Case
A man, 31 years of age, presented to a rural Queensland medical practice with a four-month history of a progressive non-pruritic rash (Figure 1). On examination, multiple clustered papules were found distributed across the extensor surfaces of both knees and elbows. The papules were solid on palpation and painful when compressed. The patient had no significant past medical history and took no regular medications. He smoked about one pack of cigarettes per day.
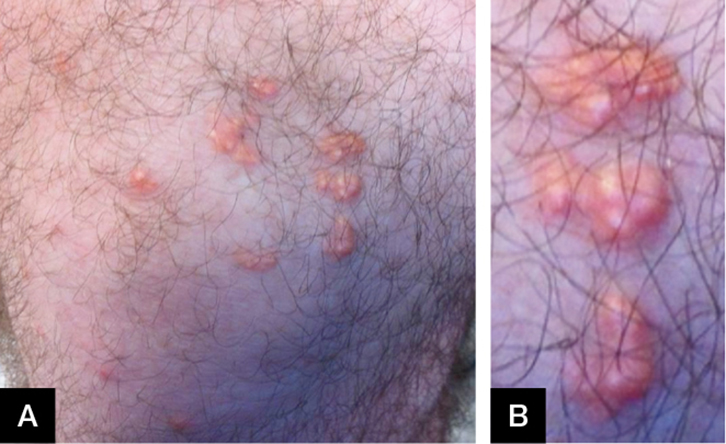 |
Figure 1. (A) Nodular eruption as at presentation
(B) Magnification of nodules |
The rural generalist performed a biopsy of the lesions and subsequently referred the case for a tele-dermatology consultation. Histology showed collections of histiocytes and focal, fibrillated, non-staining material in the superficial and mid-dermis (Figure 2). Occasional xanthoma cells and multinucleated giant cells were noted. These appearances were thought to be consistent with granuloma annulare.
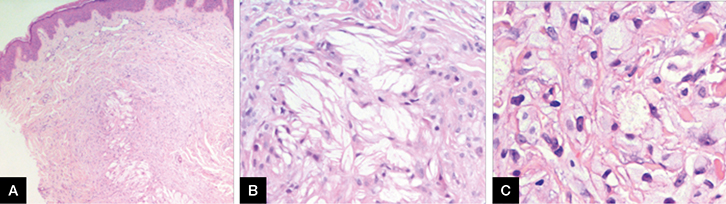 |
Figure 2. (A) Dermal histiocytic infiltrate with extracellular lipid
(B) High-power view of the extracellular lipid surrounded by foam cells and histiocytes
(C) Higher power view of foam cells |
After review by the tele-dermatologist, the case was reassessed as the clinical picture did not correlate with the initial histological diagnosis. Gouty tophus was considered as the fibrillary material was crystalline and birefringent, and resembled urate crystals, but the overall histological and clinical findings did not favour this diagnosis. However, eruptive xanthoma was in keeping with the appearances.
Subsequent lipid serology showed gross hypertriglyceridaemia and hypercholesterolaemia (triglycerides 47.0 mmol/L [RR <2.0 mmol/L]; total cholesterol 17.0 mmol/L [RR <4.0 mmol/L]). Serum urate and blood sugar levels were found to be normal. The patient was referred for a cardiology consultation. Further investigation, including a stress echocardiogram, was unremarkable.
Management included advice on strict lifestyle modification, including dietary optimisation and smoking cessation. The patient was started on gemfibrozil and fish oil, which saw a reduction in his triglycerides and resolution of the xanthomas within a few months.
Question 1
Under what circumstances do eruptive xanthomas typically form?
Question 2
How do eruptive xanthomas present clinically? Why was there initial uncertainty about the diagnosis after the biopsy?
Question 3
What are the ramifications of abnormally elevated triglyceride levels? What are the principles of management?
Question 4
What is ‘store-and-forward’ tele-dermatology? What are the benefits of this approach?
