Plantar fasciitis (PF) is reported to be the most common cause of chronic inferior heel pain.1 Risk factors include obesity, occupations with prolonged standing, pes planus, limited ankle dorsiflexion, plantar heel spurs and running.1 Based on an Australian local population study of 3206 participants, the prevalence of heel pain was 3.6%.2
Australian general practice data from the national BEACH program between April 2000 and March 2014 inclusive (1,372,100 GP–patient encounters) were analysed to determine the patient characteristics and management choices at those encounters where PF was recorded, and detect changes in the annual management rate of PF.
Over this period, PF was recorded as a problem managed at 2622 encounters (0.19%, 95% CI: 0.18–0.20, of all encounters). The sex-specific rate of PF management at encounters was significantly higher among females (0.21%,0.20–0.22), than males, (0.16%, 0.15–0.17). The age-specific rate of PF management was highest (0.35%, 0.33–0.37) for the 45–64 year age-group, followed by the 65–74 year age-group (0.22%, 0.20–0.24); those under 25 years had the lowest frequency (Figure 1).
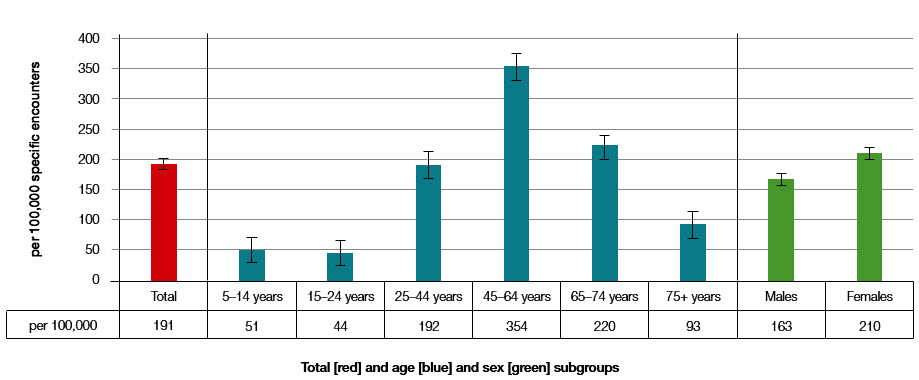 |
| Figure 1. Frequency of plantar fasciitis problem managed per 100,000 encounters in each age or sex subgroup and total (95% CI); April 2000 to March 2014: 2622 out of 1,372,100 encounters record plantar fasciitis) |
On average, for every 100 PF problems managed at encounter, 45.3 (95% CI: 42.7–47.8) medications were recorded (28.7 prescribed, 9.6 GP-supplied and 7.0 advised for over-the-counter purchase). Of these medications, approximately 64% were non-steroidal anti-inflammatory drugs, 17% were systemic corticosteroids, 6% were other analgesics and 6% were opioids.
On average, for every 100 PF problems, management actions were: 37.3 (95% CI: 35.1–39.5) clinical treatments (mostly advice/education and counselling); 27.0 (25.0–29.1) procedural treatments (including 14 physical medicine/rehabilitation and 7 local injections); 3.1 (2.5–3.8) medical specialist referrals (including 2 to orthopaedic surgeons); and 16.1 (14.5–17.6) allied health referrals (including 12 to podiatrists and 3 to physiotherapists).
For the period 2000–2014, the annual management rate of PF was variable, but trend analysis demonstrated a slight increase (3 per 100,000 per year, P = 0.006) (Figure 2). The clinical significance of this is uncertain; however, this increase may reflect the changing age or risk factor profile of the patient population.
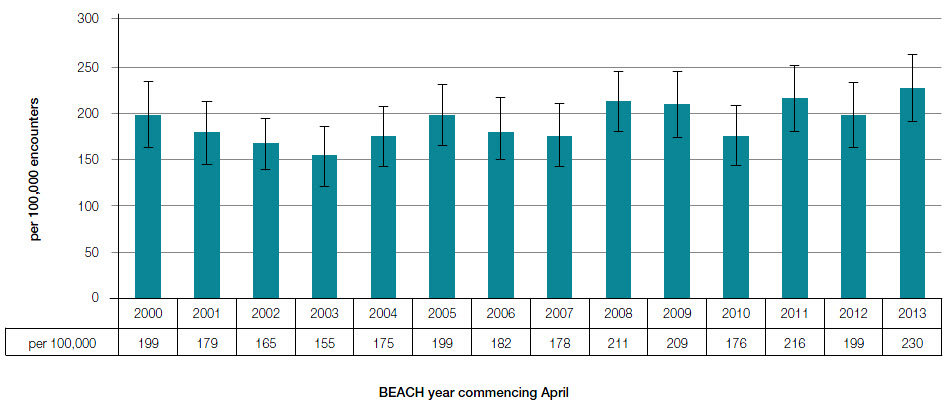 |
| Figure 2. Annual frequency of plantar fasciitis problem managed per 100,000 encounters (95% CI); (2622 out of 1,372,100 encounters record plantar fasciitis, April 2000 to March 2014) |
Although PF is not commonly managed in Australian general practice, we estimate that 310,000 (95% CI: 260,000–360,000) encounters involved PF management nationally in BEACH year 2013–14.
Competing interests: None.
Provenance and peer review: Commissioned, not externally peer reviewed.
Acknowledgements
The authors thank the GP participants in the BEACH program, and all members of the BEACH team.
Funding contributors to BEACH from April 2000 to March 2014: Australian Government Department of Health and Ageing and Department of Veterans’ Affairs; Abbott Australasia Pty Ltd; AstraZeneca Pty Ltd (Australia); Bayer Australia Ltd; bioCSL Pty Ltd; GlaxoSmithKline Australia Pty Ltd; Janssen-Cilag Pty Ltd; Merck, Sharp and Dohme (Australia) Pty Ltd; National Prescribing Service Ltd; Novartis Pharmaceuticals Australia Pty Ltd; Pfizer Australia Pty Ltd; Roche Products Pty Ltd; Sanofi-Aventis Australia Pty Ltd; and Wyeth Australia Pty Ltd.
BEACH is approved by the Human Research Ethics Committee of the University of Sydney.