Basal cell carcinoma (BCC) is commonly seen in general practice. Most skin cancers are diagnosed and treated by general practitioners (GPs) in Australia, and their role in this area is increasing in volume and complexity.1
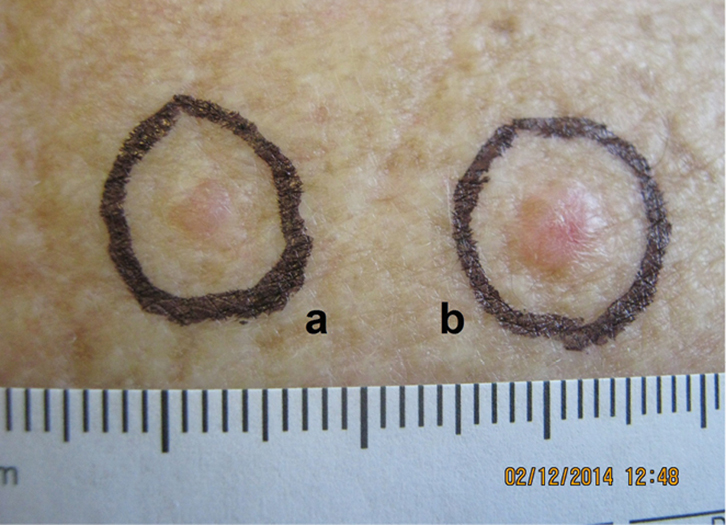 |
| Figure 1. Two BCCs on the patient’s back |
Case 1
Mrs BC, 73 years of age, presented for a general skin check. She was noted to have two skin lesions on her upper back (Figure 1). The larger lesion on the right (noted as ‘b’) is clinically typical of a BCC. There was an indurated ‘pearly’ nodule with surface telangiectasia, where the pearliness becomes more obvious with stretching of the skin. The smaller lesion on the left (noted as ‘a’) is less typical of a BCC to the naked eye.
Question 1
What management options are available, and what are the advantages and disadvantages of each?
Question 2
What are the typical features of BCC under the dermatoscope?
Question 3
How does the use of a dermatoscope for small BCCs differ from small melanocytic lesions and melanomas?
Answer 1
Management of a small lesion with non-specific clinical features consists of observation, biopsy and treatment.
Observation is the least invasive option. However, there is the risk of losing the patient to follow-up and eventual progression of the tumour, especially if the lesion is not readily visible to the patient.
Skin biopsy is a quick and accurate way to determine the diagnosis. However, the patient will require a second consultation for treatment if the biopsy confirms BCC.Lesions may be treated on spec, but this does expose the patient to the cost and morbidity of a potentially unnecessary procedure.
 |
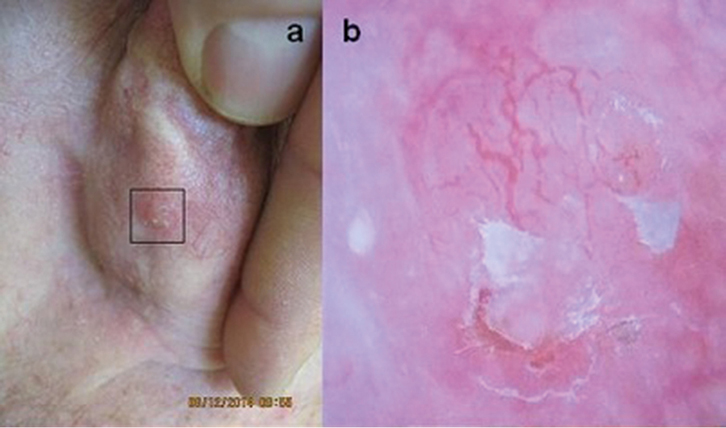
| Figure 2. Dermoscopy view of lesion b |
|
 |
| Figure 3. Dermoscopy view of lesion a |
|
In this case, the dermatoscopic images were very highly suggestive of BCC. The dermoscopy image of the bigger lesion (b) in Figure 2 shows arborising vessels and pink-white areas in the background. The dermatoscope image of the smaller lesion on the left (a) in Figure 3 is also diagnostic for BCC. Both lesions were treated at the initial consultation with cautery and curettage in this case. The histology of the curettings confirmed BCC (of nodular +/– superficial subtype).
