Case
A previously healthy, competitive surfer (male, aged 23 years) from the Gold Coast presented with chronic ear discomfort, having noticed frequent water trapping in the ear canal (Figure 1). He had been surfing for 11 years and denied participating in any other form of water activity.
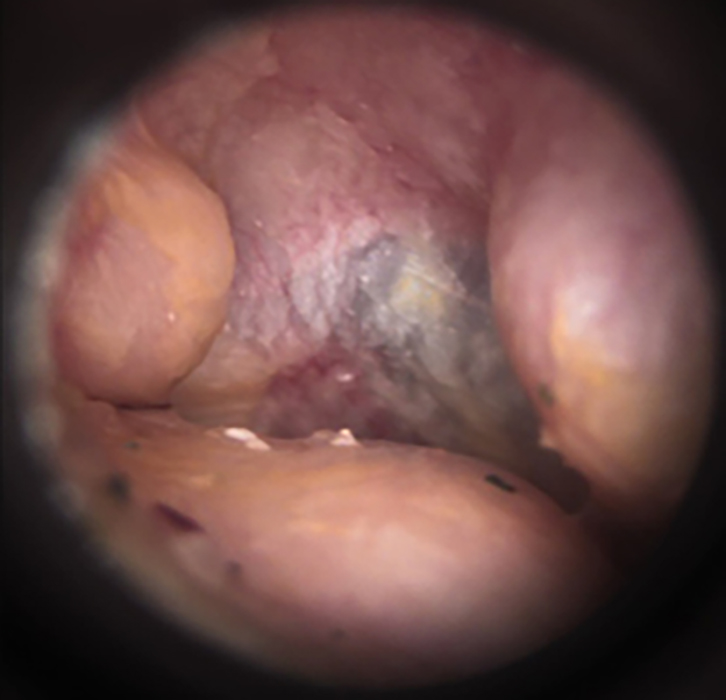
Figure 1. Otoscopic image identifying auditory exostoses in a young male competitive surfer
Question 1
What is surfer’s ear?
Question 2
What is the clinical presentation of surfer’s ear?
Question 3
What is the prevalence of surfer’s ear in surfers?
Question 4
What are the pathophysiology and aetiology of surfer’s ear?
Question 5
What are the risk factors of surfer’s ear?
Question 6
How is surfer’s ear diagnosed?
Question 7
What are the differential diagnoses of someone suspected of having surfer’s ear?
Question 8
Is surfer’s ear preventable?
Question 9
What is the treatment of surfer’s ear?
Question 10
When is it appropriate to refer a patient with surfer’s ear to a specialist?
Answer 1
Surfing is a popular recreational activity and competitive sport, with an estimated 37 million surfers worldwide.1 In Australia, this number is estimated at 2.7 million, which accounts for more than one in 10 Australians.2 One of the chronic conditions associated with surfing is external auditory exostosis (EAE). This condition is a benign and irreversible, broad-based bone outgrowth that arises from the temporal bone and projects into the external auditory canal (EAC). EAE is commonly referred to as surfer’s ear, although it has also been described in other aquatic sports. Australia is recognised as having a high prevalence of EAE.3–5
Answer 2
Typically found bilaterally with multiple lesions, EAE is usually asymptomatic and hence is often diagnosed when the condition is at an advanced stage,6 leading to a higher incidence of potentially serious health issues. Patients can present with a prolonged blocked feeling in the ears following water activities because of water trapping in the EAC or chronic cerumen impaction. Patients may also present with recurrent otitis externa, otalgia and conductive hearing impairment due to stenosis of the EAC.
EAE can be classified into four grades of severity based on the percentage of obstruction of the EAC, as assessed by otoscopy (Figure 2):7
- Grade 0 – normal ear canal, no visible exostosis
- Grade 1 – obstruction of up to 33%
- Grade 2 – obstruction of 34–66%
- Grade 3 – obstruction of 67–100%.
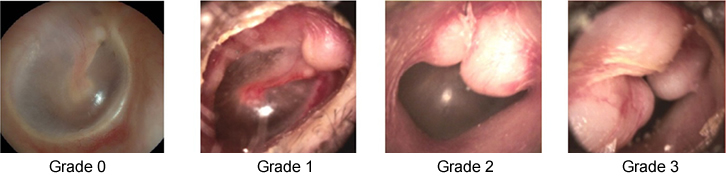
Figure 2. Otoscopic image identifying the four grades of EAE
Grades 1–3 reproduced from Nakanishi H, Tono T, Kawano H. Incidence of external auditory canal exostoses in competitive surfers in Japan. Otolaryngol Head Neck Surg 2011;145(1):80–85 with permission from SAGE Publications, Inc.
