Case
A woman, aged 21 years, presented to her general practitioner with a 1-month history of severe headaches. On further questioning she reported intermittent episodes of blurred vision. She was overweight and had a body mass index (BMI) of 32 kg/m2.
Snellan visual acuity was reduced to 6/18 in the right eye and 6/12 in the left eye. A dilated fundus examination using a direct ophthalmoscope demonstrated bilateral disc swelling, disc hemorrhages and loss of spontaneous venous pulsations in both eyes (Figures 1 and 2). Her eye movements were also abnormal (Figure 3).
|
|
|
Figure 1. Papilledema
Bilateral blurred disc margins in the right optic nerve; haemorrhages and cotton wool patches seen nasally |
Figure 2. Papilledema
Bilateral blurred disc margins in the left optic nerves; haemorrhages and cotton wool patches seen nasally |
 |
Figure 3. Abnormal ocular motility – false localising sign
A. Right gaze – normal abduction of right eye;
B. Primary gaze;
C. Left gaze – loss of abduction
of left eye past midline |
Question 1
What is the differential diagnosis for papilledema in a patient of this age group?
Question 2
What immediate investigations are appropriate?
Question 3
Who should be involved from this stage in this patient’s management?
Answer 1
The disc swelling in papilledema is the result of axoplasmic flow stasis in the area of the optic disc. If there is an increase in cerebrospinal fluid (CSF) pressure due to any cause, the pressure is transmitted to the optic nerve, the surrounding optic nerve sheath acts as a tourniquet and as a result stasis of flow occurs.1 This causes the appearance of hemorrhages and vessel anomalies at the disc.
The differential diagnoses for papilledema in a patient of this age include:
- malignant hypertension
- space-occupying lesion (benign or malignant)
- atypical meningitis
- idiopathic intracranial hypertension (IIH)
- dural venous sinus thrombosis
- atypical optic neuritis
- systemic vasculitides (eg systemic lupus erythmatosus, polyarteritis nodosa).2
Answer 2
The symptom most commonly reported was headache. Other symptoms include visual changes (blurred vision, transient visual obscurations, double vision).
The abnormal ocular motility – false localising sign in this patient – is as a result of elevated intracranial pressure. This causes mechanical compression of the abducens nerve (CN6) as it enters the midbrain, resulting in an abduction deficit on that side. Therefore immediate investigations include:
- urgent measurement of blood pressure
- computed tomography (CT) scan or magnetic resonance imaging (MRI) to exclude a space-occuyping lesion
- a CT venogram or MR venogram (MRV) to exclude dural venous sinus thrombosis.
Answer 3
This patient is likely to need input from a multidisciplinary team initially in a hospital setting.3 An initial referral should be made to:
- a neurology team for full neurological assessment and to facilitate the investigations listed above in a timely manner
- an ophthalmology team for review of vision and optic nerve function, including formal visual fields, even if vision is normal at presentation as this may change later in the course of this condition
- allied heath team including a dietician, physiotherapist and counsellor, as these team members will play an important role in co-managing this patient in the long term.
Case continued
The patient was referred immediately to a tertiary centre for urgent neurology review. A CT and later MRI/MRV were performed and both found to be normal. A lumbar puncture was then performed and opening CSF pressure was measured at 32 cmH2O (normal range 21–25 cmH2O). The CSF was clear of any infection.
Question 4
What is the definitive diagnosis now?
Question 5
What are the risk factors in this patient’s case pre-disposing her to this condition?
Question 6
What is the evidence-based management of this condition?
Answer 4
The definitive diagnosis is idiopathic intracranial hypertension (IIH), also known by the older terms benign intracranial hypertension (BIH) or pseudotumor cerebri (PTC).4 The modified criteria for a diagnosis of IIH includes:
- a normal CT/venogram or MRI/venogram
- an opening CSF pressure (in the lateral decubitus position) of >25 cmH2O
- symptoms and signs of increased intracranial pressure.
Answer 5
More than 90% of patients with IIH are women of childbearing age.5 Most cases of IIH occur in young women who have a higher BMI or recent weight gain. Other exacerbating factors may include:
- exposure to or withdrawal from certain drugs6 (eg tetracylines, corticosteroids, lithium, isotretinoin, trimethoprim, cimetidine, all-trans, retinoic acid used in treatment of some leukemias)
- vitamin A derivatives
- oral contraceptive pill.
Answer 6
Management of IIH is essentially medical but may involve surgical intervention in the medium-to-long term. The goals of management are to:
- reduce elevation of CSF pressure
- relieve patient of persistent headaches
- prevent visual loss
- prevent recurrences.
This patient was commenced on acetazolamide 250 mg 6 hourly daily. Acetazolamide is a carbonic anhydraise inhibitor useful in reducing CSF production.
Various trials have shown improvements in symptoms and visual function with maximally tolerated doses of acetazolamide (maximum 4 g/day). The recent multicentre NORDIC trial reported modest improvements in visual function with acetozolamide and weight reduction, compared with weight reduction alone for management of IIH.7,8
This patient was closely monitored over the ensuing weeks. Her vision improved with medical management. However, her headaches did not improve. She was subsequently referred to a neurosurgical team for an intracranial shunting procedure to redirect CSF. A review of published studies comparing various shunting procedures shows improvement in headaches and visual function in 38–44% cases9,10 (Figure 4).
