Dysmenorrhoea, or painful menstruation, is a common symptom of menses.1,2 Dysmenorrhoea is defined as a painful, cramping sensation in the lower abdomen or back associated with menstrual periods3 and is classified into primary and secondary types. Primary dysmenorrhoea is painful menstrual periods, not due to other diseases, and often occurs soon after menarche. Secondary dysmenorrhoea is due to an underlying pelvic abnormality, such as endometriosis, and can be either new-onset or a change in the nature of the dysmenorrhoea (intensity, duration) over time.4
Dysmenorrhoea has been examined in Australian women in only a small number of studies, mostly involving adolescent girls recruited from secondary schools.2,5 The national prevalence of dysmenorrhoea is 70–90%,2 which is comparable to that reported worldwide. Although dysmenorrhoea is a common problem faced by women, many are reluctant to consult their doctor about it.6
We evaluated the prevalence and severity of dysmenorrhoea using online questionnaires at two time points in a cohort of women aged 16–29 years. We assessed the impact of menstrual pain and its severity on relationships, productivity, health and wellbeing. We also sought to determine the level of concern in young women regarding dysmenorrhoea, and their use of available treatments.
Methods
Study design
The Young Female Health Initiative (YFHI)7 and Safe-D studies8 are the first comprehensive prospective studies in which clinical and self-reported data are collected relating to sexual and mental health, lifestyle and wellbeing in young Australian women.
Ethics
The YFHI study was approved by the Human Research and Ethics Committee (HREC) at the Royal Women’s Hospital (approval number 11/14), and the Safe-D study by Melbourne Health HREC (approval number 2013.007). Procedures followed were in accordance with the Helsinki Declaration of 2000 as revised in 2002.
Recruitment and inclusion criteria
Eligible participants were females aged 16−25 years and living in Victoria, Australia.7,8 Advertisements were posted on Facebook to recruit women into two general health studies called YFHI and Safe-D.
Clicking on the advertisement directed respondents to secure websites containing more information and where expressions of interest were registered. Prospective participants were then contacted by investigators and consented into the study.
Participation included the completion of a web-based questionnaire, using SurveyMonkey (www.surveymonkey.com) or Limesurvey (www.limesurvey.org), covering demographics, mental health, lifestyle and reproductive health. Existing participants from YFHI and the Safe-D study who had consented to be contacted for future studies were invited to fill in a follow-up dysmenorrhoea questionnaire.
Collection of dysmenorrhoea data
Dysmenorrhoea was defined as ‘period pain’ of any severity in the six months preceding questionnaire completion. The nature of the dysmenorrhoea was ascertained according to time of onset in relation to menarche (‘primary onset’ at menarche, versus ‘secondary onset’ some years after menarche). This is not a reflection of whether the dysmenorrhoea itself was primary or secondary, as information on underlying disease was not ascertained for all participants.
The severity of pain and level of interference with daily activities were measured on a Likert scale (1 [little] to 10 [severe]). This rating was used to categorise participants according to the Numerical Rating Scale (NRS) for pain, which is useful in the assessment of dysmenorrhoea.9 A rating of 1–3 was considered mild pain, 4–6 as moderate pain and 7–10 as severe pain.
Statistical analyses
Statistical analyses were performed using Stata version 11.1 (StatCorp LP, College Station, TX, USA). Analyses for associations between dysmenorrhoea and categorical variables were performed using Fisher’s exact test. Ordered logistic regression was performed to determine the risk of interference on aspects of daily living. A two-sided P <0.05 was defined as statistically significant.
It is important to note that there were missing data from participants for various questions (4−10%). Therefore, we present prevalence estimates using different denominators for a number of questions.
Results
Baseline questionnaire data were available from 250 YFHI respondents and 228 Safe-D participants. Follow-up questionnaires were completed by 247 participants (YFHI n = 141, Safe-D n = 106; Figure 1). This represented a 69% response rate (247/359).
