The rise of oropharyngeal cancer
The incidence of oropharyngeal cancer (OPC) is rising in parallel with increasing rates of human papillomavirus (HPV) infection.1,2 The 225% increase in population-level incidence is being referred to as an ‘epidemic’ internationally.3 Australian data indicate a significant increase in the proportion of HPV-associated OPC from 20% in 1987 to 64% in 2010.4 The demographic of HPV-associated OPC is typically middle-aged, affluent males, in contrast to conventional oral cavity squamous cell carcinoma (SCC), which is more common in elderly patients from low socioeconomic backgrounds and with a history of smoking and alcohol consumption.5,6
Traditionally, definitive treatment of oropharyngeal SCC has involved chemoradiotherapy (CRT) or radical surgery with mandibulotomy and neck dissection for salvage treatment of advanced disease.7 Despite allowing organ preservation, CRT requires daily treatments over six to seven weeks, and is associated with various morbidities, including mucositis, xerostomia, loss of taste, impaired speech and swallowing, dental caries, and osteoradionecrosis. Likewise, open surgery is associated with significant morbidities and requires an extended hospital stay.2
The evolution of trans-oral robotic surgery (TORS) has begun to transform the management of OPC.
What is TORS?
TORS is a minimally invasive surgical alternative for the treatment of various benign and malignant head and neck pathologies. It is performed under general anaesthesia and has been shown to be cost-effective, with significantly shorter hospital stays and fewer treatment-related costs.8
In the 1990s, there were three main robotic surgical systems. At present, however, only one system is being marketed. New robotic systems that are being developed will become available over time. The robotic system consists of three parts (Figure 1):9
- a console with which the surgeon (seated) remotely controls the robotic arms
- a patient-side robotic cart with three robotic arms positioned inside the oral cavity – one handling the 12-mm endoscopic camera and two holding 5 mm EndoWrist instruments
- a high-definition, three-dimensional vision cart.
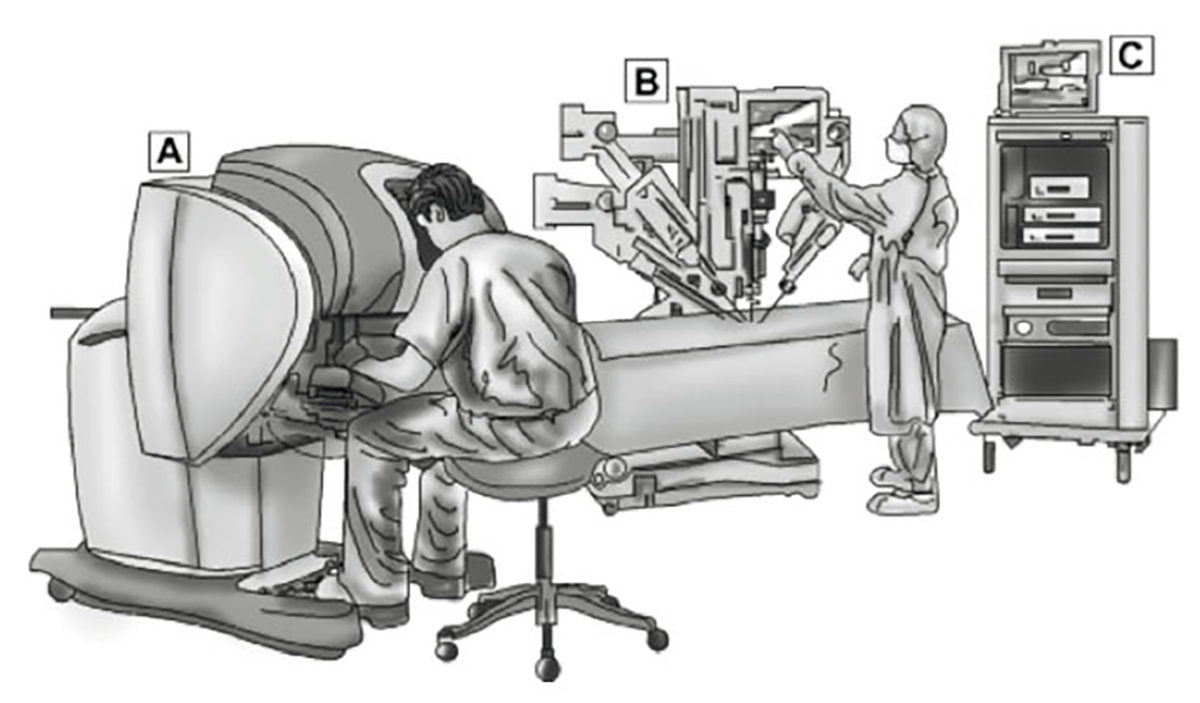
Figure 1. Illustration of surgical system robot
A, surgeon’s console; B, patient-side robotic cart; C, high-definition, 3D vision cart
Reproduced from Garg A, Dwivedi RC, Sayed S, et al. Robotic surgery in head and neck cancer:
A review. Oral Oncol 2010;46(8):571–76, with permission from Elsevier.
