Injuries are a leading cause of morbidity and mortality for young people, who engage in more road risks and are over-represented in road accidents – those aged between 18 and 25 years account for 21% of Victorian driver deaths.1–5 Clinicians have a potential role in reducing traffic injuries through preventive counselling across a range of high-risk behaviours. However, there is minimal research investigating this potential.6,7
Road accidents involving youth are attributed to a combination of inexperience and hazardous behaviours, such as driving under the influence of alcohol, speeding, carrying passengers, and using mobile phones while driving.8–10 Victoria’s graduated licensing laws allow a learner’s permit at 16 years of age and a probationary licence at 18 years of age.11 The probationary period lasts for four years and includes a limit of one peer passenger during the first year, zero blood alcohol concentration and no mobile phone use (including hands-free).11 Despite the effectiveness of graduated licensing in reducing crashes, additional approaches targeting youth are needed.6,12,13
Population studies reveal youth driving at high risk are more likely to engage in other risky behaviours, including substance use, unsafe sex and anti-social behaviour.2,14–16 Problem behaviour theory proposes a relationship between different problem behaviours, and that a combination of personality and social environment can lead to an individual engaging in multiple risks.17 Risk-taking youth are likely to become involved with a range of high-risk activities, including dangerous road behaviours.2,15 Hence, a preventive framework addressing a range of unsafe behaviours could potentially improve health outcomes.6,12
Primary care is a valuable setting for adolescent preventive services as most males and females attend at least annually.18,19 Practice guidelines from the US recommend annual preventive health screening and counselling for young people. However, few studies have examined their effectiveness; one demonstrated improved seatbelt and helmet use.20,21 While clinicians support discussing road safety, counselling is often limited to seatbelt and alcohol use.22
In Australia, adolescents most commonly attend general practice with physical issues, and females attend more frequently than males.19 Australian guidelines recommend opportunistic preventive screening using the ‘HEADSSS’ framework. This involves asking young people about home, education, activities, drugs, sexuality, suicide and safety to identify high-risk behaviours and facilitate preventive counselling.23,24 The HEADSSS framework offers an opportunity to integrate discussions of road-related risks.
A stratified cluster randomised controlled trial (RCT), the ‘prevention access and risk taking in young people’ (PARTY) project, was conducted to investigate the impact of screening and counselling in young people (aged 14–24 years) for health risks in general practice.25,26 Young people presenting to 40 Victorian general practices in the trial self-reported risk-taking behaviours, including road risks, at baseline.26 This paper investigates the trial baseline data for:
- the frequency of and types of road risks undertaken by young people
- the association of road risks with other health risks
- other characteristics of youths reporting hazardous road-related activities.
Methods
Design
A cross-sectional analysis of data from the PARTY project was undertaken.25 A detailed description of the project and results have been published elsewhere.25,26 Data were collected between June 2007 and August 2010.26
One of the inclusion criteria for practices was that they needed to have at least one interested clinician, general practitioner (GP) or practice nurse. Health-risk behaviours in patients aged 14–24 years attending a general practice for any reason were assessed by computer-assisted telephone interview (CATI). Patients were excluded if they did not speak English, were severely unwell or were immature minors who were unable to get parental consent.25
Forty-two general practices across Victoria were stratified by socioeconomic indexes for areas (SEIFA) classifications into advantage/disadvantaged areas, and by practice billing method, and then randomised. Following randomisation, two practices withdrew, which resulted in 19 intervention (53 clinicians, 377 patients) and 21 comparison (79 clinicians, 524 patients) practices.25 Intervention practices received nine hours of interactive training on youth-friendly care, discussing health risks (using HEADSSS) and motivational interviewing. These practices also had two practice visits embedding risk screening processes.25 The comparison arm received one three-hour seminar on youth-friendly care.25
Procedure
Eligible patients were initially invited by clinicians, post-consultation, to provide contact details to researchers; however, clinicians inconsistently approached eligible patients, and research assistants in waiting rooms later undertook this procedure.25 Interviewers phoned participants to obtain full consent and then perform a one-hour CATI.25 Research assistants and interviewers were blind to the practice allocation and participants were not informed by researchers. The CATI data from both trial arms was analysed in the present study. Ethics approval was obtained from the University of Melbourne’s Human Research Ethics Committee (Ethics ID 0709280).25 Figure 1 outlines the procedures for the PARTY project up to completion of the CATI.
