General practice has always been the cornerstone of Australia’s healthcare system. Almost all Australians (85%) visit a general practitioner (GP) at least once in any given year,1 and GPs act as gatekeepers for access to secondary medical services.
We sought to gain a bird’s eye view of major changes over a quarter of a century in the characteristics of the GP workforce, the patients they see and the complexity of their encounters with patients. We compared results of comparable data elements from national surveys of practising GPs and their clinical activity in three periods:
- the Australian Morbidity and Treatment Survey (AMTS) 1990–912
- the Bettering the Evaluation and Care of Health (BEACH) program 2001–03
- BEACH 2013–15.1
In 1990–2015, Australia’s population increased by 37.5% (17.1 million to 23.5 million)3 and the number of claims for GP service items from Medicare Benefits Schedule (MBS) grew by 65.5% (from 83.0 million to 137.4 million).2,4 The proportion of the population aged 65 years and older rose from 11.1% in 1990 to 15.1% in 2015.3 Therefore, in 2015, there was one more Medicare-claimed GP visit per head of population (5.8 visits) than in 1990–91 (4.8).
Methods
A re-analysis of data from the AMTS and BEACH program was conducted. Methods for AMTS and BEACH are similar and have been described in detail elsewhere.2,5 Both were cross-sectional, encounter-based studies of GP clinical activity using national random GP samples; each GP recorded encounter details on structured paper forms. Where more detail was available in the BEACH dataset than in AMTS, BEACH data were re-grouped to be comparable with the AMTS. Significance of differences in GP characteristics was tested with chi-square statistic. Clinical significance was set at P <0.05. Differences in patients’ characteristics and the content of encounters were determined by non-overlapping 95% confidence intervals with adjustment for the cluster sample design.
Results
Each of the samples was assessed and found to be representative of general practice in Australia at the time of data collection.1,2 In 1990–91, female GPs accounted for 20% of participants, but this figure grew to 43% of participants by 2013–15 (Figure 1). A large proportion of this growth occurred during the 1990s. With women now representing 50.6% of commencing medical students,6 feminisation of the GP workforce is likely to continue. This will have significant policy implications as their work pattern is very different from that of male GPs.7
Older GPs (>55 years of age) represented only 18% of participants in 1990–91, but 46% in 2013–15, the majority of change occurring over the most recent 15 years. This trend may reverse because of the large number of general practice registrars entering practice in the future.
Practices were smaller in 1990–91; one in four (26%) GPs was in solo practice and 33% in practices of four or more GPs. In 2013–15, only 9% of GPs worked solo and 77% were in practices of four or more GPs (Figure 1). Further, between 2001–03 and 2013–15, the proportion of GPs in large practices (≥10) more than doubled from 11% to 27% (results not tabled).
The decrease in the number of small practices scattered in the community may have implications for patients’ access to GPs.
