Case
A man aged 43 years presented for care after he felt an object strike his left eye while hammering a metal car part. He complained of foreign body sensation and photophobia. Examination with fluorescein staining showed a corneal abrasion. No foreign body was detected. The patient was discharged and placed on chloramphenicol topical treatment. He presented two more times over the next three days with ongoing irritation, photophobia and visual blurring in his left eye. Best-corrected visual acuity was 6/6 in the right eye and 6/5 in the left eye. The eye looked red and inflamed, but no foreign body was seen despite repeat examinations. On the third review, hypopyon was noted in the anterior chamber (Figure 1).
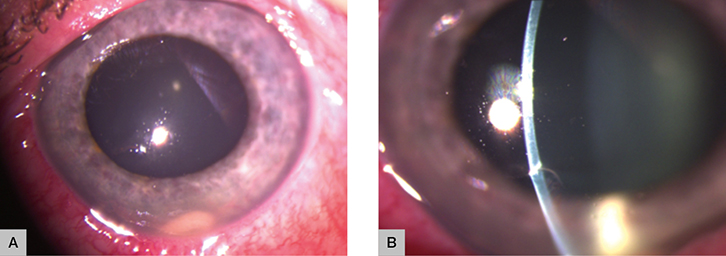 |
| Figure 1. Photograph of the affected eye on presentation |
Question 1
What is important to elicit on history in a patient with this presentation?
Question 2
How would you examine this patient?
Question 3
What would be the appropriate imaging in this case?
Question 4
What is the diagnosis?
Question 5
What initial management should you provide to this patient?
Question 6
What complications can occur from intraocular foreign bodies (IOFBs)?
Answer 1
As much information as possible should be obtained about the details of the injury, including the mechanism of injury, size and composition of the object, and its speed at the time of impact.1 Intraocular penetration can occur with seemingly minor trauma, particularly when foreign bodies result from high-speed machines, explosions or hammering (ie metal-on-metal injury).2 It is important to find out whether the patient was wearing safety glasses at the time of the injury. No eye protection is an important risk factor for penetrating eye injury (PEI).2
Answer 2
The initial examination should be as complete as possible, without further injuring the globe. Visual acuity (VA) should be measured in each eye separately using a standardised chart (eg Snellen chart). If the patient’s vision is too poor to be measured with standard charts, a gross assessment should be obtained (eg finger count at a specific distance, hand movement, light perception, no light perception).3 Next, pupillary response should be assessed, especially for the presence of relative afferent pupillary defect (RAPD). RAPD is observed using a bright light source, which is alternately directed at each eye in a swinging or back-and-forth fashion.3 The eye with the RAPD will paradoxically dilate when exposed to the light source.3 The presence of an RAPD may indicate optic nerve damage or significant retinal damage.3 Both VA and RAPD are the most important prognostic factors at presentation.4
A slit lamp examination is preferable, but not always available in the primary care setting. Assessment using a penlight or direct ophthalmoscope can still provide useful information. Conjunctiva should be examined for haemorrhage, chemosis (swelling) and laceration. The cornea should be examined for the presence of a foreign body, epithelial defect and laceration. To check for corneal wound leakage, stain the cornea with 2% fluorescein and carefully examine the cornea under cobalt blue light. If there is a full-thickness wound, the leakage of aqueous fluid will dilute the fluorescein dye, forming a green stream against the bright yellow background.3 This is known as the Seidel sign. The anterior chamber should be examined for its depth and presence of hypopyon (pus), hyphaema (blood) and IOFB. A peaked or ‘tear drop’ pupil is highly suggestive of PEI and can result from iris prolapse, which is protrusion of the iris through a corneal wound. The crystalline lens should be examined for dislocation and traumatic cataract. Red reflex should be assessed using a direct ophthalmoscope. Absence of red reflex may indicate a retinal detachment or dense vitreous haemorrhage. Assessment of intraocular pressure (IOP) should be deferred when there is suspicion of a PEI.