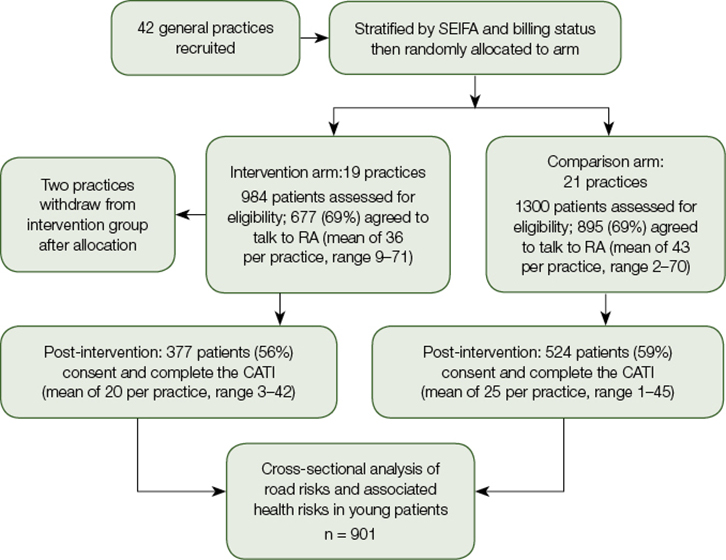
Figure 1. The PARTY project procedure outlining data collection for cross-sectional analysis in this study.
CATI, computer-assisted telephone interview; RA, research assistant; SEIFA, socioeconomic indexes for areas
Measures
Researchers designed the road risk interview items on the basis of common behaviours placing youth at risk of a crash or injury.8,9,25 Participants were asked about seven selected behaviours using a self-report, six-point categorical scale (‘never’, ‘rarely’, ‘sometimes’, ‘most of the time’, ‘always’ or ‘not applicable’).25 Safety behaviours included wearing a seatbelt when driving and helmet use when riding a bicycle or motorcycle. Risky behaviours included:25
- exceeding the speed limit by 10 km/hour or more
- driving while using a mobile phone for calls and text messages
- driving under the influence of alcohol or drugs
- travelling in a car with other people under the influence of alcohol or drugs.
A binary outcome for road risk was created where ‘no risk’ was defined as never having the risk (‘never’ or ‘not applicable’), and always following safety recommendations (‘always’ or ‘not applicable’), and ‘risk’ was defined as all other responses.25
Binary outcomes (‘no risk’ versus ‘risk’) were also created for risky use of tobacco, alcohol, cannabis and other illicit drugs, and for risk of unplanned pregnancy or sexually transmissible infections (STIs).25 Emotional distress was defined by a Kessler Psychological Scale (K10) score of greater than 20.27 The demographic characteristics of youths engaging in one or more road risks were also analysed.28
Statistical analyses
Statistical analysis was performed using Stata Statistical Software 12. Multi-variable logistic regression and Pearson’s chi-squared tests were used to investigate the association of road risks with other variables.29 All analyses were adjusted for trial arm, SEIFA index, practice billing status, patient recruitment method, and clustering and patient age and gender as appropriate.25
Results
Demographic characteristics
The study comprised 901 young people, of whom 900 completed all road-risk items (males = 219; females = 681. Age ranges were 14–17 years (n = 223) and 18–24 years (677). Most of the participants were born in Australia and attended a general practice in an area of advantage.
Proportion engaging in road risks
A large proportion (79%) of young people reported engaging in one or more road risks (Table 1). Males had higher rates for certain behaviours, including not using helmets, speeding, and driving under the influence of alcohol or drugs. When compared with the 14–17 age group, those in the 18–24 age group had higher risks for:
- failure to use a seatbelt as a passenger
- failure to always use a helmet
- speeding
- mobile phone use while driving
- driving under the influence of alcohol or drugs
- travelling with people under the influence of alcohol or drugs.