Answer 1
Eruptive xanthomas are uncommon, although important, stigmata of abnormally high serum lipid levels, namely when triglycerides exceed 20 mmol/L.1 It follows that aberrations in the metabolism of chylomicrons and very low-density lipoproteins (VLDL), the main transporters of triglycerides in serum, can result in the formation of these skin lesions. Our patient’s severe hypertriglyceridaemia and his convincing response to fibrate therapy indicates that the disorder is likely to be type V (Fredrickson classification system of hyperlipoproteinaemias).2 The prevalence of this condition is difficult to determine as many patients with high serum triglycerides remain asymptomatic; however, it is estimated to be 0.001–0.01% of the general population.2,3
Answer 2
Clinically, eruptive xanthomas present as papules with a red-to-yellowish hue, and are typically 1–5 mm1 in diameter. They generally form across the extensor surfaces of the arms and legs, as well as across the buttocks. The lesions can be tender or pruritic, particularly if severe.1,2
The first pathologist interpreted the biopsy as granuloma annulare because it showed interstitial collections of histiocytes and giant cells, as seen in this condition (though the extracellular lipid was unusual). With clinical correlation, the diagnosis was revised to eruptive xanthoma. Early eruptive xanthomas show histiocytes and a mixture of neutrophils and lymphocytes, but more established lesions show lipid and more foam cells, though not as many as in other forms of xanthomas.4,5
Answer 3
It is important that disorders of lipid metabolism are identified, as most are associated with the development of atherosclerosis and its sequelae. Specifically, hypertriglyceridaemia is associated with an increased risk of developing acute pancreatitis,6 hyperuricaemia, glucose intolerance, hepatosplenomegaly, hepatic steatosis and lipaemia retinalis.2
Aside from fibrate therapy, treatment also involves optimisation of factors such as weight, minimisation of alcohol intake, control of diabetes and a review of current medications.2
Answer 4
The case illustrates the ‘store-and-forward’ mode of telemedicine delivery, where information is captured by the primary doctor and sent for specialist consideration at a later time. This approach is convenient as the relevant information can be compiled at the patient’s first visit, and the generalist and specialist can then communicate at times suitable to themselves. There is no need for the clinical resource and coordination effort involved with the provision of live videoconferencing. As an adjunct, and depending on their layout, services such as these can provide an auditorium for ongoing, case-based education for generalists. The experience gained by directly managing these skin disorders, as well as the lessons learned from observing cases submitted by other practitioners, can be applied to other patients in the generalist’s practice.7,8
Key points
- Severe hyperlipidaemias can present cutaneously in the form of eruptive xanthomas, which manifest when triglyceride levels exceed approximately 20 mmol/L.
- Correct identification of eruptive xanthomas provides an opportunity to treat the underlying hyperlipidaemia and reduce the risk of premature cardiovascular morbidity.
- ‘Store-and-forward’ telemedicine is well suited to the provision of dermatological advice to general practitioners facing unusual clinical presentations. It can rapidly provide diagnostic and management advice and, in many cases, dispel the need for a face-to-face specialist consultation.
Authors
Stephen Andrews BE, MBBS, Resident Medical Officer, Mater Misericordiae Health Services, Brisbane, QLD. s.andrews@uq.edu.au
Lisa Byrom BPhty, MBBS, MPhil, Dermatology Registrar, Mater Misericordiae Health Services, Brisbane, QLD
Chamara Adikari MBBS, RVTS Trainee, Monto Family Practice, Monto, QLD
Inara Strungs MBBS, FRCPA, BA, Consultant Pathologist, Queensland Medical Laboratories – Histopathology, Brisbane, QLD
Jim Muir MBBS, FACD, FACRRM(Hon), Consultant Dermatologist, Mater Misericordiae Health Services, Dermatology Department, Brisbane, QLD
Competing interests: None.
Provenance and peer review: Not commissioned, externally peer reviewed.