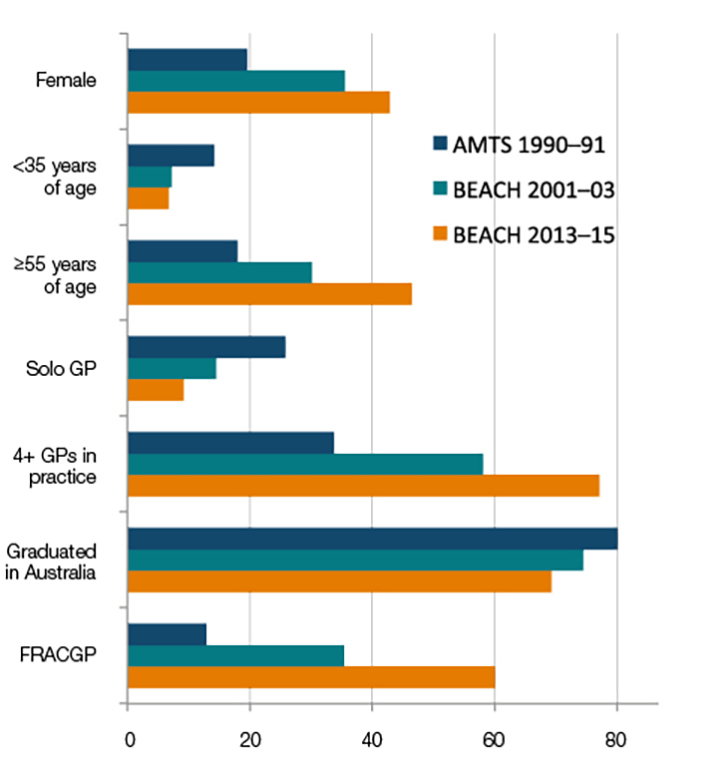
Figure 1. Signifcant changes in characteristics of GP participants
FRACGP, Fellow of the Royal Australian College of General Practitioners;GP, general practitioner
The proportion of GP participants who graduated in Australia decreased from 80% to 69%, whereas those who obtained the Fellowship of The Royal Australian College of General Practitioners (FRACGP) grew from 13% to 60% over the 25 years. The increased percentage of trained GPs with mandatory continuing professional development should result in continuing improvement in the quality of patient care.
Patients
There were significant decreases in the proportion of GP workload accounted for by each of the five younger patient age groups under 45 years. There were significant increases in the proportion of the three older age groups (>45 years of age), such that the proportion of encounters with patients aged 45 years and older rose from 47.2% of encounters in 1990–91 to 59.2% in 2013–15 (Figure 2).
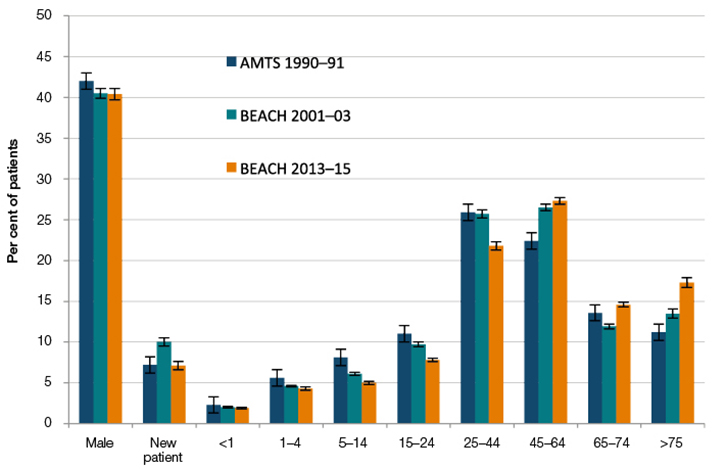
Figure 2. Changes in characteristics of patients at encounters (with 95% confidence intervals)
Workload
The complexity of GP–patient encounters has increased, with a significant stepwise increase in the number of reasons for encounter presented by patients to GPs over the three periods. There was also a significant increase in the average number of problems managed, but all this growth occurred between 2001–03 (148 per 100 encounters) and 2013–15 (161 per 100 encounters), with no growth in the earlier decade. On average, GPs are managing fewer new and acute problems, but more chronic problems (as defined by O’Halloran et al)8 per encounter (Figure 3). Increasing numbers of older patients with complex disease will require redirection of resources to this patient population group.
With more problems managed, one would expect more management actions of all types. However, prescriptions decreased by 15% from 100 per 100 encounters in 1990–91 to 85 per 100 encounters in 2001–03, then stayed steady. The decrease could be the result of changes in prescribing behaviour by GPs (eg decreased antibiotic prescribing for upper respiratory tract infection [URTI]),9 but also to increased numbers of combination products, requiring one prescription (not two), and movement of drugs off the Pharmaceutical Benefits Scheme (PBS) to over-the-counter purchase. Clinical treatments (eg advice, education, counselling) rose by more than 50% from 1990–91 (25.1 per 100 encounters) to 2001–03 (39.6 per 100 encounters), with no further change in 2013–15 (37.6 per 100 encounters). Procedures undertaken by GPs were steady in 1990–91 (14.8 per 100 encounters) and 2001–03 (14.7 per 100 encounters), but then significantly increased to 18.5 per 100 encounters in 2013–15.
