Patients with schizophrenia tend to present with physical complaints at a later, more serious stage. They also have a significantly higher incidence of type 2 diabetes mellitus, coronary heart disease and chronic obstructive pulmonary disease than the whole population.3 There is evidence of inequality not only in their healthcare access and utilisation, but also in healthcare provision, all of which contributes to their poor physical health.5,6
We sought to gauge the general health of patients (including the prevalence of lifestyle risk factors and comorbidity) having schizophrenia managed in Australian general practice.
Methods
This study was an analysis of data from the Bettering the Evaluation and Care of Health (BEACH) program and from two program sub-studies.7 BEACH methods are described in detail elsewhere.8 In this study, we identified patient encounters where schizophrenia was managed (ICPC-2 PLUS codes7 ‘P72002’, ‘P72004’, ‘P72005’, ‘P72011’) between April 2009 and March 2014. We also used data from a sub-study examining patient risk factors over the same period.8 The three-item Alcohol Use Disorders Identification Test-C (AUDIT-C) questionnaire9 was used to measure ‘hazardous’ alcohol consumption. Diagnosed comorbidities were identified from a chronic condition prevalence sub-study (conducted November 2012 – February 2015), in which GPs were asked to list all of the patient’s diagnosed chronic conditions (whether or not managed at that consultation).7
Results
Between April 2009 and March 2014, 4687 GPs recorded 468,700 encounters with patients. Schizophrenia was managed at 2086 of these encounters (at a rate of 4.3 per 1000 encounters). Male patients were twice as likely to have schizophrenia managed as female patients (Figure 1). Patients aged 25–64 years had a significantly higher rate of schizophrenia management than younger and older patients. Aboriginal and Torres Strait Islander patients also had a significantly higher management rate.
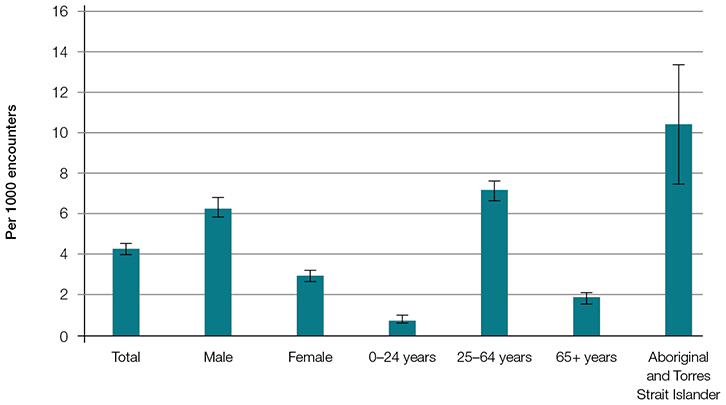 |
| Figure 1. Patient characteristic-specific management rate of schizophrenia per 1000 encounters |
Significantly more problems were managed at schizophrenia encounters (1.86 problems per encounter; 95% CI: 1.81–1.91) than at non-schizophrenia encounters (NSEs; 1.59 problems per encounter; 95% CI: 1.58–1.59). Almost half (49.0%; 95% CI: 47.4–50.7) of the other problems managed at schizophrenia encounters were chronic conditions, while only 34.8% (95% CI: 34.6–35.0) of problems managed at NSEs were chronic (results not tabled).
Lifestyle risk factors
Patients with schizophrenia were more likely to be obese and were more than three times as likely to be daily smokers as patients at NSEs (Table 1). However, patients with schizophrenia were less likely to drink alcohol at hazardous levels. Overall, patients with schizophrenia were nearly twice as likely as patients at NSEs to have two or more of these risk factors. To examine whether these findings were due to the age differences between the two groups, we repeated the process for patients aged 25–64 years and found the same pattern of differences as for all encounters (Table 1).
