General practice vocational training in many countries, including Australia, operates in an apprenticeship-based model. Most of the teaching and learning occurs in the practice environment with the trainee/registrar working as an independent practitioner, but under the overall supervision of an experienced general practitioner (GP) supervisor. Most learning is experiential and the learning environment is decentralised – compared with other specialties, learning occurs in relatively small, independent practices that are often widely dispersed geographically. The nature of learning and training occurring within the decentralised clinical component of training is not clearly visible and the potential for variability in clinical experience is considerable. The significance of this variability is that an adequate patient mix in medical training is deemed essential, being positively associated with learning outcomes.1
Establishing the epidemiology of trainees’ clinical experiences is vital in evaluating and planning educational programs. It is also of importance for individual registrars and their training practices: it may provide a framework for reflection on an individual registrar’s training experience and the training environment that supervisors and practices provide for their registrars. However, little has been documented about general practice training experiences, especially in Australia.
The Registrars’ Clinical Encounters in Training (ReCEnT) project has addressed these educational and research gaps. ReCEnT is conducted across five states in five of Australia’s 17 Regional Training Providers (RTPs) – General Practice Training Valley to Coast, the Victorian Metropolitan Alliance, General Practice Training Tasmania, Adelaide to Outback General Practice Training and Tropical Medicine Training. ReCEnT has been operating since 2009, and contains educational2 and research3 elements that are inextricably linked. Both elements are predicated on the collection of detailed and accurate data.
Data collection in ReCEnT
Each registrar in the participating RTP completes a round of data collection during each of their three, 6-month (full-time equivalent) general practice posts.
Registrars complete a questionnaire before each data collection round, providing demographic data on themselves and their current practice. Consultation data are recorded through a paper-based, patient encounter form. At approximately mid-term during each training term, the registrars record demographic, clinical and educational details of 60 consecutive, office-based consultations (home or nursing home visits are excluded). For a full-time, term 1 registrar, this represents patients seen in about 1 week. Data collected are related to registrar, patient, practice, consultation and educational aspects of the consultation. The variables collected are presented in Table 1.
Registrars receive a detailed face-to-face orientation to the project, and instructions on how to record the data. This is supplemented with a detailed manual.
Table 1. Variables collected
|
|
Registrar factors
|
|---|
- Age
- Gender
- Training term
- Training pathway enrolled in (rural or general)
- Place of medical qualification (Australia/international)
- Full-time/part-time status
|
|
Patient factors
|
|---|
- Age
- Gender
- Aboriginal or Torres Strait Islander status
- New patient to the practice
- New patient to the registrar
|
|
Practice factors
|
|---|
- Rurality/urbanicity*
- Practice size (number of general practitioners)
- Socioeconomic status of location†
- If the practice routinely bulk-bills patients
|
|
Consultation factors
|
|---|
- Duration of consultation
- Whether a practice nurse was involved in the consultation
- Number and nature of diagnoses/problems‡ dealt with
- If pathology was ordered
- If a specialist referral was made
|
|
Educational factors
|
|---|
- If the registrar sought clinical advice or assistance during the consultation (eg from their supervisor/trainer, from a specialist, allied health practitioner, or from electronic or hard-copy resources)
- If the registrar generated personal learning goals in the consultation
|
|
*Defined by the practice postcode and the Australian Standard Geographical Classification-Remoteness Area (ASGC-RA)13
†Defined by the practice postcode and the Socioeconomic Index for Area (SEIFA) Relative Index of Disadvantage14
‡Diagnoses/problems are coded according to the International Classification of Primary Care, second edition classification system (ICPC-2 plus)15
|
Educational uses of the data
The educational applications of ReCEnT are primarily based on facilitating registrars’ reflections on their practice through feedback on their clinical exposure and behaviours.2 Registrars receive an individualised, emailed feedback report after each round of data collection (6-monthly for full-time registrars) from the ReCEnT team.
