What is healthy living?
The term ‘healthy living’ conjures up different images for different individuals. For some, it is a healthy diet and within this, perhaps, is restricted sugar, fat, salt or alcohol intake. For others, it is a regular jaunt to the gym to carry out what they consider state of the art – yoga, aerobics, high-intensity interval training or weightlifting.
Often, however, the less obvious determinants of human health are ignored. These include not just those with a close link to wellbeing, such as regular holidays and reduced stress, but the state of our relationships with family and friends, the healthiness of the environment – both micro (immediate surroundings) and macro (the country, the world) – the benefits of good sleep, our interactions with technology, and our existing and future socioeconomic status. This is what is variously called ‘lifestyle’. Lifestyles and the environments driving these make up a new and adjunct branch of clinical practice known as lifestyle medicine.1,2 This has spurred a movement in health sciences around the world, designed to better cope with the growing tsunami of chronic diseases accompanying advances in human economic development.
A short history of health
Our effectiveness in managing infectious diseases, which have dominated human health throughout history, and the increases in longevity accompanying this, have led to the need for lifestyle medicine. There are things that can be learned from such success. Infections, for example, were countered effectively through the monocausal focus that came from the ‘germ theory’ of the late 19th and early 20th centuries.3 This recognised that not only are infectious diseases caused by microorganisms, but that all the different types of microorganisms (eg bacteria, viruses, protozoa) could be grouped under the single heading ‘germs’. This led to the development of public health, hygiene, immunisation and pharmaceutical developments, as powerful armaments in the war on disease.
Chronic diseases on the other hand, have had no such monocausal focus. They are managed in ‘silos’ (eg heart disease, cancers, respiratory problems), all of which have different, albeit overlapping, levels of ‘causality’.4
However, the discovery of a form of low-grade, systemic and chronic inflammation in the mid-1990s changed this.5 Originally thought to be associated with obesity, and a possible link between obesity and disease, ‘metaflammation’ (for ‘metabolically related inflammation’) has now been shown to be linked to a wide range of chronic diseases in the presence or absence of obesity.6 While it is tricky to discuss ‘causality’ in a non–antigen related ailment, this type of inflammation has been shown to have a number of lifestyle factors as its determinants,7 and these in turn