BEACH data collected in 2012–14 were used to investigate the management of unresolved gastrointestinal (GI) symptoms in Australian general practice. This included the characteristics of patients who had unresolved GI symptoms managed, and a comparison with the management of new GI symptoms. Nearly half of the GI symptoms managed in 2012–14 were unresolved (had been managed previously).
The findings suggest that general practitioners order pathology and imaging tests more often during first presentations of GI symptoms, and often refer patients when GI symptoms are unresolved.
In 2013–14, 19.1% of problems managed in Australian general practice were labelled as ‘symptoms and complaints’.1 Managing unresolved symptoms is a common challenge for general practitioners (GPs), and one study from the US indicated that only 56% of symptoms managed in primary care had completely resolved after 5 years.2
In this study, we investigated how GPs approach the management of unresolved symptoms, focusing on the management of ‘as yet unresolved’ gastrointestinal (GI) symptoms in general practice. The aims of this study were to:
identify the frequency at which unresolved GI symptoms were managed during general practice encounters, and the characteristics of patients who had unresolved GI symptoms managed
describe the management of unresolved GI symptoms, and compare this with the management of new cases of GI symptoms.
Methods
This was a secondary analysis of data from the Bettering the Evaluation and Care of Health (BEACH) program relating to Australian general practice activity. Detailed methods for BEACH are described elsewhere.3
For this study, we analysed BEACH encounters from April 2012 to March 2014 where a GI symptom was recorded as a problem managed. The problems managed were classified according to the International Classification of Primary Care, Version 2 (ICPC-2).4 We defined GI symptoms as:
- abdominal pain/cramps, general (ICPC-2 code D01)
- diarrhoea (ICPC-2 code D11)
- nausea (ICPC-2 code D09)
- abdominal pain, localised, other (ICPC-2 code D06)
- digestive symptom/complaint, other (ICPC-2 code D29).
GPs who participate in BEACH are asked to indicate whether a problem is being managed for the first time (ie a ‘new’ problem), or has been managed previously (an ‘old’ or as yet unresolved problem). All GI symptoms that were not marked as being new were regarded as unresolved. Problems expressed as diagnosed conditions (such as pancreatitis) that cause GI symptoms were not included in this study.
Results
Of 2453 GI symptoms managed between April 2012 and March 2014, 1153 (47.0%) were unresolved. These symptoms were managed at a rate of 0.60 per 100 encounters (95% CI, 0.56–0.63). When extrapolated, there was an estimated 780,000 GP encounters where unresolved GI symptoms were managed in Australia annually in 2012–14.
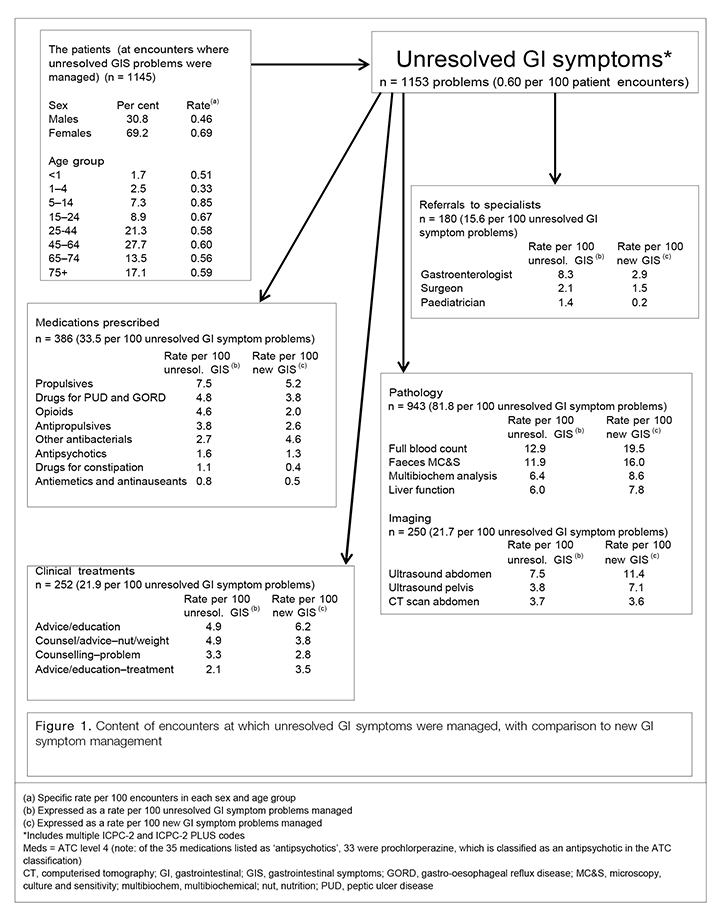
More than two-thirds (69.2%) of unresolved GI symptoms were managed in female patients (Figure 1). Significantly more females had undiagnosed GI symptoms managed (0.69%; 95% CI, 0.64–0.74) than males (0.46%; 95% CI, 0.41–0.51).
