Effective communication between general practitioners (GPs) and their patients is essential to the provision of high-quality care and the best health outcomes for patients. Criterion 1.2.3 of The Royal Australian College of General Practitioners’ (RACGP’s) Standards for general practice, fourth edition, states that ‘our practice provides for the communication needs of patients who are not proficient in the primary language of our clinical team and/or who have a communication impairment’.1 To facilitate this, GPs in Australia have free access to Auslan for patients who are deaf, and professional interpreters for Medicare-rebateable consultations via the Translating and Interpreting Service (TIS).1 TIS operates the Doctors Priority Line, a telephone service available 24 hours a day, seven days a week, providing access to an interpreter within three minutes.2 Appropriate use of interpreters is associated with improved clinical care, access to care, outcomes and satisfaction with care.3,4 However, there is concern that professional interpreters are under-utilised in general practice.5–10
In 2011, one-fifth of Australians reported speaking a language other than English (LOTE) at home, and 16.7% of this population group (3% of all people) indicated that they had limited English proficiency.11 Bettering the Evaluation and Care of Health (BEACH) data suggest that more than one in 10 (11.3%) patients at GP consultations in 2011–12 reported that their primary language was not English. However, most GPs (73%) reported that they conducted all of their consultations in English.12 An analysis of census and TIS data suggest that just 1% of GP and specialist consultations with patients with limited English proficiency involved professional interpreters.6 A similar local study in New Zealand estimated that 0.7% of consultations in general practice with patients with limited English proficiency involved professional interpreters.10 Both studies suggest much lower levels of professional interpreter services use than predicted for the population, but are based on extrapolated estimates of service use. To date, no studies have examined communication in general practice consultations with patients who speak a LOTE.
Barriers to interpreter use include:5,8–10
- lack of awareness of, and experience with, professional interpreter services among GPs and practice staff
- lack of time for GPs to use an interpreter
- GPs’ preference for the use of family members or friends as interpreters
- beliefs about patients’ preferences for the use of family members or friends as interpreters.
While there is evidence to suggest that interpreters are under-utilised, we do not know the extent to which GP–patient consultations involve communicating in a LOTE. This study sought to determine:
- the number of GP consultations with patients who speak a LOTE
- the extent to which these involve communicating in a LOTE
- who communicated with the patients in a LOTE
- GPs’ use, awareness of and opinions about use of professional interpreters.
Method
This study was a sub-study of the BEACH program – a continuous, national, cross-sectional survey of Australian GP activity. The BEACH methods are described in detail elsewhere.13 In summary, each year, approximately 1000 randomly sampled GPs are recruited, each recording details for 100 consecutive patient consultations on structured paper forms.
Between December 2013 and March 2014, 250 GPs recorded (for a sub-sample of 30 of their 100 consultations) details about:
- whether the patient spoke a LOTE at home
- the languages spoken
- whether that day’s GP–patient consultation involved communicating in a LOTE (known as a LOTE consultation)
- who communicated with the patient during the LOTE consultation.
Where a professional interpreter was not used, GPs were asked whether they believed their use would have improved the quality of the consultation.
Our study had a cluster sample design – the GP being the primary sampling unit, and the patient at the consultation being the unit of analysis. We used procedures in SAS Version 9.4, accounting for the cluster study design to determine robust 95% confidence intervals (CIs) for the resulting estimates and percentages. Significance of differences was judged by non-overlapping CIs.
Results
The study was completed for 6074 patients at consultations with 206 GPs (82.4% completion rate). The GP participants were similar to all active practising GPs in Australia14 in terms of their sex distribution and practice location as classified by the Australian Standard Geographical Classification (ASGC). GPs in the sample were more likely to have graduated in Australia (72.6%) than all GPs (62.5%), and were older, with 50.7% aged 55 years or older, compared with 42.8%.14
Patients speaking a LOTE
There were 986 (16.2%; 95% CI: 13.2–19.3) patients who reported that a LOTE was spoken at home, and more than 80 different languages were spoken among them. The most common languages spoken were Greek (14.9% of patients speaking a LOTE), Italian (13.8%) and Cantonese (7.7%; Table 1).