vary in their level of proximity to the actual disease. The list in Figure 1 shows the hierarchy of lifestyle and environmental determinants that define healthy modern living. These have been termed ‘anthropogens’, which are ‘… man-made environments and the lifestyles associated with these, many of which may lead to disease’.8 In essence, they have almost all (except smoking) arisen or become prominent since the beginning of the Industrial Revolution in the late 18th century. It could be considered the ‘downside’ of an otherwise wide-ranging ‘upside’ of human advancement.
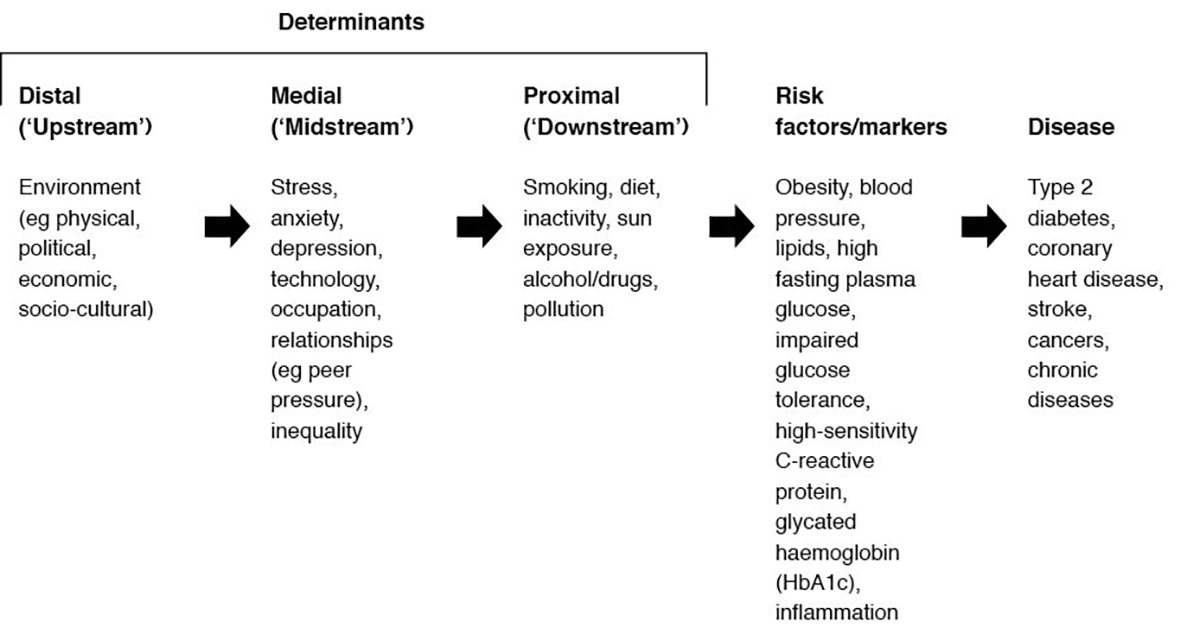
Figure 1. A hierarchy of determinants in chronic disease
Anthropogens and health
So what makes up the category ‘anthropogen’ and what does this tell us about healthy living?
In the typical fashion of epidemiology, an acronym is called for. Hence, the appearance of NASTIE MAL ODOURS, the components of which are spelled out in Table 1. These not only assist those looking for a fuller picture, but form the knowledge base of the new field of lifestyle medicine.9 However, before taking the list on board to share with patients, it is incumbent upon clinicians to be aware that longevity is not necessarily the primary goal, as this has genetic determinants that, to date at least, are difficult to change. The early and embarrassing deaths of many health ‘experts’ from what has been facetiously called ‘Guru’s disease’ testify to the fact that quality of life may be a more readily attainable target than quantity.
Table 1. ‘Anthropogens’ as determinants of chronic diseases
|
|
Determinants
|
Decreases disease risk
|
Increases disease risk
|
|---|
|
Nutrition
|
Fruit/vegetables, dietary fibre, natural foods, food variety, healthy eating patterns, fish, low-dose alcohol
|
High total energy, high energy density, excess processed foods, high glycaemic index foods, saturated or trans fats, sugars, salt, excess alcohol, processed meats, obesity
|
|
(in) Activity
|
Aerobic or resistance exercise, flexibility, stability training
|
Sitting, sedentary work, excessive exercise, obesity
|
|
Stress, anxiety, depression
|
Perceived control, resilience, self-efficacy, coping skills, exercise or fitness, healthy diet
|
Overload, ‘learned helplessness’, early trauma, boredom, caffeine or drug use, excess alcohol use
|
|
Techno-pathology
|
Selective technology use, preventive care, limiting exposure
|
Machinery use, TV or small screens, repetitive actions, excessive noise, weapons of war
|
|
Inadequate sleep
|
Sleep hygiene, healthy diet, exercise or fitness
|
Shift work, excessive entertainment, sleep disorders, interactive media in room, obesity, drugs or alcohol, stress, activity before sleep
|
|
Environment
|
Political or economic structure, ‘nature therapy’, infrastructure for exercise, reduced chemical use