The age-specific rates at which unresolved GI symptoms were managed in general practice patients ranged from 0.33% (1–4 years) to 0.85% (5–14 years). The rate of unresolved GI symptom management was significantly lower in the 1–4 year age group (0.33%; 95% CI, 0.21–0.46) than for all older age groups (results not presented). There were no other differences present.
Figure 1 shows that 33.5 medications were prescribed per 100 unresolved GI symptoms managed. Propulsives (7.5 per 100 unresolved GI symptoms) and drugs for peptic ulcer and gastro-oesophageal reflux disease (GORD; 4.8 per 100) were most frequently prescribed.
For the average 100 unresolved GI symptoms, GPs made 15.6 referrals to specialists (95% CI, 13.4–17.8; Figure 1), which is more than twice the referral rate for new GI symptoms (6.2 per 100 problems, 95% CI, 4.8–7.6; results not tabled). About half of the referrals for unresolved GI symptoms were to gastroenterologists (8.3 per 100 unresolved GI symptoms).
Imaging tests were ordered at a rate of 21.7 per 100 unresolved GI symptoms managed. Ultrasounds of the abdomen (7.5 per 100) and pelvis (3.8 per 100) were the imaging tests most frequently ordered (Figure 1). Imaging orders were significantly less common in the management of unresolved GI symptoms (95% CI, 19.0–24.3) than for new GI symptom management (31.5 per 100 new GI symptoms; 95% CI, 28.2–34.7; results not tabled).
The rate of orders for pathology tests was also significantly lower for unresolved GI symptoms managed (81.8 per 100 unresolved GI symptoms; 95% CI, 72.7–90.9), compared with new GI symptoms (111.2 per 100 new GI symptoms; 95% CI, 101.4–121.1; results not tabled). Common pathology tests for unresolved GI symptoms were full blood count (12.9 per 100) and faeces microscopy, culture and sensitivity (MCS; 11.9 per 100).
Discussion
The findings of this study indicate that GPs order pathology and imaging tests more often during the first presentation of GI symptoms, compared with subsequent encounters. They often refer patients to gastroenterologists when GI symptoms are unresolved at subsequent encounters. GPs may refer because of investigation results, or when further investigations are required that GPs are currently unable to order (eg types of magnetic resonance imaging).
This paper provides information regarding how GPs approach the complexities involved in managing unresolved GI symptoms. However, very little quantitative research has been published regarding the extent to which unresolved symptoms evolve into ‘medically unexplained symptoms’. Addressing this deficiency in future research has the potential to help GPs manage this complex area of practice.
Authors
Julie Gordon BAppSc (HIM) (Hons), PhD, Research Fellow, Family Medicine Research Centre, Sydney School of Public Health, Sydney Medical School, University of Sydney, Parramatta, NSW. julie.gordon@sydney.edu.au
Graeme Miller MBBS, PhD, FRACGP, Medical Director, Family Medicine Research Centre, Sydney School of Public Health, Sydney Medical School, University of Sydney, Parramatta, NSW
Lisa Valenti BEc, MMedStat, Senior Research Analyst, Family Medicine Research Centre, Sydney School of Public Health, Sydney Medical School, University of Sydney, Parramatta, NSW
Competing interests: None.
Provenance and peer review: Commissioned, externally peer reviewed.
Acknowledgements
We wish to thank the general practitioners who participated for their generosity. During the data collection period of this study, the BEACH program was funded by the Australian Government Department of Health, AstraZeneca Pty Ltd (Australia), Novartis Pharmaceuticals Australia Pty Ltd, bioCSL (Australia) Pty Ltd, Merck Sharp & Dohme (Australia) Pty Ltd, Pfizer Australia Pty Ltd, National Prescribing Service Ltd, and the Australian Government Department of Veterans’ Affairs.