Referrals to medical specialists and allied health professionals increased significantly across the three study periods (Figure 3), the larger growth in both occurring since 2001–03. In particular, referrals to allied health professionals more than doubled from 2001–03 to 2013–15, probably in response to changes in MBS coverage of some of these services and an increase in management of chronic conditions. This trend is likely to continue with an ageing population.
The likelihood that the GP would order one or more pathology tests at an encounter rose by more than 50% from 2001–03 to 2013–15, perhaps reflecting the increased number of problems (and specifically chronic problems) being managed. There was also a 70% increase in the likelihood of ordering imaging at an encounter, but the major proportion of growth occurred in the more recent years. The increased likelihood of testing may also be due to the need to monitor for an ever-increasing number of patients with diagnosed chronic disease.
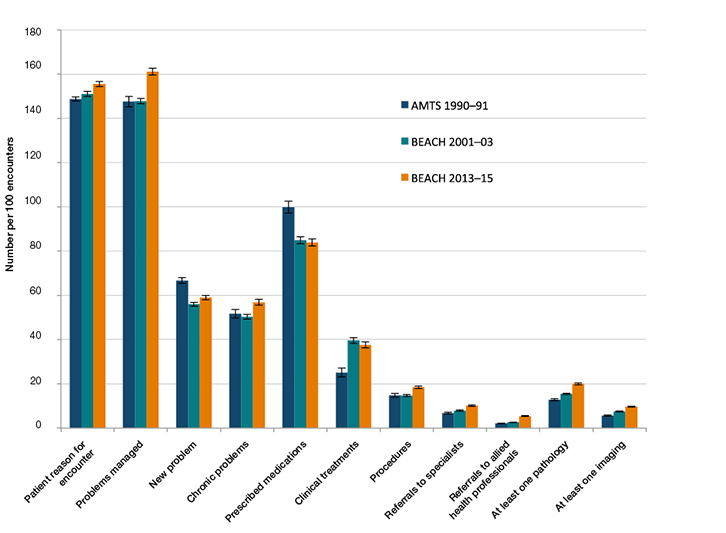
Figure 3. Significant changes in content of encounters
Discussion
Clearly, the GP workforce, patients at GP encounters and content of encounters have changed over the past 25 years. GPs’ clinical work has become more centred on care of older people, more frequent management of chronic conditions, more clinical and therapeutic procedures, and more referrals and test ordering. However, as demonstrated in an earlier paper in this series, this is not at the expense of the care of children whose visit rate did not change between 2000–03 and 2012–15.10
Authors
Helena Britt BA, PhD, Professor of Primary Care Research, School of Public Health, Sydney Medical School, University of Sydney, NSW. helena.britt@sydney.edu.au
Graeme C Miller MBBS, PhD, FRACGP, Honorary Associate Professor and (formerly) Medical Director of the BEACH program, School of Public Health, Sydney Medical School, University of Sydney, NSW
Lisa Valenti BEc, MMed Stat, Honorary (and formerly) Senior Research Analyst for the BEACH program, School of Public Health, Sydney Medical School, University of Sydney, NSW
Joan Henderson BAppSc (HIM) (Hons), PhD, Honorary Senior Research Fellow, School of Public Health, Sydney Medical School, University of Sydney, NSW
Clare Bayram BAppSc (HIM) (Hons), PhD, Honorary Research Fellow and (formerly) Project Manager of the BEACH program, School of Public Health, Sydney Medical School, University of Sydney, NSW
Julie Gordon BAppSc (HIM) (Hons), PhD, Research Fellow, School of Public Health, Sydney Medical School, University of Sydney, NSW
Competing interests: None.
Provenance and peer review: Commissioned, externally peer reviewed.