A difference in age was found between YFHI and Safe-D participants who completed the follow-up questionnaire (Figure 1). However, after adjustment for a delay in the inclusion of participants aged 16–17 years in the YFHI study, no differences in age were observed. Thus, the two data sets were collated and the results of pooled data are presented in this paper.
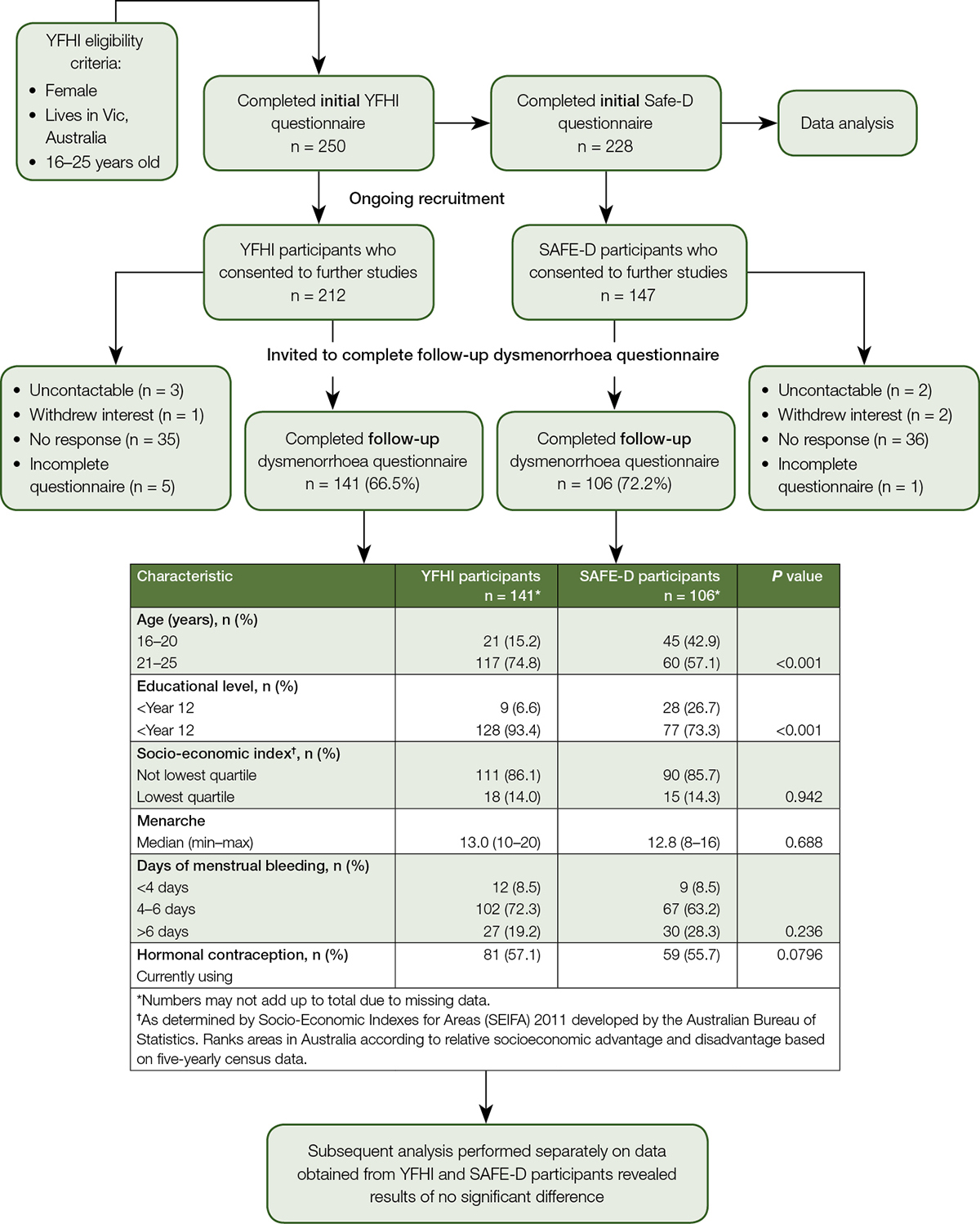
Figure 1. Sample derivation for follow-up dysmenorrhoea questionnaire from Young Female Health Initiative (YFHI) and Safe-D participants
Descriptive statistics
Dysmenorrhoea was reported by 88% (n = 207/236) of respondents who completed the follow-up dysmenorrhoea questionnaire and had had a period in the past 12 months. This was comparable to the prevalence found in the respondents who completed the baseline questionnaires (86%, n = 369/431). Those who reported dysmenorrhoea at baseline did not differ, with respect to age, marital status or education level, from those not reporting dysmenorrhoea. However, a greater proportion of those who experienced dysmenorrhoea reported depression (32% versus 19%, P = 0.04) and had experienced a pregnancy (24% versus 4%, P = 0.02; Table 1).
