Case study
A man aged 84 years presented to his general practitioner (GP) with new, recurrent chest pains over the past fortnight, which started 10 weeks after coronary artery bypass graft (CABG) surgery.
The first episode was brief, sharp and severe, occurring suddenly while twisting to empty a heavy bucket and resolving spontaneously within minutes. He subsequently experienced similar, milder pains at rest and with activity. These episodes lasted minutes. He attended his GP 2 hours after one such episode.
The chest pain was central and right-sided, radiating to his jaw, with associated diaphoresis. It was neither pleuritic nor postural. He had recovered well from surgery, having resumed all premorbid activities pain-free. These new pains were different from his previous angina, but were relieved by sublingual nitrates. He had no other past medical history.
Examination was unremarkable, with normal vital signs, well-healed surgical wounds, a stable sternum, no cardiac murmurs or rubs, and clear lungs.
Question 1
What are some causes of chest pain following recent CABG surgery?
Question 2
What history and examination features support these differentials?
Question 3
What are the important features of the initial assessment and management of this patient?
Answer 1
Causes of chest pain following recent CABG surgery include:1,2
- Musculoskeletal causes (most common)
- Myocardial ischaemia (graft stenosis/occlusion)
- Pericarditis (eg Dressler’s syndrome)
- Pulmonary embolus
- Aortic dissection
- Sternal wound infection or non-union
- Pneumonia
- Gastritis.
Answer 2
Although musculoskeletal pain is most common,2 it is always expedient to have a high index of suspicion of less common but more severe causes. In this case the patient’s response to nitrates and associated diaphoresis are suggestive of cardiac ischaemia, even if unlikely after CABG surgery. Features of dissection include the initial sharp, tearing pain. Absence of a postural component makes pericarditis less likely, and absence of cough, dyspnoea or pleurisy makes pulmonary embolus or pneumonia less likely.
Important features on physical examination could include a tachycardia (pulmonary embolus, infection), a blood pressure differential (aortic dissection), cardiac rub (pericarditis), a new murmur (acute aortic regurgitation from retrograde dissection), signs of congestive cardiac failure (due to myocardial ischaemia or tamponade caused by dissection), sternotomy infection, sternal instability, epigastric tenderness (gastritis) and altered breath sounds (pneumonia, cardiac failure). Haemodynamic instability would be a crucial finding.
Answer 3
If the patient is haemodynamically stable, a thorough history and examination should be obtained. An office electrocardiogram (ECG) could assess for new ischaemic changes. Further investigations could include creatine kinase/troponin (ischaemia), full blood count (anaemia, leucocytosis), renal function (before possible computed tomography pulmonary angiography), as well as a chest X-ray (consolidation, mediastinal widening, congestion).
As this patient had new atypical chest pain with some concerning features, it was most appropriate to first contact his cardiologist or cardiac surgeon.2 If this was not possible, the patient could have been referred directly to the emergency department.
Case continued
The GP was concerned about the severe, sharp, atypical nature of the pain and its delayed-onset after surgery. He liaised with the patient’s cardiologist and the patient was hospitalised immediately. Admission ECG showed a pre-existing right bundle branch block. Troponin was slightly elevated at 0.05 µg/L and chest X-ray was unremarkable. Coronary angiography revealed patent grafts. An initial left ventriculogram suggested external aortic compression (Figure 1). An aortogram revealed a dissection of 8.9 cm in diameter from the aortic root base, compressing the true aortic lumen (Figure 2).
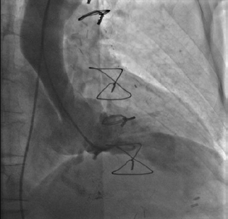 |
Figure 1. Left ventriculogram showing
unusual aortic root contour with
apparent external compression |
|
 |
Figure 2. Aortogram showing contrast
entering a large false lumen, maximal
transverse diameter 8.9 cm |
|
Question 4
What causes aortic dissection after CABG surgery?
Answer 4
Aortic dissection involves a breach in
the aortic lining, often arising from hypertension or trauma. This creates a ‘false’ longitudinal lumen in the aortic wall. Dissections are typically classified as either Stanford type A, which involve the ascending aorta, often extending to the arch and descending aorta, and type B, which arise distal to the aortic arch with no ascending aorta or arch involvement (Figure 3). Type B dissections usually respond to pharmacological management of hypertension. Type A dissections are an acute surgical emergency.3
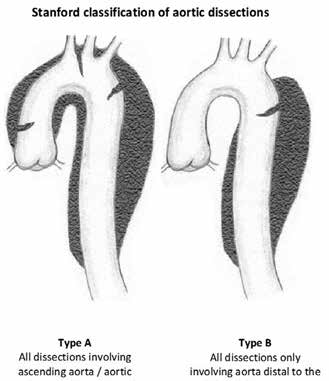 |
| Figure 3. Stanford classification of aortic dissections |
Aortic dissection is a rare, serious complication after CABG surgery (0.05% incidence).4 It can occur intra-operatively, immediately post-operatively or even years later. Presenting symptoms vary and include chest pain and dyspnoea (due to tamponade or acute aortic regurgitation). Alternatively, it may be incidentally found on chest or coronary imaging. Urgent surgery usually involves replacement of part of the ascending aorta and possibly the aortic valve.4
Case continued
The patient had urgent cardiac surgery. Intra-operative diagnosis was a sub-acute type A aortic dissection, originating from a proximal graft anastomosis. The aortic root and proximal ascending aorta were replaced and the graft anastomosis reimplanted.
Conclusion
This case illustrates the diagnostic dilemma of chest pain after CABG surgery, where a GP may reasonably assume cardiovascular causes of chest pain are unlikely. Although aortic dissection is a rare surgical complication, this highlights the need for prompt referral if there is any suspicion of a cardiovascular cause of chest pain after CABG surgery.
Competing interests: None.
Provenance and peer review: Not commissioned, externally peer reviewed.
References