Answer 2
There are several dermatoscopic findings that are used to diagnose BCC. These include arborising vessels (eg fine, well-demarcated, branching vessels), blue-grey ovoid nests, blue-grey dots and globules, ulceration and erosions, concentric structures, spoke-wheel areas, leaf-like areas, pink-white areas and short white streaks.2 These features are well described in many research articles, text books and websites. Good sources of images may be found at:
Dermoscopy of BCCs is best performed using a polarised light dermatoscope. Use of a glass contact face plate may reduce the vascular signs of a lesion due to the skin pressure it causes.
Answer 3
Dermoscopic features of a BCC (unlike melanocytic lesions) appear from the start of the natural history of the tumour. A 2012 study found 77% of BCCs 5 mm or less can be easily diagnosed with a polarised light dermatoscope.3
Case 2
A man, 78 years of age, presented with a small nodule on the posterior surface of his right pinna (Figure 4a). When seen with the naked eye, the lesion was likely to be a BCC. The adjacent dermatoscopic image (Figure 4b) shows well-defined arborising vessels, erosions and pink white structures.
 |
| Figure 4. Typical clinical and dermoscopy images of a BCC |
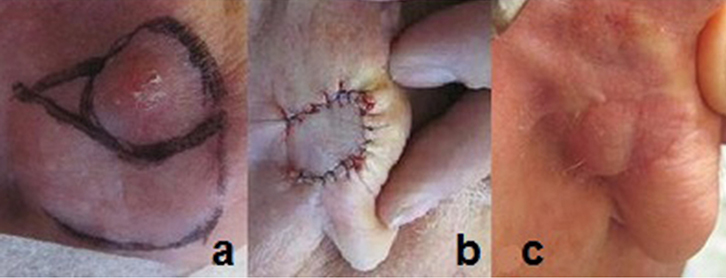 |
Figure 5. Excision of BCC from the posterior pinna
A. Pre-operative; B. Post-operative; C Five weeks post-operative |
Question 1
How accurate is the clinical diagnosis of BCC?
Question 2
Should the lesion be biopsied?
Question 3
What other applications does dermoscopy have for the management of BCC?
Answer 1
The diagnostic accuracy of dermatologists is thought to be 59–70% with BCCs.4 This can be increased to 95–99% with the use of a dermatosocope.2
Answer 2
Repairing a skin defect post-excision in this area may be difficult as it would require a skin flap or graft. The dermatoscopic image (Figure 4b) was diagnostic for a BCC and supported the clinical diagnosis. The lesion was therefore excised under local anaesthetic, and the defect was repaired with a small rotation flap at the initial consultation (Figure 5; (a) pre-operation, (b) immediately post-operation, (c) five weeks post-operation). Histopathology confirmed a completely excised BCC of nodular subtype.
Answer 3
The use of dermoscopy is quickly evolving, and broader applications are being applied clinically in the management of BCC:
- Dermoscopy has been found to assist with tumour margin assessment prior to excision. A 2012 trial of 112 patients found that the use of dermoscopy reduced sub-optimal excision rates from 22% to 7%.5
- Dermoscopy may help with assessing the response to non-surgical treatment (eg imiquimod), where dermoscopic features in the area after treatment correspond well with histological response to treatment.2
- Dermoscopy may assist in treatment choice. For example, pigmented BCC, which can appear non-pigmented to the naked eye, may respond poorly to photodynamic therapy. An alternative treatment may be more appropriate in these cases.2
Key points
Dermoscopy may assist in BCC management through:
- diagnosing small lesions
- increasing diagnostic accuracy
- assisting with the clinical diagnosis and reducing the need for skin biopsy
- assisting with BCC margin assessment
- assessing success following non-surgical BCC treatment
- assisting in the selection of non-surgical treatment modalities.
Author
Steven Tomas MBBS (Hons), MMed, FRACGP Clinical Lecturer, University of Sydney, and General Practitioner, Gumtree Medical Practice, Dubbo, NSW. stomas101@australiaonline.net.au
Competing interests: None
Provenance and peer review: Not commissioned, externally peer reviewed.