Table 1. Characteristics of respondents who experienced dysmenorrhoea versus those who did not at baseline
|
Topics
|
Dysmenorrhoea* n = 369
|
No dysmenorrhoea* n = 62
|
P value
|
|---|
|
Age (years) mean ± SD
|
21.5 ± 2.7
|
21.4 ± 2.4
|
0.8
|
|
Marital status
|
|
|
|
|
Never married
|
315 (87.3)
|
53 (85.5)
|
0.7
|
|
Married/de facto
|
44 (12.7)
|
9 (14.5)
|
|
|
Level of education
|
|
|
|
|
No tertiary qualification
|
105 (28.8)
|
18 (29.0)
|
0.7
|
|
Undergraduate (or equivalent)
|
231 (63.3)
|
41 (66.1)
|
|
|
Postgraduate (or equivalent)
|
29 (8.0)
|
3 (4.8)
|
|
|
Employment
|
|
|
|
|
No paid employment
|
103 (28.2)
37 (10.1)
|
22 (35.5)
5 (8.1)
|
0.2
|
|
Labourer or related work
|
81 (22.2)
144 (39.5)
|
7 (11.3)
28 (45.2)
|
|
|
Managerial or professional occupation
|
|
|
|
|
Clerical or related work
|
|
|
|
|
SEIFA quartiles†
|
|
|
|
|
Not lowest quartile
|
309 (84.7)
|
47 (77.1)
|
0.1
|
|
Lowest quartile
|
56 (15.3)
|
14 (23.0)
|
|
|
Current smoker
|
40 (11.3)
|
8 (13.3)
|
0.6
|
|
Alcohol consumption in the last 12 months
|
|
|
|
|
≤Once a month
|
91 (32.2)
|
19 (39.6)
|
0.5
|
|
2–3 days a month
|
70 (24.7)
|
11 (22.3)
|
|
|
1–2 days a week
|
92 (32.5)
|
16 (33.3)
|
|
|
≥3 days a week
|
30 (10.6)
|
2 (4.2)
|
|
|
Depression
|
117 (32.1)
|
12 (19.4)
|
0.04
|
|
Experienced a pregnancy
|
24 (8.8)
|
4 (8.5)
|
0.02
|
|
Current hormonal contraception use
|
134 (36.4)
|
24 (38.7)
|
0.7
|
|
SEIFA, Socio-Economic Indices for Areas.*n (%) unless specified otherwise; †As determined by Socio-Economic Indexes for Areas (SEIFA) 2011 developed by the Australian Bureau of Statistics. Ranks areas in Australia according to relative socioeconomic advantage and disadvantage based on five-yearly census data. There were missing data for information regarding the prevalence of dysmenorrhoea for 47 participants. Numbers may not add up to 100% due to missing values.
|
At follow-up, 19% reported mild dysmenorrhoea, 49% moderate and 32% severe. Dysmenorrhoea commenced at menarche for 70% (n = 144/207) of respondents (‘primary onset’ dysmenorrhoea), while for 30% (n = 63/207) dysmenorrhoea commenced some years after menarche (‘secondary onset’ dysmenorrhoea).
