beta-2 agonist; LABA, long-acting beta-2 agonist
*Reliever: short-acting beta-2 agonist (or low-dose budesonide/eformoterol combination for patients using this combination as both maintenance and reliever)
§In addition, manage flare-ups with extra treatment when they occur, and manage exercise-related asthma symptoms as indicated
†Montelukast can be added to inhaled corticosteroid as an alternative to switching to ICS/LABA, but is less effective
Note: PBS status as at April 2015: Montelukast treatment is not subsidised by the PBS for people aged 15 years or over. Special Authority is available for DVA gold card holders, or white card holders with approval for asthma treatments.
Reproduced with permission from the the National Asthma Council Australia from the Australian Asthma Handbook v1.1 |
The management of asthma in adults1 is based initially on confirming the diagnosis, assessing the symptoms and their control, providing asthma education about the underlying nature of the condition and establishing treatment goals. Enquiry should always be made about the patient’s expectations, and instruction must be given about asthma self-management, including acute severe asthma, and an appropriate written asthma action plan provided.
In cases of newly diagnosed symptomatic asthma, regular use of low-dose, inhaled corticosteroids, supplemented by the use of inhaled short-acting beta-2 agonists when symptomatic, is appropriate. If symptoms are severe at initial presentation, a short period of high-dose, inhaled steroids and/or a short course of oral steroids may be needed to gain control. Regular review should follow to assess progress. If treatment is effective in achieving good asthma symptom control, then a gradual reduction in dosage should be possible, with the aim of reaching the minimum that controls symptoms. If the asthma is then only partly controlled with low-dose inhaled corticosteroids, stepping up to an inhaled corticosteroid/long-acting beta-2 agonist combination can be considered (Figure 1). Ongoing review at appropriate intervals is important to ensure good asthma control.
Individuals with occupational asthma should avoid the sensitising or triggering agent, but can otherwise be treated in the same way as those with non-work-related asthma. They may be able to continue their job, providing that exposure to triggers is minimised. This is not possible in some cases. It is recommended that the person be referred to a respiratory specialist who is experienced in managing occupational asthma before considering leaving their job.1
Poor treatment responses should prompt re-assessment of inhaler technique and adherence to therapy. The majority of patients do not use their inhaler devices correctly, and clear instructions and regular technique checks are essential.1,23 Patients do forget their regular preventive therapy from time to time. Strategies should be encouraged to improve adherence.
Loss of asthma control may also be associated with respiratory tract infections and exposure to other known irritants and trigger factors. Education and strategies to avoid these situations should be adopted. Worsening asthma control should prompt an increase in preventive medication (inhaled steroids/long-acting beta-2 agonists). In ongoing, severe asthma, or acute flare-ups, oral steroids should be used. Individuals with asthma that is difficult to treat, or in whom control has not been achieved or who present with severe asthma, require objective assessment of lung function, chest imaging and an evaluation of eosinophil response to treatment. Specialist assessment and management, and hospital admission should be considered when this occurs.
Key points
- Adult-onset asthma is often overlooked or misdiagnosed, especially in older age groups.
- About 10% of adult-onset asthma cases are caused by occupational exposures.
- Diagnosis is based on objective lung function testing.
- Regular preventive therapy is important for those with ongoing symptoms.
- Poor treatment responses should prompt an assessment of inhaler technique.
- Worsening asthma not responding to appropriate therapy, ongoing severe asthma or acute flare-ups should prompt specialist assessment.
Author
Jonathan Burdon AM, MBBS, MD, M Hlth & Med Law, FRACP, FCCP, FACLM, FAICD, Consultant Respiratory Physician, Mercy Private Hospital, East Melbourne, VIC; Chairman, National Asthma Council Australia, South Melbourne, VIC. jburdon@bigpond.net.au
Competing interests: None.
Provenance and peer review: Commissioned, externally peer reviewed.