|
Political or economic structure, passive influences, second-hand smoke, particle pollution, endocrine disrupting chemicals, drug immunity (eg antibiotics)
|
|
Meaninglessness
|
Something to do, someone to love, something to look forward to, pro-active self balance
|
Unemployment, displacement, ageing and loss of responsibility, depression, negative affect, early experiences
|
|
Alienation
|
Family relationships, improved parenting, increased competencies
|
Discrimination, early experiences, poor parental support, feelings of isolation, illness, emotional distress, social rejection
|
|
Loss of culture or identity
|
Cultural acceptance and support, conflict resolution, cultural pride or training
|
Warfare, domination by invading culture, displacement
|
|
Occupation
|
Employment, social justice, work equality, economic security
|
Shift work, stress, hazard exposure, conflict, unhealthy interests or habits
|
|
Drugs, smoking, alcohol
|
Social support, relationships, resilience, employment
|
Stress, anxiety, depression, peer or social pressure, addiction, social disadvantage, relationships, social
|
|
Over and under exposure
|
Sunlight (adequate), light, general stimulation
|
Climate, sunlight (excess), sunlight (inadequate), excessive darkness, low humidity, radiation, asbestos
|
|
Relationships
|
Companionship, peer support, maternal support in childhood, ‘love’
|
Loneliness, interpersonal conflict, lack of support, economic insecurity
|
|
Social Inequity
|
Socioeconomic status, education, trust, economic security, support
|
Inequality, poverty, lack of welfare support
|
The list in Table 1 covers 15 determinants, or drivers, of chronic diseases that we know of from different levels of immediacy, as shown in Figure 1. In reality, only three of these are readily considered (nutrition and (in)activity – often called the ‘penicillin of lifestyle medicine’ – and smoking). In fact, these three factors do personally and interactively account for a large proportion of the variance in modern morbidity. However, the remaining 12 not only have an impact individually, but interact with the big three to make up the remainder of the variance. Social inequality,10 for example, can affect the ability to have adequate nutrition, which in turn can affect daily activity levels and sleep, which then might encourage self-medication through drugs and tobacco.
This has changed the nature of our thinking about those factors affecting healthy living. Unlike the single-focus (‘germ theory’) approach to infectious diseases, which can be managed in a ‘linear’ fashion (eg disease ---> treatment ---> disease resolution), ‘anthropogens’ need to be considered in a ‘systems’ model, where everything interacts with everything else (Figure 2) and feedback can influence outcomes. The notion of considering diet alone to manage obesity is therefore akin to using a loofa to manage dermatitis.