Primary versus secondary onset dysmenorrhoea
No significant differences were observed between those who reported primary onset of dysmenorrhoea and secondary onset of dysmenorrhoea with regards to age (21.8 ± 2.5 versus 21.4 ± 2.6; P = 0.02), current use of hormonal contraceptives (60% versus 51%; P = 0.2) and severity of dysmenorrhoea (P = 0.7).
Reported management options for dysmenorrhoea
At follow-up, use of pain medication was reported by 58% (n = 120/206) of respondents with dysmenorrhoea. Pain medication included paracetamol, aspirin, mefenamic acid and ibuprofen. Those with severe dysmenorrhoea were more likely to use pain medication when compared with those who experienced moderate or mild period pain (73% versus 56% and 30%, respectively; P = 0.001).
Hormonal contraception was used by 57% (n = 140/247) of women, with 74% using the combined oral contraceptive pill (COCP), 13% etonogestrel implant, 9% levonorgestrel intrauterine device, 2% progestogen-only oral contraceptive pill, and 2% medroxyprogesterone acetate injection. Period pain was the reason for using hormonal contraception in 36% (n = 45/117). There was no significant difference in hormonal contraceptive use between respondents who experienced dysmenorrhoea and respondents who did not (P = 0.6).
Most respondents with dysmenorrhoea (92%; n = 190/207) indicated using non-pharmacological measures, either alone or in conjunction with analgesics, to relieve period pain. The use of heat packs was most popular, with 54% (n = 112) reporting their use, followed by hot baths (37%; n = 77), meditation (7%; n = 15) and exercise (2%; n = 3).
Association between dysmenorrhoea and consultations
Only 34% (n = 71/207) of those with dysmenorrhoea had ever consulted a healthcare provider about period pain. Participants with severe dysmenorrhoea (53%; n = 34/64) were more likely to consult their healthcare provider than those with mild (13%; n = 5/39) or moderate (31%; n = 30/98) dysmenorrhoea (P <0.001). Approximately 86% (n = 176/206) who experienced dysmenorrhoea had sought information about period pain from other sources (eg internet, social media, friends, magazines), including 34% (n = 69/206) who obtained information from family members.
Impact of dysmenorrhoea on quality of life
More severe dysmenorrhoea was associated with greater risk of interference in numerous aspects of daily living (work/study attendance and productivity; relationships with family, friends and partners; exercise; sexual activity [P <0.001; Table 2]). Among respondents experiencing dysmenorrhoea, 24% (n = 50/207) required time off work or study in the preceding six months because of the pain. Taking time off because of period pain was associated with the severity of dysmenorrhoea (52% [n = 33/64] in severe dysmenorrhoea, 15% [n = 15/98] in moderate and 3% [n = 1/39] in mild; P <0.001).
Table 2. Relationship between severity of dysmenorrhoea and impact on normal daily activities
|
Interference
|
Mild n (%)
|
Moderate n (%)