Table 1. The proportion of road safety risks in young patients by gender and age
|
Prevalence of road safety risks
|
n (%)
|
Males n (%)
|
Females n (%)
|
Age 14–17 n (%)
|
Age 18–24 n (%)
|
|
Total sample
|
900
|
219
|
681
|
223
|
677
|
|
No seat belt passenger
|
86 (9.56)
|
24 (10.96)
|
62 (9.10)
P = 0.417†
|
33 (14.80)
|
53 (7.83)
P = 0.002
|
|
No seat belt driver
|
26 (2.89)
|
7 (3.20)
|
19 (2.79)
P = 0.755
|
6 (2.69)
|
20 (2.95)
P = 0.838
|
|
No helmet*
|
119 (13.24)
|
52 (23.74)
|
67 (9.85)
|
43 (19.28)
|
76 (11.24)
|
|
|
|
|
P <0.001
|
|
P = 0.002
|
|
Speeding
|
389 (43.22)
|
115 (52.51)
|
274 (40.23)
|
26 (11.66)
|
363 (53.62)
|
|
|
|
|
P = 0.001
|
|
P <0.001
|
|
Mobile phone use while driving
|
364 (40.44)
|
82 (37.44)
|
282 (41.41)
|
18 (8.07)
|
346 (51.11)
|
|
|
|
|
P = 0.298
|
|
P <0.001
|
|
Travelling with people under the influence of alcohol or drugs*
|
498 (55.39)
|
133 (60.73)
|
365 (53.68)
P = 0.068
|
86 (38.74)
|
412 (60.86)
P <0.001
|
|
Driver under the influence
of alcohol or drugs
|
115 (12.78)
|
41 (18.72)
|
74 (10.87)
P = 0.002
|
5 (2.24)
|
110 (16.25)
P <0.001
|
|
*Total responses 899 due to missing female response; †P values calculated using Pearson’s chi-squared test
|
Association of road risks with health risks
Table 2 shows road risk-taking was significantly associated with tobacco, alcohol and other substance use, and with unprotected sex, but not with emotional distress.
Table 2. Association between health risks and road risks performed using multivariable logistic regression
|
Health risk
|
Total
|
One or more road safety risks n (%)
|
Unadjusted odds
ratio (95% CI)
|
P
|
Adjusted odds
ratio (95% CI)*
|
P
|
|
Smoking risk in past 12 months
|
|
No risk
|
546
|
401 (73.44)
|
1.0
|
|
1.0
|
|
|
At risk
|
350
|
304 (86.86)
|
2.390 (1.696–3.367)
|
<0.001
|
2.213 (1.579–3.101)
|
<0.001
|
|
Drinking risk in past 12 months
|
|
No risk
|
125
|
67 (53.60)
|
1.0
|
|
1.0
|
|
|
At risk
|
775
|
642 (82.84)
|
4.179 (2.855–6.116)
|
<0.001
|
3.082 (1.986–4.782)
|
<0.001
|
|
Cannabis use in past 12 months
|
|
No risk
|
712
|
536 (75.28)
|
1.0
|
|
1.0
|
|
|
At risk
|
188
|
173 (92.02)
|
3.787 (2.247–6.383)
|
<0.001
|
3.309 (1.905–5.749)
|
<0.001
|
|
Illicit drug use in past 12 months
|
|
No risk
|
754
|
574 (76.13)
|
1.0
|
|
1.0
|
|
|
At risk
|
146
|
135 (92.47)
|
3.849 (1.830–8.094)
|
0.001
|
2.704 (1.313–5.566)
|
0.008
|
|
Sexual health risk in past three months
|
|
No risk
|
247
|
148 (59.92)
|
1.0
|
|
1.0
|
|
|
At risk
|
646
|
556 (86.07)
|
4.132 (2.835–6.023)
|
<0.001
|
2.660 (1.705–4.151)
|
<0.001
|
|
At risk for mental health in past month
|
|
No risk
|
635
|
492 (77.48)
|
1.0
|
|
1.0
|
|
|
At risk
|
264
|
216 (81.82)
|
1.308 (0.876–1.953)
|
0.184
|
1.276 (0.829–1.966)
|
0.260
|
|
*Adjusted for age, gender, cluster, intervention arm, practice billing status, socioeconomic indexes for areas (SEIFA) and method of recruitment
|
Characteristics of the young people engaging in road risks
Table 3 presents the demographic characteristics of participants engaging in one or more safety risks. There was no overall significant association of road risks with gender. Those aged 14–24 years who were working were more likely to report road risks than those who were not working. Participants born outside Australia were significantly less likely to report road risk behaviours.