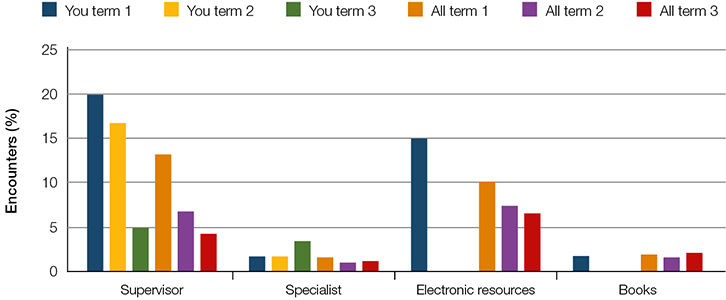 |
| Figure 1. An example of how a registrar’s information-seeking behaviours are presented in their report |
The report is comprehensive (11 pages, which includes 12 graphs/figures) and presents the individual registrar’s data for their current and previous rounds. Normative values derived from the aggregated data of the registrar’s peers (all registrars and all rounds of data collection) are provided to aid reflection. Comparable figures for established GPs in other studies are also provided for consideration. Timeliness is vital to the reflective process and we undertake to produce the report within 3 weeks of receiving completed encounter data. Examples of graphical feedback from the reports are presented in Figures 1 and 2 (for registrars’ information-seeking behaviour and exposure to the International Classification of Primary Care, second edition (ICPC-2 plus) classification system chapters, respectively). For ICPC-2 disease chapters and for the sex of patients, comparison is with aggregated data for registrars of the same sex. For all other parameters, the comparisons are of the individual registrar’s data with the aggregated data of all registrars (male and female). Thus far, we have produced and distributed 1920 reports for 880 registrars (from 10 rounds of data collection in 2009–2014).
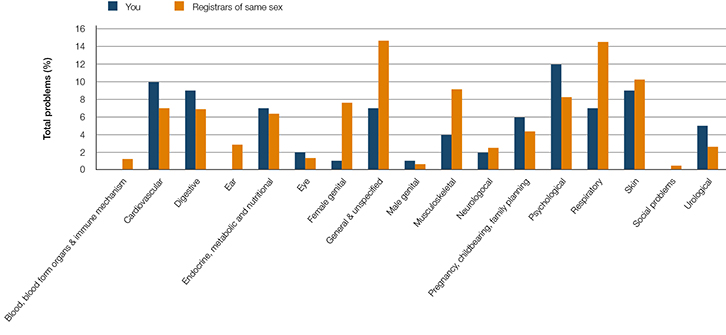 |
| Figure 2. Frequency of problems managed by disease chapter heading for current term |
Registrars are encouraged to reflect on their feedback data individually as well as in meetings with their supervisor and medical educator/training advisor. Reflection on clinical exposure and practice (eg patient demographic, chronic disease exposure, continuity of care) may identify potential deficits. Registrars may also reflect on aspects of the practice including prescribing, ordering tests, specialist referrals, and rates and sources of information-seeking. For example, the marked decrease in recourse to supervisor advice in Term 3, and the lack of in-consultation use of electronic or hardcopy resources during Terms 2 and 3, illustrated in Figure 1, would be expected to prompt the registrar and their supervisor to consider reasons for this. Given that they are working within an apprenticeship-like training model, reflection aided by the supervisor is particularly encouraged. Supervisors receive face-to-face instruction on how to use the report, supplemented by a ReCEnT Report User’s Guide. In addition to reflection prompted by the report, some registrars also report that the very act of data recording prompts reflection on their clinical practice.
A further level of reflection for supervisors and practices is provided by ‘practice feedback’ reports in which aggregated data of all registrars who have been supervised in an individual practice are presented, with comparisons of the aggregated data of all other practices. It is also anticipated that these recently introduced reports will be of use in registrars’ planning of subsequent term-placements (by comparing the relative deficits in their own clinical exposures with the aggregated exposures of registrars in prospective practice workplaces).
At the RTP macro-level, our data can be used to map coverage of the training curricula and inform articulation of RTP educational day-release activities with demonstrated relative deficits in clinical exposure. At the RTP micro-level, ReCEnT data are used to illustrate and contextualise materials in clinical lectures and workshops conducted by the RTP.
