Case
A Malay man, aged 23 years, presented to his local general practitioner (GP) with a 1-week history of fever, sore throat and mild bilateral shoulder, elbow and knee pain without joint effusion. He did not have any other respiratory, gastrointestinal or cardiovascular symptoms. He had a past history of Dengue fever and was currently employed as a worker in a spectacle frame factory. He had a 3 pack-year smoking history. He did not use illicit drugs or consume alcohol.
He was haemodynamically stable and afebrile. His examination was unremarkable, apart from an injected pharynx and bilateral finger and toe clubbing. There was no sign of joint inflammation and he had a normal range of motion for all his joints. The patient had not noticed the digital clubbing. On further questioning, he had no risk factors for human immunodeficiency virus (HIV), hepatitis B or C viruses.
A full blood count was done and the results were normal.
The patient came back for a follow-up 2 days later. All of his symptoms had resolved. After talking to his family, he realised that he was the only person in the family with digital clubbing.
How is digital clubbing detected?
Digital clubbing can be detected through various tests. Of these tests, Myers et al1 recommend assessment of profile angle and phalangeal depth ratio (Figure 1). A profile angle that approaches a straight line (180°) or phalangeal depth ratio that exceeds 1.0 is rare in people with no disease.1
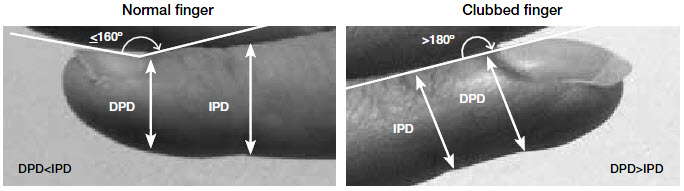 |
Figure 1. Profile angle and phalangeal depth ratio
DPD, distal phalangeal depth; IPD, interphalangeal depth |
What is the clinical significance of digital clubbing?
Digital clubbing can be an isolated finding or may occur as part of the hypertrophic osteoarthropathy (HOA) syndrome. The cardinal clinical features of HOA are periostosis (abnormal deposition of periosteal bone) of long bones, and joint pain and clubbing.2 HOA can be further classified into primary (also known as pachydermoperiostosis, an autosomal dominant disorder) and secondary (resulting from other disease processes). Familial clubbing is likely to be an incomplete form of primary HOA.3 Primary HOA represents approximately 5% of HOA cases, while the other 95% of cases are related to secondary causes.4 Of adults with secondary HOA, 90% have or will develop a malignancy.5 Therefore, clinicians should have high index of suspicion for any patient presenting with secondary HOA.
A Belgian study found that 40% of digital clubbing cases were associated with serious diseases, such as infection, malignancy or inflammatory conditions.6 Digital clubbing has been associated with bronchogenic carcinoma, lymphoma, mesothelioma, asbestosis, sarcoidosis, tuberculosis, cyanotic heart disease, primary biliary cirrhosis, cirrhosis, inflammatory bowel disease, HIV and other infections.3 The major conditions associated with secondary digital clubbing with or without HOA are pulmonary diseases (75–80%), cardiovascular abnormalities (10–15%), diseases of the liver and gastrointestinal tract (5–15%) and miscellaneous disorders (5–15%).7
How to manage patients with digital clubbing?
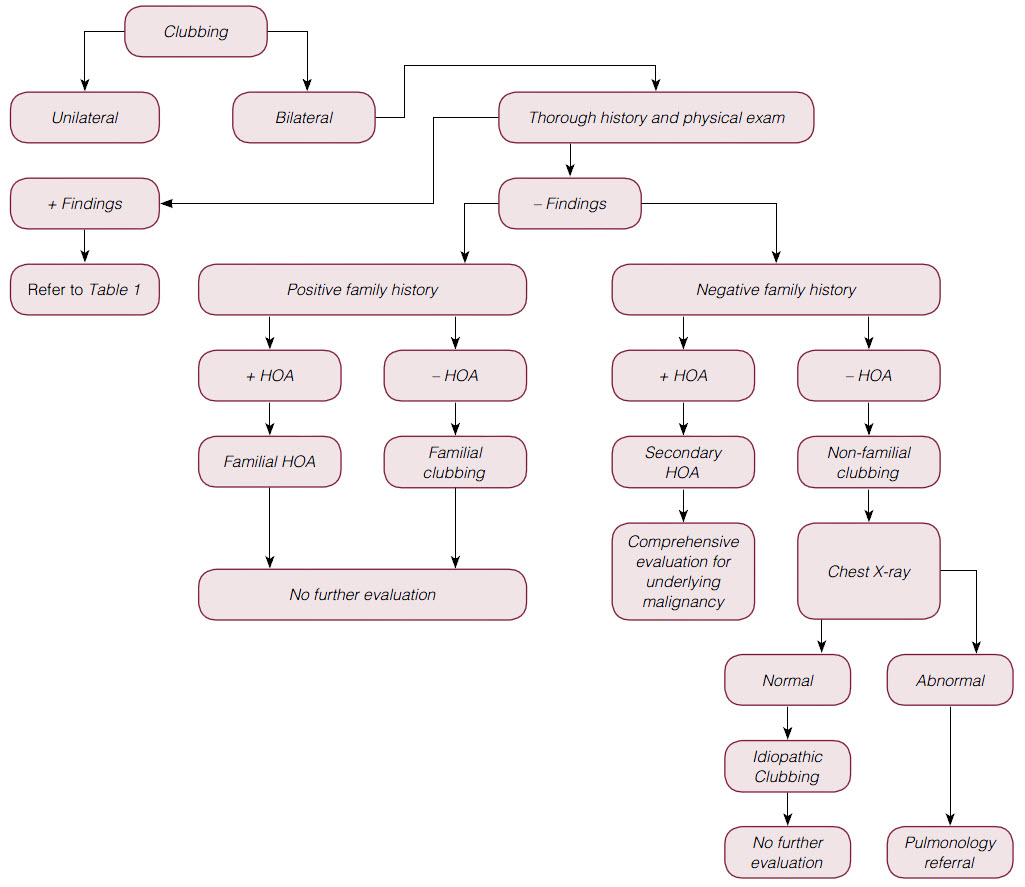 |
| Figure 2. Management of patients with digital clubbing |