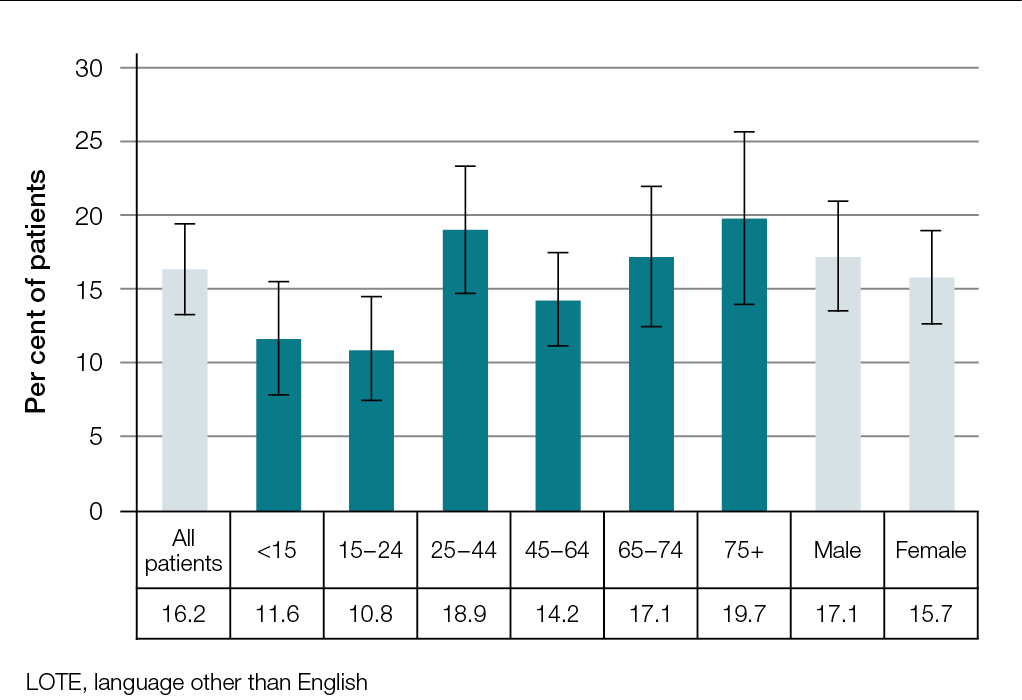
There were no statistically significant sex-specific or age-specific differences in the proportion of patients who spoke a LOTE (Figure 1). Three-quarters (74.8%) of GPs saw at least one patient in their sampled consultations who spoke a LOTE at home.
Table 1. Ten most common LOTE spoken by general practice patients at home
|
| Language | Number of patients | Per cent of all patients
(n = 6074) | Per cent of patients who spoke LOTE
(n = 986) |
|---|
| Greek |
147 |
2.4 |
14.9 |
| Italian |
136 |
2.2 |
13.8 |
| Cantonese |
76 |
1.3 |
7.7 |
| Spanish |
59 |
1.0 |
6.0 |
| Mandarin |
56 |
0.9 |
5.7 |
| Arabic |
49 |
0.8 |
5.0 |
| Hindi |
37 |
0.6 |
3.8 |
| Tamil |
29 |
0.5 |
2.9 |
| Croatian |
25 |
0.4 |
2.5 |
| German |
24 |
0.4 |
2.4 |
| Subtotal |
638 |
10.5 |
64.7 |
| Total |
994* |
16.2† |
100.0 |
*986 patients reported speaking 994 LOTE at home
† Patients reporting multiple languages were counted once
LOTE, language(s) other than English |
 |
 |
| Figure 1. Proportion of patients at general practice consultations who speak a LOTE at home – Total, age-specific and sex-specific rates (error bars are 95% CI; n = 986) |
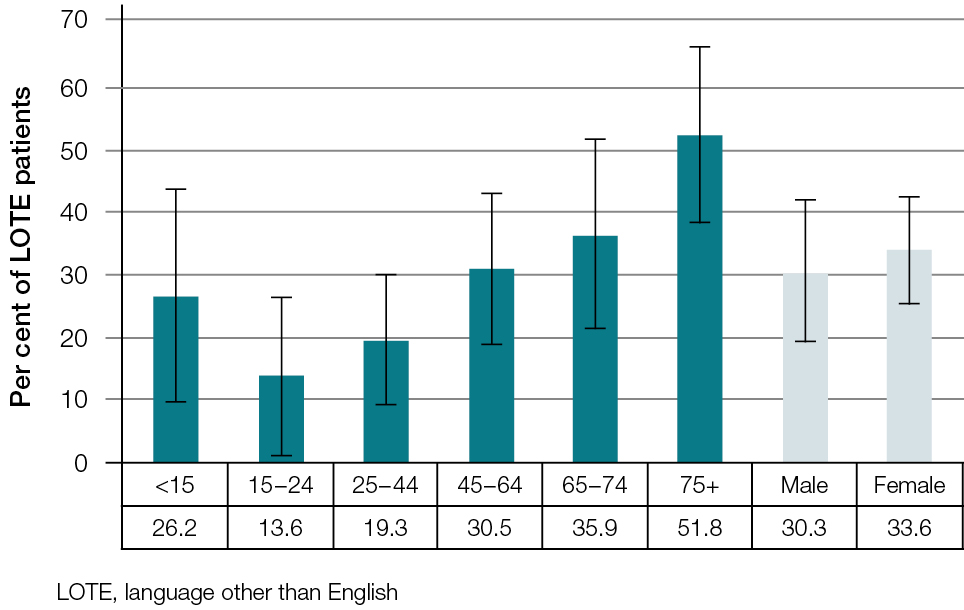
Figure 2. Age- and sex-specific rate of LOTE consultations among patients who speak a LOTE at home (error bars are 95% CI; n = 306) |
Consultations involving communicating in a LOTE
Information about languages spoken at the consultation was given at 946 (95.9%) of the 986 consultations where patients spoke a LOTE at home. Almost one-third (32.3%) of these consultations involved communicating in a LOTE (Table 2). One-third (31.1%) of GPs conducted at least one LOTE consultation.