Table 3. The characteristics of young people engaging in road risks using multivariable logistic regression
|
Characteristics
|
Total
|
One or more road safety risks n (%)
|
Unadjusted odds
ratio (95% CI)
|
P
|
Adjusted odds
ratio (95% CI)*
|
P
|
|
Age
|
|
|
|
|
|
|
|
14–17
|
223
|
133 (59.64)
|
1.0
|
|
1.0
|
|
|
18–24
|
677
|
576 (85.08)
|
3.859 (2.731–5.453)
|
<0.001
|
4.227 (2.936–6.087)
|
<0.001
|
|
Gender
|
|
|
|
|
|
|
|
Male
|
219
|
176 (80.37)
|
1.0
|
|
1.0
|
|
|
Female
|
681
|
533 (78.27)
|
0.880 (0.574–1.350)
|
0.549
|
0.819 (0.531–1.264)
|
0.359
|
|
Country of birth
|
|
|
|
|
|
|
|
Australia
|
756
|
606 (80.16)
|
1.0
|
|
1.0
|
|
|
Other
|
143
|
102 (71.33)
|
0.616 (0.440–0.861)
|
0.006
|
0.436 (0.275–0.691)
|
0.001
|
|
Employment and studying
|
|
Not working
|
302
|
204 (67.55)
|
1.0
|
|
1.0
|
|
|
Working
|
596
|
504 (84.56)
|
2.632 (1.864–3.716)
|
<0.001
|
1.783 (1.200–2.649)
|
0.005
|
|
Not studying
|
288
|
251 (87.15)
|
1.0
|
|
1.0
|
|
|
Studying
|
610
|
457 (74.92)
|
0.440 (0.310–0.626)
|
<0.001
|
0.802 (0.559– 1.152)
|
0.225
|
|
Neither working nor studying
|
65
|
50 (76.92)
|
1.0
|
|
1.0
|
|
|
Working and studying
|
373
|
303 (81.23)
|
1.299 (0.715–2.357)
|
0.380
|
1.537 (0.776–3.046)
|
0.211
|
|
Socio-Economic Indexes for Areas (SEIFA)
|
|
Advantage
|
750
|
595 (79.33)
|
1.0
|
|
1.0
|
|
|
Disadvantage
|
150
|
114 (76.00)
|
0.825 (0.567–1.200)
|
0.305
|
0.970 (0.651–1.444)
|
0.876
|
|
*Adjusted for age, gender, cluster, intervention arm, practice billing status, SEIFA and method of recruitment
|
Discussion
This cross-sectional study examined road risk behaviours among young people attending primary care, and associations with other health risks and demographic characteristics, using data collected during a large cluster RCT in general practice.1–4 Although clinical guidelines recommend injury prevention counselling, this study is one of the first to describe road risks among youth attending Australian general practice.21,23
Most of the participants reported engaging in one or more road risks, commonly speeding, mobile phone use while driving, and travelling with people under the influence of alcohol or drugs. These behaviours were higher among those aged 18–24 years, which coincides with the probationary licensing period in Victoria. The proportion of youth under the age of 18 years, and hence ineligible for probationary licences, engaging in risky driving behaviours is concerning. Five reported driving under the influence of alcohol or drugs; 26 reported exceeding the speed limit by 10 km/hour or more; and 18 reported mobile phone use while driving. We could not determine if these youth were supervised by a fully licensed person (as per Victorian law).
Engaging in road risks was strongly associated with health risks including use of tobacco, alcohol and illicit drugs, and unprotected sex. This is a new finding among youth attending a healthcare setting and consistent with evidence supporting the problem behaviour theory.2,5,17 There is conflicting evidence for an association between depression and anxiety in high-risk drivers.2,16 This study showed no association between road risks and emotional distress. Road risks were more likely to occur in employed youth, which may be attributed to greater financial independence and increased access to motor vehicles. Young people born outside Australia were significantly less likely to report road risks. The reason for this is unclear and requires further investigation.
A major strength of this study is the methodological rigour in recruiting and interviewing youth using CATI interviewers blind to the allocation status of patients. It therefore minimises interview bias based on study arm.
The main limitations of this study are that it is a secondary analysis of data collected in a large RCT, so it was not possible to include other measures. The wording of the measure for mobile phone use (‘In a car, how often do you stop driving if you need to receive, or send, a call or text message on a hand held mobile phone?’) may have been confusing and therefore underestimated the true occurrence. Cross-sectional analysis of trial data was adjusted for study design factors including intervention arm, practice billing, SEIFA, recruitment method and clustered data. Self-reported measures are subject to recall error, social desirability and potential under-reporting of illegal behaviours or over-reporting of safety device use. However, self-report has been a well-validated method for road safety research in youths.8,9 Our proportions of youth with road risks attending general practice stop short of true prevalence because clinicians did not recruit every eligible young person during the study period; this was rectified when research assistants were introduced. Adjustment analyses did not change estimates; hence, the proportions are likely to be approaching true prevalence.