The following recommendations for managing patients with digital clubbing with or without HOA are based on a review by Spicknall et al.3 Figure 2 shows the steps in the management of patients with all forms of digital clubbing. First, determine whether the clubbing is unilateral or bilateral. Unilateral clubbing has been observed and is associated with hemiplegia or vascular lesions (dialysis fistula, atrioventricular anastomosis or aneurysm).
In patients with bilateral clubbing, perform a thorough history and physical examination to rule out underlying malignancy, infection or inflammatory conditions. Table 1 lists investigations that could be undertaken if the patient is found to have any positive findings on history or physical examination. If there are no findings on the history or physical examination, the next step is to identify whether the patient has a family history of HOA (positive symptoms for arthralgia and/or bone pain) or clubbing.
Table 1. Suggested investigations and referrals for any positive findings on
history and physical examination
|
|
Positive findings on history and physical examination
|
Investigations/referral
|
|---|
- Cough
- Shortness of breath
- History of smoking
- Exposure to tuberculosis
- Asbestos exposure
|
- Chest X-ray
- PPD
- Consider CT scan of chest
- Consider pulmonology referral
|
- History of congenital cyanotic heart disease
|
- Consider cardiology referral for new cardiac symptoms
|
- Right upper quadrant tenderness
- Jaundice
- Hepatitis risk factors
|
- Check AST/ALT/bilirubin
- Check hepatitis serology
- Consider referral to gastroenterologist if patient is suspected of having primary biliary cirrhosis
|
|
|
- Consider referral to gasteroenterologist if patient is suspected of having inflammatory bowel disease and coeliac sprue
|
- Fever
- Chills
- Night sweats
- Weight loss
|
- FBE, Chest X-ray, PPD
- Consider CT scan of chest/abdomen/pelvis
- Consider blood culture if patient is suspected of having endocarditis
- Consider HIV testing
- Consider referral to haematologist for possible lymphoma
- Consider infectious disease referral for endocarditis/parasite work-up
|
|
|
|
- Exophthalmos
- Pretibial myxedema
|
- TSH
- Free T4
- Consider endocrine referral
|
- Weakness, paresthesias
- Oedema
- Skin findings
- Hepatosplenomegaly
|
- Haematology referral for evaluation for POEMS
|
|
ALT, alanine transaminase; AST, aspartate transaminase; CT, computed tomography; FBE, full blood evaluation; HIV, human immunodeficiency virus; POEMS, polyneuropathy, organomegaly, endocrinopathy, monoclonal gammopathy and skin changes; PPD, purified protein derivative skin test; T4, thyroxine; TSH,
thyroid stimulating hormone
|
 |
| Figure 3. Clubbing involved patient’s finger and toenails |
 |
| Figure 4. Comparison between clubbing and normal digit |
If the patient has a family history of either HOA or clubbing, no further evaluation is needed. However, in patients with non-familial (secondary) HOA, a comprehensive evaluation for underlying malignancy is warranted. In patients with non-familial clubbing without HOA, a screening chest X-ray is recommended. If the chest X-ray is normal, the patient is likely to have idiopathic clubbing and no further investigations are needed.
As this otherwise healthy patient had non-familial clubbing without HOA, a chest X-ray was done. It was negative for any pathological changes. The final diagnosis of idiopathic clubbing was made and no further investigations were performed.
Competing interests: None.
Provenance and peer review: Not commissioned, externally peer reviewed.