Research uses of the data
Although the principal function of ReCEnT is educational, it also has strong research and evaluation elements. Registrars may consent to the use of their data for research purposes.
Given the paucity of information on registrars’ clinical experiences,4 the initial research task of ReCEnT is to document the basic epidemiology of Australian general practice vocational training.5,6 Further analyses of registrars’ clinical exposures involving higher level general practice constructs, such as continuity of care,7 care of chronic disease,8 management of undifferentiated fatigue,9 pathology test ordering10 and the sources of in-consultation information and advice accessed by registrars, have been or are being conducted.
The cohort design of the project will allow longitudinal analyses, so enabling inferences of causality in registrars’ clinical experiences and behaviours. However, the greatest potential for this project is for interventional studies. The framework of ReCEnT data collection facilitates measurement of educational intervention outcomes. This represents a translational research–education model where ReCEnT data are used to identify evidence–practice gaps. Further ReCEnT data concerning the context of these evidence–practice gaps will then inform the construction of educational interventions. The effectiveness of the subsequent interventions can be measured by further rounds of ReCEnT data collection. Currently, trials on the effectiveness of educational interventions for evidence-based prescribing of opioids in chronic non-malignant pain, for rational test-ordering, and for evidence-based prescribing for respiratory tract infections are being conducted within the ReCEnT framework.
ReCEnT is a resource for registrar and supervisor research training. This includes academic registrars. Five academic terms have been undertaken, or are being undertaken, wholly or partly within the ReCEnT project. Areas of academic registrar research include testing for genital chlamydia,11 prescribing antibiotics for respiratory tract infections,12 recording of Aboriginal and Torres Strait Islander status in general practice clinical records, and the use and utility of dermatoscopy by registrars.
Conclusions
ReCEnT is a multifaceted project with strong research and evaluation elements. However, its principal functions are educational, particularly in prompting and facilitating reflection on practice and planning clinical training, and in registrar research training. Reflecting this, the ReCEnT project was the recipient of the 2014 General Practice Education and Training (GPET) Innovation Award.
Its successful operation is dependent on the ongoing contribution of the registrars and practices of the five participating RTPs. It requires collection of detailed and accurate data by registrars (a task that requires commitment and diligence), and prompt processing and return of these data to the registrars who have generated it, to allow them to make optimal use of it.
Authors
Parker Magin PhD, FRACGP, Conjoint Professor, Discipline of General Practice, the University of Newcastle, Newcastle; Medical Educator, General Practice Training Valley to Coast, Mayfield; NSW. parker.magin@newcastle.edu.au
Simon Morgan MPH&TM, FRACGP, Medical Educator, General Practice Training Valley to Coast, Mayfield, NSW
Kim Henderson BNurs, Grad Dip Health Soc Sci, Projects Manager, General Practice Training Valley to Coast, Mayfield, NSW
Amanda Tapley BBiomedSc, Research Officer, General Practice Training Valley to Coast, Mayfield, NSW
John Scott BComSc, Information Technology Officer, General Practice Training Valley to Coast, Mayfield, NSW
Neil Spike MBBS, FRACGP, Clinical Professor, Department of General Practice, the University of Melbourne, Carlton; Director of Medical Education and Training, Victorian Metropolitan Alliance, Hawthorn; VIC
Lawrie McArthur BMed, MBBS, FACRRM, FRACGP, Medical Director, Adelaide to Outback GP Training Program, Adelaide, SA
Jenny Presser BSc (Hons), PhD, MBBS, FRACGP, Senior Medical Educator, Tropical Medical Training, Townsville, QLD
Natalie Lockwood, Administrative Assistant, Education, General Practice Training Tasmania, Hobart, TAS
Mieke van Driel MD, Msc, PhD, Head of the Discipline of General Practice, The University of Queensland, Brisbane, QLD
Competing interests: None.
Provenance and peer review: Not commissioned, externally peer reviewed.