Answer 3
The prevalence of this condition in surfers, both professional and recreational, is 38–80% when investigated by otological examination.8,9 A study in Victoria reported that 78% of male surfers and 69% of female surfers had some degree of exostoses; a severe grade (ie Grade 3) was observed in more than 50% of the male surfers diagnosed.3 However, our recent study investigating injuries while surfing via an online survey identified only 3.5% of the participants reporting exostoses.10
Answer 4
The precise mechanism for the development of EAE remains unknown. Cold water and air exposure are believed to stimulate osteoblasts within the temporal bone, leading to bone growth into the EAC, possibly as a mechanism to protect the tympanic membrane against low temperatures.11,12
Answer 5
It is well known that EAE is highly correlated with the amount of time spent in the water. The risk of EAE increases after five sessions of surfing per month and significantly increases after five years of surfing.13,14 Exposure to cold water and wind are recognised risk factors.15,16 With regard to the wind effect, it has been proposed that evaporative cooling would result in greater progression of exostoses in the ear more exposed to a predominant wind. However, some studies did not find significant differences in prevalence and severity between the ears, even though one ear was typically more exposed to the wind than the other.12 Exostosis of the EAC does not appear to be influenced by genetic factors or any type of medication.12,17
Answer 6
Auditory exostosis is diagnosed via otoscopic examination to identify bony outgrowths projecting into the EAC.
Answer 7
Some of the differential diagnoses of EAE include osteoma, squamous cell/glandular cell carcinoma, benign glandular tumours, cholesteatoma and conditions affecting the temporal bone (eg paraganglioma).18
Answer 8
The feasibility of EAE prevention remains uninvestigated. However, given the current theory of aetiology, the regular use of earplugs or other protective equipment (eg hood) has been suggested in the literature to prevent the occurrence of EAE.14 Avoiding exposure to cold or windy conditions when surfing is also recommended.
Answer 9
The definitive treatment of EAE is surgical removal, which is usually only reserved for severe and symptomatic cases. This procedure does not prevent recurrence and exposes the individual to risk of complications, such as tympanic membrane rupture, sensorineural hearing loss, facial nerve injury, infection, delayed healing and stenosis.4,15
Answer 10
Referral to an otorhinolaryngologist is advised for large lesions (Grade 3), recurrent ear infections or progressive hearing loss. Referral is also recommended if the doctor or patient have any concerns, and when there is suspicion of another diagnosis (eg tumour) or when the symptoms are not compatible with clinical findings (eg hearing loss with only a small lesion). An audiogram should be organised prior to referral.18
Key points
- EAE is a common condition in surfers.
- EAE is typically undiagnosed at early stages.
- EAE is a potentially serious health issue.
- Risk factors of EAE include exposure to cold water and wind.
- The only treatment for EAE is surgical correction, which is reserved for severe or symptomatic cases.
- Prevention of EAE should be highlighted, and general practitioners play an important role in early identification and advising susceptible patients.
Authors
Vini Simas MD, PhD candidate, Water Based Research Unit, Institute of Health & Sport, Faculty of Health Sciences and Medicine, Bond University, Gold Coast, Qld. vinicius.perezsimas@student.bond.edu.au
James Furness PhD, Assistant Professor, Water Based Research Unit, Institute of Health & Sport, Faculty of Health Sciences and Medicine, Bond University, Gold Coast, Qld
Wayne Hing PhD, Head of Program, Professor Water Based Research Unit, Institute of Health & Sport, Faculty of Health Sciences and Medicine, Bond University, Gold Coast, Qld
Rodney Pope PhD, Associate Professor – Physiotherapy, Water Based Research Unit, Institute of Health & Sport, Faculty of Health Sciences and Medicine, Bond University, Gold Coast, Qld
Joe Walsh MSc, Exercise & Sport Science, Charles Darwin University, Casuarina, NT
Mike Climstein PhD, FACSM, FASMF, Adjunct Associate Professor, Exercise Health & Performance Faculty Research Group, Faculty of Health Sciences, University of Sydney, Lidcombe, NSW; Vale Medical Practice, Brookvale, NSW
Competing interests: None.
Provenance and peer review: Not commissioned, externally peer reviewed.