There were more females than males recruited to the study, which is likely to be attributed to the well-established observation that males attend health services less often than females, even after adjusting for reproductive health visits.19,30 Males had higher rates of some road risks; however, a significant gender association with road risks was not found in this study. Given that males represent 75% of young driver fatalities, further studies recruiting more males are needed.5 New graduated licensing laws came into effect in Victoria during the period of data collection (2007–10). As of 1 July 2008, the probationary period was increased from three to four years, and a limit of carrying only one peer passenger in the first year was introduced.11 Laws prohibiting mobile phone use and a limit of zero blood alcohol concentration remained unchanged during this period.11 These more stringent measures may have affected the rates of road risks; however, young people continue to be over-represented in crash statistics.5
The results of the RCT, now available,26 revealed that intervention clinicians discussed road safety significantly more often than comparison clinicians; however, this was only 10% of consultations. This level of intervention did not have an impact on road risks; study authors attributed this in part to lack of a robust instrument to measure road risks and the study’s lack of power to assess changes in each behaviour.26 However, other behaviours that may have an impact on road safety, such as use of illicit drugs and alcohol did show favourable shifts. Suggestions for approaching the topic of road safety within a consultation are presented in Box 1 (available online only). Current work explores the potential of technology for systematically and efficiently identifying risks in general practice.31
Implications for general practice
Global health agendas have prioritised youth injury prevention.1,4 Young people, still over-represented in crash statistics, despite graduated licensing restrictions, require additional approaches.6,13 Most youth attending Australian general practices are engaging in at least one road risk, often associated with other health risks that have a negative impact on future health. Hence, GPs with the capability of tailoring interventions to individuals could have a valuable role in further reducing the youth road toll. Future research is needed to refine ways to assess and address road risks in primary care, informed by clinicians and young people, to ensure potential for effectiveness.
Authors
Jennifer Martin MD, BBiomedSci, Hospital Medical Officer, Melbourne Medical School, University of Melbourne, Carlton, Vic
Sylvia Kauer PhD, BBehSci (Hons), Postdoctoral Research Fellow, Department of General Practice, University of Melbourne, Carlton, Vic
Lena Sanci MBBS, PhD, FRACGP, Associate Professor, Deputy Head, Department of General Practice, University of Melbourne, Carlton, Vic. l.sanci@unimelb.edu.au
Competing interests: None
Provenance and peer review: Not commissioned, externally peer reviewed.
Acknowledgements
We would like to acknowledge Patty Chondros for her statistical support and guidance on this project. We would also like to acknowledge Antonietta Cavallo from VicRoads for her input into the gaps in the field of clinical research on this topic. The data for this project were collected as part of a randomised controlled trial funded by the Australian Health Ministers’ Advisory Council (AHMC), the Australian Primary Health Care Research Institute (APHCRI) and the National Health and Medical Research Council (NHMRC). We wish to acknowledge and thank the young patients, clinicians and general practice staff who participated in the PARTY project, and all the researchers involved, particularly the other investigators: George Patton, Susan Sawyer, Jane Pirkis, Alan Shiel, Kelsey Hegarty, Elizabeth Patterson, Helen Cahill, and Elizabeth Ozer.
References
Box 1. Approaching the topic of road safety with young people in general practice
|
The HEADSSS framework24 commonly used in primary care settings to explore psychosocial risk and protective factors in a young person’s life can include an S for safety:
Home
Education, employment, eating, exercise
Activities and peers
Drugs, cigarettes, alcohol
Sex and sexuality
Suicide and other mental health screening
Safety (eg discussion on topic of road safety).
Signposting and permission:
‘We have had a discussion of lifestyle factors that may affect your health and safety. I would now like to ask you about your safety on the road – would that be okay with you?
Open-ended question:
‘Just wondering, what sort of things you do to keep yourself safe when driving a car/riding a bike/skateboard, etc?’
Targeted questions:
‘Thanks, I see you are aware of a number of safety strategies, that’s great … I have some other things on my list I would like to check out with you if that’s okay. What percentage of the time do you manage to wear a helmet/seatbelt when you are riding/driving? How often do you drive 10 km/hour or more over the speed limit? How often do you drive when you are feeling tired or sleepy? We talked about drinking/drugs before, what are your travel arrangements when you have been drinking/taking drugs? What do you do if you get a call/text when you are driving?’ These are just some examples, but it does depend on the individual patient. If any significant risk taking comes to light, advice or further discussion may be required, as with any lifestyle risk, using a non-judgemental approach.
Further resources on working with young people in primary care can be found at www.party.unimelb.edu.au/resources/otherresources.html
|