Case
A student of Asian descent, 27 years of age, presented to his general practitioner (GP), reporting a three-day history of erythema, swelling and purpuric rash on his hands and feet. The erythema had appeared suddenly on his palms and subsequently spread and evolved to include purpura on his hands and soles. The purpuric lesions were painful but not pruritic. He described a prodromal illness in the week prior that was associated with mild arthralgias. He had no remarkable medical history or known allergies, and was not on any regular medications.
On examination, the patient was afebrile and appeared well systemically. He had erythema and purpuric papules up to 1 cm in diameter on his hands and soles. The rash was non-palpable and well demarcated at the wrists and ankles. Petechia were visualised on the hard palate. There was no hepatosplenomegaly or lymphadenopathy. Blood samples were sent for haematology, biochemistry and inflammatory markers, which returned a mild neutropaenia but were otherwise within normal limits.
Given the patient’s systemic fitness and unremarkable blood test results, the patient was discharged without a clear diagnosis to be managed expectantly for review in 48 hours. On review, he remained well but had larger areas of involved skin, with more purpura appearing in affected areas. Photos were taken (Figures 1, 2) and sent to a local dermatologist. The patient was sent home once again pending specialist advice.

Figure 1. Palmar purpure
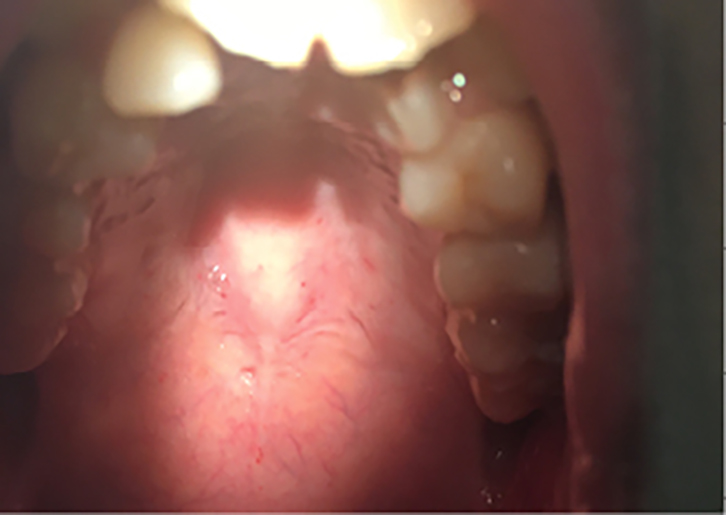
Figure 2. Palate petichiae
Question 1
What are the possible diagnoses of this purpuric rash?
Question 2
What is the probable diagnosis in this case?
Question 3
How is the diagnosis confirmed?
Answer 1
Purpuric papules on the hands, feet and mucosa can arise from a wide differential list including infectious, haematological, vasculitic and rheumatological conditions:
- thrombocytopenic purpuric syndromes (eg idiopathic thrombocytopenic purpura [ITP], thrombotic thrombocytopenic purpura [TTP])
- cutaneous small vessel vasculitis (eg Kawasaki disease, leukocytoclastic vasculitis)
- hand, foot and mouth disease (Coxsackie virus)
- papular-purpuric gloves and socks syndrome (PPGSS)
- atypical measles
- meningococcemia
- Rickettsial diseases
- haematological malignancy (eg leukaemia)
- Gianotti–Crosti syndrome.
Answer 2
The evolution, morphology (purpura), distribution (acral) and infective prodrome of the patient’s rash make viral PPGSS the most likely diagnosis, despite this being rare.1 Gianotti–Crosti syndrome, an important differential in post-infective papular eruptions, is less likely in an adult (most common in young children) in the absence of more widespread distribution (face, buttocks) and lymphadenopathy.2
PPGSS is seen most commonly in young adults in late spring and summertime, and is spread via respiratory secretions. Incubation periods range from four to 14 days followed inconsistently by a prodrome of fevers, headaches, malaise, arthralgias and myalgias. These self-limiting symptoms can precede cutaneous lesions by up to one week.3 Similar lesions (most commonly petechia and erosions) may be observed at other sites, including oral and genital mucosa.4
In the literature, around 50% of PPGSS cases have been attributed to parvovirus B19. The remainder of cases are largely shared between hepatitis B virus (HBV), Epstein–Barr virus (EBV), Varicella zoster, human Herpes viruses (HHPs) 6 and 7, cytomegalovirus (CMV), human immunodeficiency virus (HIV), rubella and measles.5
Answer 3
PPGSS diagnosis is made predominantly on the basis of the clinical features. It should be strongly suspected of any well-demarcated acral purpuric rash.6 Serum testing (polymerase chain reaction [PCR] or enzyme-linked immunosorbent assay [ELISA]) for IgM can be used to confirm clinical suspicion. IgM peaks in the first week, declines during the subsequent four weeks and can be detectable until three months after infection.7
Seroprevalence increases with age, with a seropositivity rate of greater than 85% in the elderly, which explains why symptoms are much less common in adults than in children.8
Case continued
On the dermatologist’s advice, the patient attended for additional blood testing the next day. These tests included:
- serology: HBV, EBV, parvovirus B19, Varicella zoster, HHVs 6 and 7, CMV, HIV, rubella and measles
- antinuclear antibodies (ANAs)
- perinuclear anti-neutrophil cytoplasmic antibodies (pANCA)
- cytoplasmic anti-neutrophil cytoplasmic antibodies (cANCA)
- complement levels (C3, C4).
A few days later, results revealed elevated parvovirus B19 immunoglobulin M (IgM) titres, confirming the diagnosis of PPGSS. The patient was promptly informed of this over the phone. He was advised of the expected disease course and reasons to return.
Question 4
What is the pathophysiology of this skin manifestation?
Question 5
What is the expected disease course?
Answer 4
Pathogenesis is most likely to be due to immune complex deposition. This is supported by histopathology that demonstrates lymphocytic perivascular infiltrates, oedema of the papillary dermis and extravasation of red blood cells. Direct immunofluorescence shows IgM and C3 deposits at the dermo-epidermal junction and in the walls of the papillary dermal vessels.9
Answer 5
In immunocompetent populations, the eruption generally clears with variable desquamation in less than two weeks with no specific treatment.10 Those with haemoglobinopathies and immunosuppression should be closely monitored for uncommon complications, including chronic arthropathy, anaemia and aplastic crisis.11 Pregnant women should be promptly referred to the emergency department, as there is a risk of miscarriage or hydrops fetalis.12 Rare complications such as hepatitis, encephalitis, non-occlusive bowel infarction, amegakaryocytic thrombocytopenia, myositis and heart disease have also been described.13
Case continued
At one-week follow-up, the patient’s clinical condition was unchanged.
Key points
- Diagnosis relies principally on recognition of characteristic clinical features, confirmed by serological testing.
- PPGSS manifests as non-palpable purpura, which distinguishes it from vasculitic causes, which typically produce palpable purpura.
- Around 50% of PPGSS cases are caused by acute parvovirus B19 infection.
- No specific treatment is required for most patients, who generally recover in two weeks.
Author
Thomas Stewart BBioMedSc (Hons), MBBS, General Practice Registrar, Kogarah Railway Medical Centre, general practice, Kogarah, NSW. thomas_stewart@live.com
Competing interests: None.
Provenance and peer review: Not commissioned, externally peer reviewed.