A rapid rise in the treatment of chronic wounds in the United States has been linked to an ageing population and an increasing incidence of diabetes and obesity.1 In Australia, we also have an ageing population, and increases in the prevalence of obesity and in the management rate of type 2 diabetes.2
We defined chronic skin ulcers as S97 in the International Classification of Primary Care (ICPC-2).3 BEACH data show that between April 2000 and March 2014 there was a significant increase in the management of chronic skin ulcers. The trend was explained by the growing proportion of older patients attending general practice.
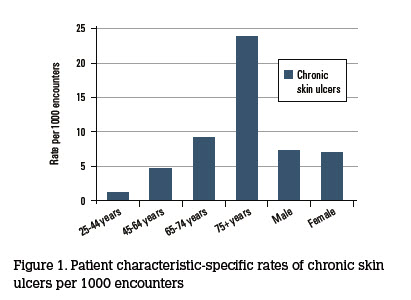 From April 2013 to March 2014, general practitioners (GPs) participating in BEACH managed chronic skin ulcer 686 times, at a rate of 7 per 1000 encounters. Leg ulcers were the most common, accounting for 43% of skin ulcers. Unspecified skin ulcers accounted for another 15%, foot ulcers made up 10% , venous ulcers 8% and pressure sores 5%. Most patients with chronic skin ulcers (59%) were aged ≥75 years, and the condition was managed at a rate of 24 per 1000 encounters with patients in that age group (three times the average rate). There was no difference in rates between male and female patients (Figure 1). In line with the predominance of elderly patients, encounters at residential aged care facilities took place at six times the average rate: 102 per 1000 chronic skin ulcer encounters, compared with 17 per 1000 total encounters. Type 2 diabetes was twice as likely to be managed at skin ulcer encounters than would be expected.
From April 2013 to March 2014, general practitioners (GPs) participating in BEACH managed chronic skin ulcer 686 times, at a rate of 7 per 1000 encounters. Leg ulcers were the most common, accounting for 43% of skin ulcers. Unspecified skin ulcers accounted for another 15%, foot ulcers made up 10% , venous ulcers 8% and pressure sores 5%. Most patients with chronic skin ulcers (59%) were aged ≥75 years, and the condition was managed at a rate of 24 per 1000 encounters with patients in that age group (three times the average rate). There was no difference in rates between male and female patients (Figure 1). In line with the predominance of elderly patients, encounters at residential aged care facilities took place at six times the average rate: 102 per 1000 chronic skin ulcer encounters, compared with 17 per 1000 total encounters. Type 2 diabetes was twice as likely to be managed at skin ulcer encounters than would be expected.
Management of chronic skin ulcers
The primary management of chronic skin ulcers was dressing the wound (Table 1). These dressings were often applied by practice nurses who were involved in the management of 47% of these problems (compared with 5% of all problems in BEACH). Medications were not often recorded. Two-thirds of medications were antibacterial agents. Referrals were uncommon (4 per 100) and pathology tests were not commonly ordered at chronic skin ulcer encounters. Dressing of wounds by practice nurses has not been a claimable Medicare Benefits Schedule item since January 2012. It can be seen from this study that GPs still rely heavily on practice nurses to undertake this work.
Table 1. Treatments for chronic skin ulcers
|
| Treatment | number | Rate per 100 chronic skin ulcer problems | Proportion of each treatment type (%) |
|---|
|
Medications
|
249
|
36.3
|
100.0
|
|
Cephalexin
|
65
|
9.5
|
26.2
|
|
Flucloxacillin
|
17
|
2.5
|
6.8
|
|
Silver sulfadiazine
|
13
|
2.0
|
5.4
|
|
Pathology tests
|
73
|
10.6
|
100.0
|
|
Skin swab C&S
|
31
|
4.6
|
43.1
|
|
Procedures
|
505
|
73.6
|
100.0
|
|
Dressing
|
484
|
70.5
|
95.8
|
Competing interests: None.
Provenance and peer review: Commissioned, not peer reviewed.
Acknowledgements
The authors thank the GP participants in the BEACH program and all members of the BEACH team. Financial contributors to BEACH 2012– 2013: Australian Government Department of Health and Ageing; Australian Government Department of Veterans’ Affairs; AstraZeneca Pty Ltd (Australia); CSL Biotherapies Pty Ltd; Merck, Sharp and Dohme (Australia) Pty Ltd; National Prescribing Service Ltd; Novartis Pharmaceuticals Australia Pty Ltd; Pfizer Australia Pty Ltd.