Older patients who spoke a LOTE at home were more likely to have a LOTE consultation than younger patients, with 51.8% of consultations with LOTE patients aged 75 years or older involving communicating in a LOTE (Figure 2).
The person/people who communicated with the patient in the ‘other’ language was recorded for 305 patients. The majority (82.3%) of LOTE consultations involved GPs who spoke the patient’s preferred language (referred to as multilingual GPs). These multilingual GPs comprised 15.5% of all GPs in the sample (Table 2). Languages spoken at consultations with multilingual GPs were most commonly southern European (including Greek, Italian, 50.6%), Chinese (23.9%) and southern Asian (Indian subcontinent, 12.4%).
A family member or friend acted as an interpreter at 17.7% of LOTE consultations. One-fifth (20.9%) of GPs conducted at least one consultation involving a family member/friend interpreter. A professional interpreter was used at just 1.0% of consultations (Table 2).
Table 2. General practice consultations involving communication in a LOTE
|
| | Number of GPs* | Number of patients | Percentage of patients who spoke a LOTE (95% CI)† |
|---|
| Patient consultations involving communication in a LOTE |
64 |
306 |
32.3 (23.4–41.3) |
| Person who communicated with patients in a LOTE |
|
|
Percentage of patient consultations involving communication in a LOTE (95% CI) (n=305)‡ |
| GP |
32 |
251 |
82.3 (74.1–90.4) |
| Family member/friend |
43 |
54 |
17.7 (9.9–25.5) |
| Professional interpreter |
1 |
3 |
1.0 (0.0–3.0) |
| Other |
2 |
2 |
0.7 (0.0–1.6) |
Note: Missing data removed
CI, confidence interval; LOTE, language other than English
*The number of GPs in the sample of 206 who managed at least one patient in this category. Individual GPs can be included in more than one category because an individual GP can have patients in more than one category.