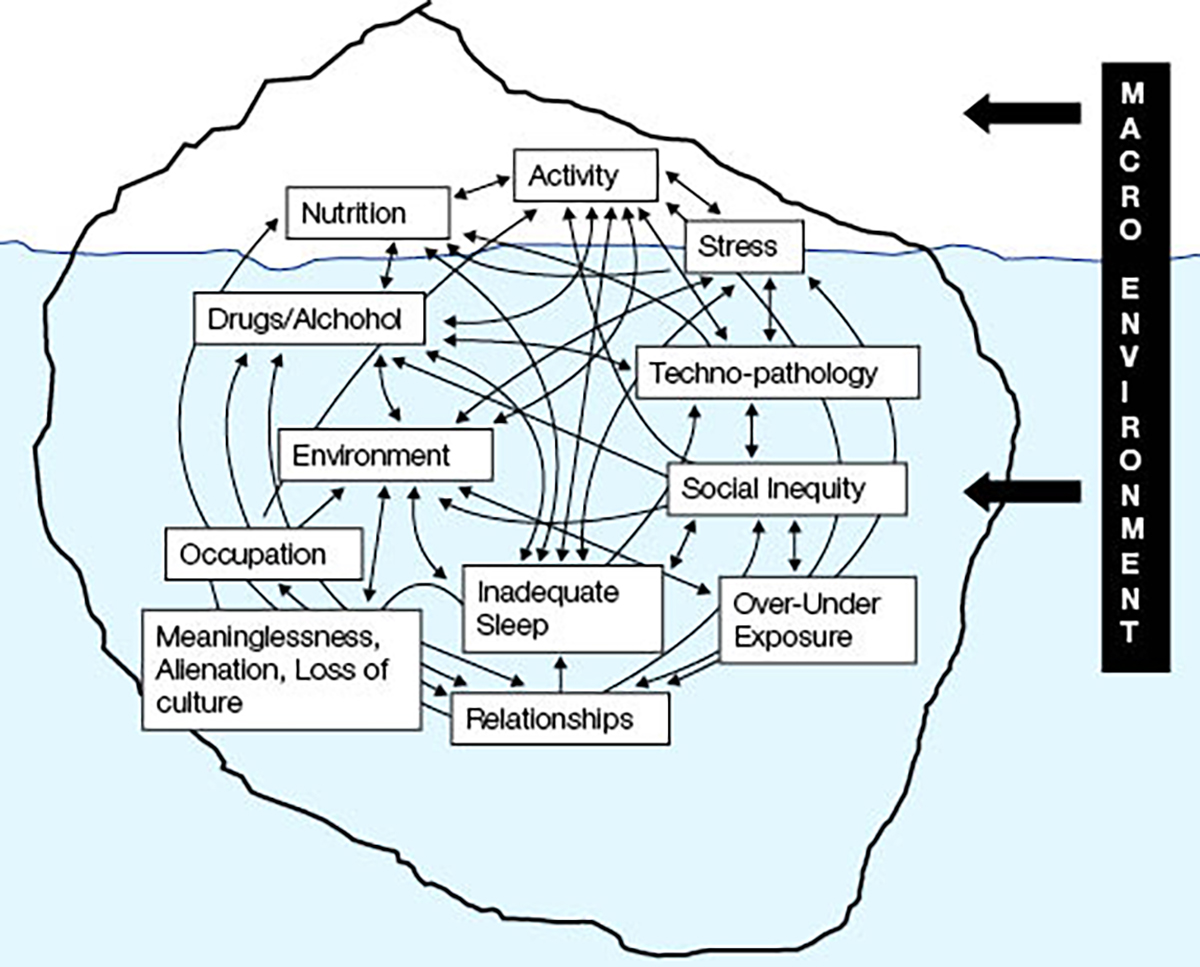
Figure 2. A ‘systems’ model of lifestyle and environmental determinants of chronic disease
In a practical sense, this means not only focusing on those aspects of the NASTIE MAL ODOURS determinants that may be obvious risk factors, but on other determinants, sometimes much broader and outside the clinical sector (eg social inequality) that feedback on the obvious. Getting all the ducks lined up may be difficult in order to ensure healthy living (particularly considering currently unchangeable determinants such as genetics), but at least an awareness of these influences is vital for a holistic approach to health management.
Conclusion
The requirements for healthy living change within the changing social structures in which humans have evolved. Hunter–gatherers, for example, were predisposed to infections and injury from predators and warfare; those living around the time of the agrarian revolution were predisposed to zoonotic diseases through their close proximity to animals. Strangely, aspects of population health, at least as indicated by declining obesity, improved during the war years in many countries only to be later replaced by the chronic ‘diseases of civilisation’ of the late 20th and early 21st centuries.
It is unlikely that such changes, and the demands they put on health systems evolving to keep up, will decrease. Healthy living in the epoch of the Holocene had different requirements to those in what has been proposed as the age of the Anthropocene, or the modern era, in which human activity has been the dominant influence on the biosphere. While the technological revolution, which makes up the early stages of the modern era, will undoubtedly provide great advances in human disease management, it is unlikely to eliminate all future disease and suffering, or the need for individual and regulatory involvement for healthy living.
Key points
- The nature of diseases changes with the nature of the societies in which these occur.
- We currently live in an era of chronic diseases for which there is no ‘mono-causal’ focus.
- Chronic diseases have lifestyle and environment determinants or ‘anthropogens’.
- While nutrition and exercise are often considered the main focus of healthy living, there are several other anthropogens that need to be considered.
- These interact in a ‘systems’ fashion, unlike the linear models of past infectious diseases.
Authors
Garry Egger AM, MPH, PhD, Professor, Health and Human Sciences, Southern Cross University, Lismore, NSW. eggergj@ozemail.com.au
Competing interests: None.
Provenance and peer review: Commissioned, externally peer reviewed.