Answer 3
Suspected PEI or IOFB can be investigated using the following imaging modalities:4
- Computed tomography (CT) orbit – CT with thin slices is currently considered the gold standard for detection, localisation and characterisation of both metallic and non-metallic IOFBs.
- Plain X-ray – Although cheap and readily available, localisation of IOFBs without limbal ring may pose diagnostic problems.
- Ultrasound – Sensitivity is user dependent and contraindicated in cases of suspected globe rupture.
- Magnetic resonance imaging (MRI) orbit – MRI is contraindicated in the detection of suspected metallic IOFBs. It may be considered when there is a strong suspicion of non-metallic IOFBs that were not detected on CT or ultrasonography.
Answer 4
On slit lamp examination, there is a visible hypopyon in the anterior chamber (Figure 1A) and a full thickness corneal laceration (Figure 1B), both of which suggest possible PEI. In addition to the clinical findings, the orbital X-ray (Figure 2A) shows a metallic foreign body in the left orbit. The orbital CT (Figure 2B) localises the foreign body to the inferior section of the anterior chamber. These radiological findings confirm the diagnosis of the IOFB resulting from a PEI.
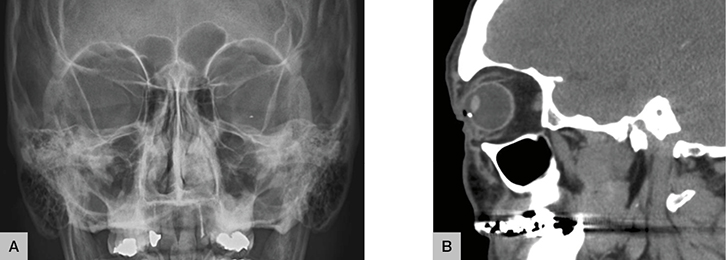 |
| Figure 2. Plain orbital X-ray (A) and CT orbit (B) |
Answer 5
The following initial management should be provided to all patients with PEI:5
- protect the eye with a rigid eye shield to prevent inadvertent pressure being applied to the eye
- make sure the patient is kept nil by mouth in case surgery is required
- adequate analgesia
- adequate antiemetic
- tetanus prophylaxis
- antibiotic prophylaxis, especially if there is going to be treatment delay due to travel.
All suspected or confirmed cases of PEI must be referred to an ophthalmologist immediately for further evaluation and management.
Answer 6
The most significant complication from IOFBs is endophthalmitis, which can have devastating visual consequences and may ensue with loss of the eye. Other potential complications include:4
- sympathetic ophthalmia
- retinal tear and detachment
- intraocular haemorrhage – hyphaema, vitreous haemorrhage
- elevated IOP
- traumatic cataract
- corneal scarring or opacity.
Case continued
The patient was transferred to a large tertiary hospital. He had sustained a 2 mm full-thickness corneal laceration at 7 o’clock, which had self-sealed as the Seidel sign was negative. No IOFB was visible on examination; however, in theatre, a metal foreign body was found buried deep in the iridocorneal angle at the location of the hypopyon. At his one-month follow-up, the patient’s VA was 6/7.5 in the left eye.
Key points
- Clinical signs of PEI can be subtle; hence, diagnosis can be delayed or missed.
- It is important to maintain a high index of suspicion, especially in patients at risk, as PEI can have devastating visual consequences.
- Hypopyon is a sign of severe intraocular infection and mandates an urgent specialist referral.
- All suspected or confirmed cases of PEI should be referred to an ophthalmologist immediately.
Author
Jenny Xue Tian BPharm, MBBS, Ophthalmology Principal House Officer, Princess Alexandra Hospital, Woolloongabba, QLD. jenny.tian@uqconnect.edu.au
Competing interests: None.
Provenance and peer review: Not commissioned, externally peer reviewed.