†There were 40 patients for whom data were missing.
‡Of the 306 patients at consultations involving communication in a LOTE, the question of who communicated at the consultations was answered by 305 patients, with 1 missing. Multiple responses were allowed. A total of 310 responses were recorded for 305 patients, therefore this column adds to more than 100%. |
Barriers to use of interpreters
Reasons for not using an interpreter were given for 220 (72.6%) of the 303 LOTE consultations. At 92.3% of consultations, GPs indicated that an interpreter was not needed (eg the GP was multilingual). For a further 15 consultations, the GP stated that an interpreter was not used because the patient was in a nursing home. At no consultations was lack of awareness or lack of availability of professional interpreter services reported.
GPs’ opinions about use of professional interpreters to improve quality
At 291 of the 303 LOTE consultations where a professional interpreter was not used, the GP gave their opinion as to whether their use would have improved the quality of the consultation. For 8.6% of these, GPs believed quality would have improved; they were unsure of improvement in 2.4% of consultations. For 89.0% of LOTE consultations they indicated that quality would not be improved or that the use of a professional interpreter would not have been appropriate.
GPs’ opinions of potential improvement varied depending on who communicated with the patient. At LOTE consultations with multilingual GPs, the GPs judged that the quality of 6.9% of consultations would have improved if a professional interpreter had been used, and they were unsure of improvement in a further 0.4% of consultations. Of consultations involving a family member/friend interpreter, GPs indicated the quality of the consultation would have improved for 14.8%; they were unsure of improvement for a further 13.0%.
Discussion
On average, 16% of patients at GP consultations spoke a LOTE at home. For two-thirds of consultations with these patients, English was spoken. The one-third involving communicating in a LOTE equated to 5.0% of all GP consultations. Extrapolating these results to the 137.3 million Medicare-rebateable GP consultations in 2014–15,15 using the method described by Britt et al,12 we estimate that throughout Australia there were approximately 22 million GP consultations with patients who spoke a LOTE at home, 7 million of which involved communicating with the patient in a LOTE.
The majority of LOTE consultations were provided by multilingual GPs, suggesting patients actively sought GPs who spoke their preferred language. Use of informal interpreters (family members/friends) was also common.
Our finding that professional interpreters were used at only 1% of LOTE consultations aligns with estimates from two previous studies based on census and interpreter services data in Australia6 and New Zealand.10
While other studies have reported a lack of awareness of professional interpreter services in general practice,5,9,10 this was not apparent among our sampled GPs. Although the use of professional interpreters was low, GPs felt their use could potentially improve the quality of some consultations, particularly when a family member/friend interpreter was used. GPs indicated the quality of 28% of these consultations would have or might have been improved. This suggests GPs may be receptive to systems that encourage the uptake of professional interpreter services to replace family member/friend interpreters. Practice-wide interventions are recommended as the best way to improve the use of professional interpreters in general practice.1,5,8
Seeing multilingual GPs seems to be a logical solution for patients to overcome language barriers. However, it raises concerns about a reliance on multilingual GPs for patients with limited English proficiency, as these GPs are unlikely to be able to cover the diversity of languages spoken in Australia. No quality concerns have been expressed in the literature about consultations undertaken by multilingual clinicians. However, it is interesting that for a small proportion (7%) of these consultations, GPs felt that the use of professional interpreters would have improved consultation quality. Where multilingual GPs are not available, our results suggest patients primarily rely on family members/friends to act as interpreters.