TORS has numerous advantages over conventional endoscopic surgery. High‑resolution, three-dimensional optics and magnification allow for excellent visualisation. Wristed instruments provide increased range of motion, enabling delicate tissue handling and enhanced surgical precision with the elimination of tremor. Technically challenging tasks such as endoscopic suturing may also be performed with relative ease robotically.9
History of robotic surgery
The first human surgical procedures to use robotic technology were performed in the 1980s.10 Since then, robotic surgery has enabled various cardiac, urological and abdominopelvic procedures to become minimally invasive.
After experimentation in animal and cadaveric models, TORS made its human debut in 2005, with the successful excision of a vallecular cyst in a woman aged 46 years. From 2006–07, the feasibility and safety of TORS was demonstrated in preclinical and clinical trials at the University of Pennsylvania.11–13 This led to its approval by the US Food and Drug Administration (FDA) in December 2009 for the treatment of selected benign and malignant head and neck tumours.14
Which patients may be candidates for TORS?
The leading indication for TORS is excision of T1–T2 (up to 4 cm) oropharyngeal carcinomas, including tumours of the tonsils, base of tongue and soft palate.15 TORS may also be used to remove other benign and malignant neoplasms of the oropharynx, hypopharynx and larynx. Other procedures that have been safely performed using TORS include base of skull surgery, supraglottic partial laryngectomy, total laryngectomy, parapharyngeal tumours, closure of paediatric laryngeal clefts and reconstructive procedures.9,15
Tumours in the oral cavity (anterior to the junction of hard and soft palate) are generally not treated with TORS (with the exception of tumours in the posterior tongue) as access is usually good.15
Contraindications to TORS
The main contraindications to TORS are trismus (reduced mouth opening), incomplete lesion visualisation due to unfavourable anatomy, and tumour involvement of the mandible, posterior pharyngeal wall, internal carotid artery, prevertebral fascia or >50% of the base of the tongue. Factors that may limit surgical exposure include narrow-arched mandible, trismus and retrognathia.12,16 As with all surgery, patient cardiopulmonary status and comorbidities must be considered when determining eligibility.
TORS compared with conventional treatment options
The oropharynx is a difficult area to access. Several surgical approaches have been described to enable adequate exposure. Typically, this requires cutting the lower lip and bone of the mandible (mandibulotomy). The mandible is ‘swung’ laterally to expose the tongue base and tonsils, and the lingual nerve is often removed to improve access. These radical operations often take 8–10 hours because of the extensive dissection, need for associated tracheostomy and free flap reconstruction to close the large defect that is created. Trans-oral laser surgery is a minimally invasive alternative, but has limited visualisation and is technically challenging because of the need to use long manipulators.9
Over the past decade, TORS has emerged as the principal minimally invasive modality that overcomes these limitations. The trans-oral surgical approach avoids the need for external incision and thus confers the advantage of no facial scarring. Compared with traditional open surgery, TORS has been shown to have better cosmetic results, less blood loss, fewer complications, less postoperative pain, lower rates of intensive care unit admission, reduced operative time, and reduced length of hospitalisation.2 Most patients who undergo TORS are able to return to normal speech and swallowing, with lower requirements for tracheostomy and gastrostomy tubes.16,17,18
In one-third of patients, TORS is effective as a single-modality therapy.19 This spares patients the adverse effects of CRT and offers the advantage of a single hospital stay rather than multiple outpatient visits. This is particularly advantageous for patients living in rural or remote regions of Australia who have to travel long distances to receive treatment. Although the majority (67%) of patients will still require adjuvant radiotherapy or chemotherapy, the dose, treatment volumes and duration of treatment may be reduced, translating into reduced side effects.20 A recent study from the University of California found that swallowing was significantly better in patients who underwent TORS with adjuvant radiotherapy compared with definitive CRT.21 Both modalities were associated with excellent survival and locoregional control. Hence, both are considered acceptable treatment options for oropharyngeal cancer.21
Limitations of TORS
There are several barriers to the widespread use of TORS:22
- Cost – estimated costs are $4 million for initial installation, $150,000 annual maintenance fee and $1000 per case for disposable instruments
- Size – the unit occupies considerable space and requires additional theatre time and staff for set-up
- Although TORS has a favourable learning curve, additional training overseas and in Australia is required before surgeons can be credentialled.
Key points
- TORS is a minimally invasive surgical alternative for treatment of some head and neck pathologies, including tumours of the oropharynx, hypopharynx and larynx.
- TORS has numerous advantages when compared with traditional open surgery or trans-oral laser surgery, including no facial incisions, fewer complications and reduced length of hospitalisation.
Authors
Wendy Sijia Liu MBBS, Junior Medical Officer, Royal North Shore Hospital, St Leonards, NSW
Alex Limmer MBBS (Hons1), Junior Medical Officer, Liverpool Hospital, Liverpool, NSW
Joe Jabbour BMedSci (Hons1) MBBS (Hons1), Junior Medical Officer, Westmead Hospital, Westmead, NSW
Jonathan Clark FRACS, MBiostat, Head and Neck Surgeon, Royal Prince Alfred Hospital & Chris O’Brien Lifehouse; Director of Fellowship Program and Research, Sydney Head and Neck Cancer Institute, Chris O’Brien Lifehouse, Camperdown, NSW; Conjoint associate professor, Central Clinical School, University of Sydney, NSW, South West Clinical School, University of New South Wales, NSW, Western Sydney University, NSW. Jonathan.Clark@lh.org.au
Competing interests: None.
Provenance and peer review: Not commissioned, externally peer reviewed.