Table 1. Prevalence of risk factors, common comorbidities and multimorbidity
|
|
Topics
|
All encounters
|
Patients aged 25–64 years
|
|---|
|
|
Schizophrenia encounters % (95% CI)
|
Non-schizophrenia encounters % (95% CI)
|
Schizophrenia encounters % (95% CI)
|
Non-schizophrenia encounters % (95% CI)
|
|
Risk factors in adults
(18 years or older)
|
(n = 765)
|
(n = 152,203)
|
(n = 647)
|
(n = 88,929)
|
|
Daily smoker
|
51.0*
(47.5–54.5)
|
14.3
(14.0–14.6)
|
54.3*
(50.5–58.0)
|
18.7
(18.3–19.2)
|
|
Hazardous drinking
|
19.3*
(16.5–22.2)
|
24.8
(24.4–25.2)
|
20.1*
(16.9–23.3)
|
27.8
(27.4–28.3)
|
|
Obesity
|
40.0*
(36.4–43.6)
|
26.6
(26.3–27.0)
|
41.6*
(37.7–45.4)
|
28.4
(27.9–28.8)
|
|
Two or more risk factors
|
43.4*
(39.8–47.0)
|
22.5
(22.2–22.8)
|
46.4*
(42.4–50.3)
|
27.4
(26.9–27.8)
|
|
Comorbidities
|
(n = 158)
|
(n = 34,883)
|
(n = 121)
|
(n = 16,895)
|
|
Hypertension
|
13.3*
(7.7–18.8)
|
26.0
(25.1–26.9)
|
6.6*
(1.6–11.6)
|
16.4
(15.6–17.1)
|
|
Osteoarthritis
|
13.3*
(7.9–18.7)
|
22.9
(21.9–23.9)
|
6.6*
(2.1–11.1)
|
12.8
(12.1–13.6)
|
|
Hyperlipidaemia
|
10.1*
(5.5–14.8)
|
16.6
(15.8–17.3)
|
8.3
(3.4–13.1)
|
12.1
(11.4–12.8)
|
|
Depression
|
27.8 *
(20.0–35.7)
|
16.2
(15.6–16.8)
|
26.4
(17.5–35.4)
|
19.7
(18.9–20.6)
|
|
Anxiety
|
17.1
(10.7–23.5)
|
11.7
(11.1–12.3)
|
17.4
(9.9–24.8)
|
13.4
(12.6–14.1)
|
|
Type 2 diabetes
|
15.2
(9.8–20.6)
|
9.4
(9.0–9.9)
|
14.9*
(8.6–21.1)
|
6.5
(6.0–6.9)
|
|
Multimorbidity
|
|
Two or more chronic conditions†
|
74.7*
(67.6–81.8)
|
51.0
(49.7–52.3)
|
70.2*
(61.9–78.6)
|
44.2
(42.9–45.6)
|
|
Three or more chronic conditions†
|
53.2*
(45.0–61.3)
|
36.8
(35.6–38.1)
|
48.8*
(39.5–58.0)
|
27.0
(25.9–28.2)
|
|
*A significant difference in prevalence compared with patients at encounters where schizophrenia was not managed
†Not including schizophrenia as a chronic condition
|
Comorbid conditions
Of the 10 most prevalent chronic conditions, patients at schizophrenia encounters were more likely to have diagnosed depression than those at NSEs. They were significantly less likely to have diagnosed hypertension, osteoarthritis and hyperlipidaemia. There was no difference between the two groups in the prevalence of type 2 diabetes, anxiety, gastro-oesophageal reflux disease, chronic back pain and asthma. Overall, patients with schizophrenia were more likely to have diagnosed multimorbidity (both two or more and three or more chronic conditions, not including schizophrenia) than those at NSEs.
When we examined patients aged 25–64 years, patients with schizophrenia were significantly more likely to have diagnosed type 2 diabetes and less likely to have diagnosed hypertension and osteoarthritis. Overall, patients aged 25–64 years with schizophrenia were more likely to have multimorbidity (both two or more and three or more chronic conditions) than patients at NSEs.
Discussion
In line with international research, our study has shown that patients who have schizophrenia managed in general practice are more likely to have lifestyle risk factors and comorbidities than other patients. They are more likely to be daily smokers and more likely to be obese, but less likely to drink alcohol at hazardous levels. The higher number of problems managed at schizophrenia encounters and the higher proportion of chronic problems managed at schizophrenia encounters provide some evidence that GPs recognise and manage these comorbidities. However, the lower prevalence of diagnosed hypertension and osteoarthritis requires further investigation into possible underdiagnosis, as one would expect these patients to have high prevalence of both due to the high prevalence of obesity.10
As a large majority of patients with schizophrenia visit a GP at least once a year, GPs have the opportunity to screen for and manage chronic conditions at an earlier stage. For people with schizophrenia, management of the whole patient, not just their mental illness, is essential.
Authors
Christopher Harrison, BPsych (Hons), MSocHlth, Senior Research Analyst, Family Medicine Research Centre, University of Sydney, NSW. christopher.harrison@sydney.edu.au
Janice Charles BA, MSc (Med), Senior Researcher, Family Medicine Research Centre, School of Public Health, Faculty of Medicine, University of Sydney, NSW
Helena Britt BA, PhD, Director, Family Medicine Research Centre, Sydney School of Public Health, Sydney Medical School, University of Sydney, NSW
Competing interests: None
Provenance and peer review: Commissioned, externally peer reviewed.
Acknowledgements
We wish to thank the general practitioners who participated for their generosity. During the data collection period of this study, the BEACH program was funded by the Australian Government Department of Health, AstraZeneca Pty Ltd (Australia), Novartis Pharmaceuticals Australia Pty Ltd, bioCSL (Australia) Pty Ltd, Merck Sharp & Dohme (Australia) Pty Ltd, Pfizer Australia Pty Ltd, Sanofi-Aventis Australia Pty Ltd, GlaxoSmithKline Australia Pty Ltd, National Prescribing Service Ltd, Janssen-Cilag Pty Ltd, Abbott Australasia Pty Ltd, Roche Products Pty Ltd, Bayer Australia Ltd, Wyeth Australia Pty Ltd, and the Australian Government Department of Veterans’ Affairs. Funding organisations had no editorial control over any aspect of this article.
Competing interests: None.
Provenance and peer review: Commissioned, externally peer reviewed.