The use of family members/friends as interpreters is described as a common occurrence in general practice.1,8,9 We found they were used at 18% of LOTE consultations, and were the most widespread method of communication, with 21% of GPs in our study conducting at least one consultation where a family member or friend acted as the interpreter. There are well-documented risks with this approach including, for example, serious adverse health outcomes (including death), and medicolegal, privacy and ethical concerns.3,4,7,16 Caution is recommended for GPs using family members/friends as interpreters.1,7,17
Consultations with older LOTE patients were more likely to involve communicating in non-English languages than those with younger patients. This is likely to reflect poorer English proficiency reported among older Australians in the community.11 For a small group of older patients, being a nursing home patient was the reason GPs gave for not using an interpreter. This is a concern as it may indicate that the residential aged care facilities did not have policies to assist with communication. GPs should be aware of the increased need for communication support among their older LOTE patients.
This study is the first to investigate GP consultations involving communicating in a LOTE, using data collected from a national, random sample of GPs. Our study focused on consultations involving communicating in a LOTE, but it is possible that there were consultations conducted in English with patients who had limited English proficiency, for whom an interpreter may have improved the quality of the consultation. We also did not investigate the role that patient preference had in determining the use of interpreters. Investigating patients’ preferences, English proficiency, and their relationship to use of interpreters are areas for future research. It is also unclear whether the slight over-representation of GPs aged 55 years or more, and the under-representation of overseas graduates, had an impact on our results.
This study confirms that the use of professional interpreters at LOTE consultations is rare in Australian general practice. For the first time, we have shown that the majority of LOTE consultations are performed by multilingual GPs, for which no quality concerns are expressed in the literature. GPs recognised the potential to improve the quality of LOTE consultations that involved family member/friend interpreters through use of professional interpreters. Given published quality concerns related to use of family member/friend interpreters, this group should be targeted in future practice-based interventions that aim to increase the use of interpreter services.
Resources for GPs
Translating and Interpreting Service (TIS), Doctors Priority Line 1300 131 450
TIS is free for Medicare-rebated consultations. GPs need to register with TIS to access the service, https://tisonline.tisnational.gov.au/RegisterAgency
Authors
Clare Bayram BAppSc (HIM) (Hons), PhD, Research Fellow and Project Manager, BEACH program, Family Medicine Research Centre, Sydney School of Public Health, Sydney Medical School, University of Sydney, Parramatta, NSW.
clare.bayram@sydney.edu.au
Rowena Ryan MBBS, FRACGP, DipSocHealth, General Practitioner, Cohealth Kensington Community Health Centre, VIC
Christopher Harrison BPsych (Hons), MSocHlth, Senior Research Analyst, Family Medicine Research Centre, Sydney School of Public Health, Sydney Medical School, University of Sydney, Parramatta, NSW
Joanne Gardiner MBBS, DipObsRANCOG DipGeriatricMed(UK), General Practitioner, Cohealth Kensington Community Health Centre, VIC; Refugee Health Fellow, Royal Melbourne Hospital
Marion Jean Bailes MBBS, MHSc(Transcultural Mental Health), General Practitioner, Eastern Access Community Health, VIC
Nayantara Obeyesekere MBBS, DipChildPsych, General Practitioner, Cohealth Kensington Community Health Centre, VIC
Graeme Miller MBBS, PhD, FRACGP, Associate Professor, Medical Director, Family Medicine Research Centre, Sydney School of Public Health, Sydney Medical School, University of Sydney, Parramatta, NSW
Helena Britt BA, PhD, Professor of Primary Care Research, Director, Family Medicine Research Centre, Sydney School of Public Health, Sydney Medical School, University of Sydney, Parramatta, NSW
Competing interests: None.
Provenance and peer review: Commissioned, peer reviewed.
Acknowledgements
We wish to thank the general practitioners who participated for their generosity. During the data collection period of this study, the BEACH program was funded by the Australian Government Department of Health, AstraZeneca Pty Ltd (Australia), Novartis Pharmaceuticals Australia Pty Ltd, bioCSL (Australia) Pty Ltd, Merck Sharp & Dohme (Australia) Pty Ltd, and the Australian Government Department of Veterans’ Affairs. Funding organisations had no editorial control over any aspect of this article.