This patient proceeded to do very well. Her visual acuity improved to 6/9 in each eye, although the visual field still showed some persistent defects. Her headaches have now completely resolved. She is currently on a diet and exercise weight-reduction program and receives 3-monthly reviews.
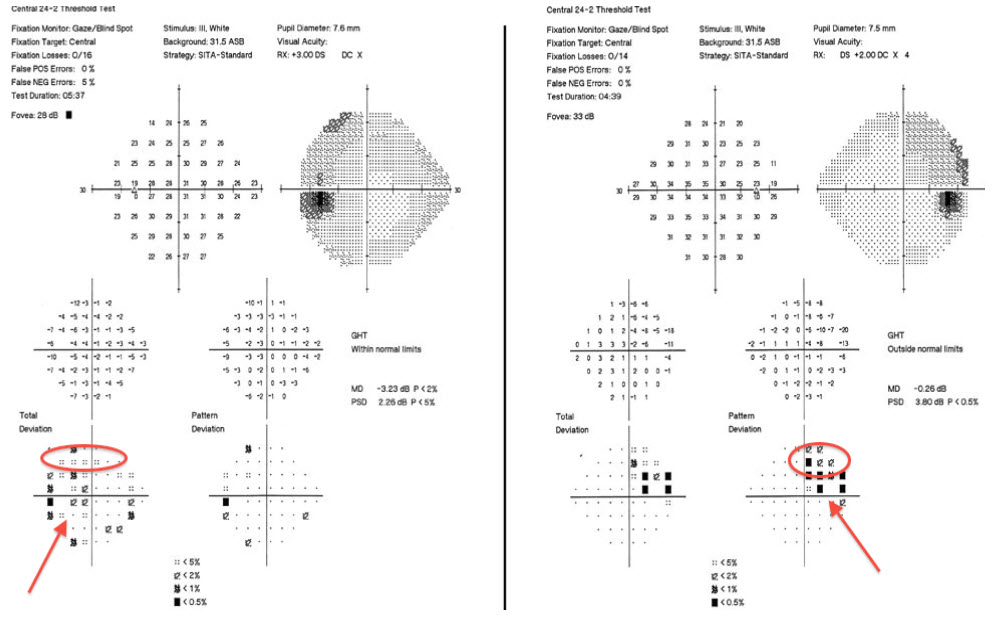 |
| Figure 4. Visual fields of this patient showing bilateral enlarged blind spots (arrows) and superior visual field defect (circle) |
Key points
- IIH is a common cause of papilledema in women of childbearing age who are overweight.
- A headache is often the initial presenting complaint in IIH.
- A thorough history and examination of intracranial pressure, visual acuity and funduscopy are essential for the assessment for IIH.
- A diagnosis of IIH can be made only after MRI and lumbar puncture with measurement of opening CSF pressure of >25 cmH2O.
- Current medical treatment includes oral acetozolamide, weight reduction programs and cessation of exacerbating medications.
- Surgical intervention, including intracranial shunting procedures and/or optic nerve sheath fenestration, may also be required (Figure 5).
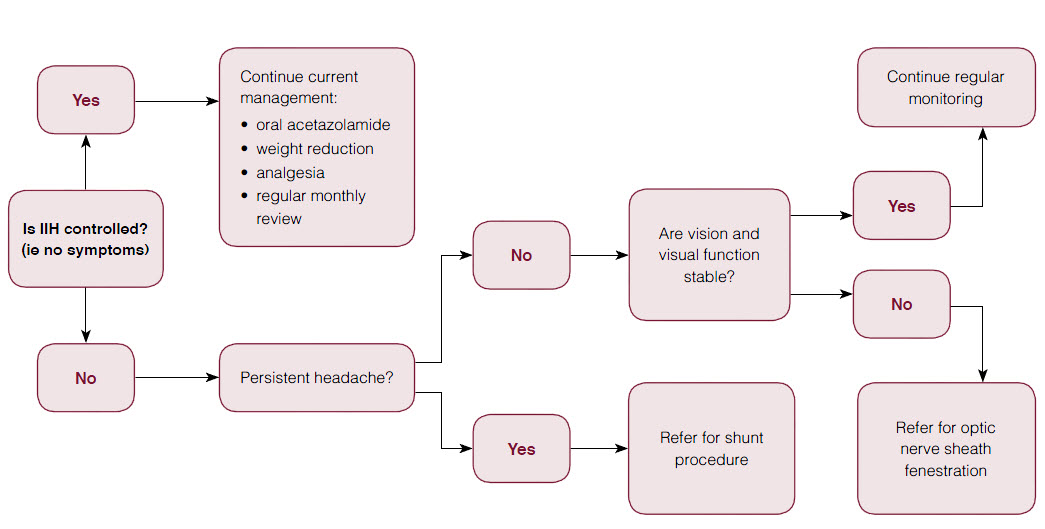 |
| Figure 5. Flowchart summarising current management guidelines of idiopathic intracranial hypertension (IIH) |
Competing interests: None.
Provenance and peer review: Not commissioned, externally peer reviewed.