|
Severe n (%)
|
P value
|
OR† (95% CI‡)
|
|---|
|
Daily activities
|
|
|
|
|
|
|
None
|
8 (20.5)
|
7 (7.2)
|
0 (0)
|
|
|
|
Mild
|
31 (79.5)
|
70 (72.2)
|
26 (41.9)
|
<0.001
|
7.1
(4.2–12.0)
|
|
Moderate
|
0 (0)
|
19 (19.6)
|
12 (19.4)
|
|
|
|
Major
|
(0)
|
1 (1.0)
|
24 (38.7)
|
|
|
|
Work/study attendance
|
|
|
|
|
|
|
None
|
3 (37.5)
|
9 (19.2)
|
3 (6.0)
|
|
|
|
Mild
|
5 (62.5)
|
26 (55.3)
|
15 (30.0)
|
<0.001
|
3.1
(1.3–7.6)
|
|
Moderate
|
0 (0)
|
10 (21.3)
|
15 (40.0)
|
|
|
|
Major
|
0 (0)
|
2 (4.3)
|
12 (24.0)
|
|
|
|
Work/study productivity
|
|
|
|
|
|
|
None
|
6 (46.2)
|
9 (14.8)
|
4 (7.7)
|
|
|
|
Mild
|
6 (46.2)
|
34 (55.7)
|
20 (38.5)
|
<0.001
|
3.7
(2.1–6.5)
|
|
Moderate
|
1 (7.7)
|
16 (26.2)
|
11 (21.2)
|
|
|
|
Major
|
0 (0)
|
2 (3.3)
|
17 (32.7)
|
|
|
|
Friendships
|
|
|
|
|
|
|
None
|
3 (60.0)
|
14 (26.4)
|
6 (14.3)
|
|
|
|
Mild
|
2 (40.0)
|
28 (52.8)
|
14 (33.3)
|
0.002
|
3.9
(1.9–7.7)
|
|
Moderate
|
0 (0)
|
11 (20.8)
|
15 (35.7)
|
|
|
|
Major
|
0 (0)
|
0 (0)
|
7 (16.7)
|
|
|
|
Family relationships
|
|
|
|
|
|
|
None
|
6 (66.7)
|
13 (24.1)
|
5 (12.2)
|
|
|
|
Mild
|
3 (33.3)
|
30 (55.6)
|
14 (34.2)
|
<0.001
|
4.7
(2.4–9.0)
|
|
Moderate
|
0 (0)
|
11 (20.4)
|
15 (36.6)
|
|
|
|
Major
|
0 (0)
|
0 (0)
|
7 (17.1)
|
|
|
|
Relationship with partner
|
|
|
|
|
|
|
None
|
3 (30.0)
|
9 (16.1)
|
3 (8.1)
|
|
|
|
Mild
|
7 (70.0)
|
26 (46.4)
|
12 (32.4)
|
0.004
|
3.2
(1.7–5.9)
|
|
Moderate
|
0 (0)
|
18 (32.1)
|
12 (32.4)
|
|
|
|
Major
|
0 (0)
|
3 (5.4)
|
10 (27.0)
|
|
|
|
Sexual activity
|
|
|
|
|
|
|
None
|
1 (5.6)
|
3 (4.3)
|
1 (2.2)
|
|
|
|
Mild
|
9 (50.0)
|
23 (32.9)
|
7 (15.6)
|
0.005
|
2.7
(1.6–4.6)
|
|
Moderate
|
4 (22.2)
|
18 (25.7)
|
6 (13.3)
|
|
|
|
Major
|
4 (22.2)
|
26 (37.1)
|
31 (68.9)
|
|
|
|
Exercise
|
|
|
|
|
|
|
None
|
7 (26.9)
|
5 (5.8)
|
2 (3.6)
|
|
|
|
Mild
|
16 (61.5)
|
37 (43.0)
|
12 (21.4)
|
<0.001
|
4.9
(3.0–7.9)
|
|
Moderate
|
3 (11.5)
|
30 (34.9)
|
12 (21.4)
|
|
|
|
Major
|
0 (0)
|
14 (16.3)
|
30 (53.6)
|
|
|
|
CI, confidence interval; OR, odds ratio
†Odds ratio, as determined by ordinal logistic regression analyses
‡95% confidence interval
|
Discussion
The very high prevalence of dysmenorrhoea among the study participants falls within the range reported in a systematic review conducted by the World Health Organization.10 A greater proportion of those who experienced dysmenorrhoea also reported depression, compared with those who did not. This finding is supported by that reported in a case-control study comprising 424 adolescents,11 and is intuitive as dysmenorrhoea may have a negative impact on quality of life.
While a large proportion of women reported moderate to severe dysmenorrhoea, approximately 60% of these used pain medication for relief. By contrast, 82% of women with moderate or severe dysmenorrhoea reported using non-pharmacological measures, such as heat therapy, despite the limited and inconsistent evidence for their efficacy in dysmenorrhoea.12 The discrepancy between the use of pharmacological and non-pharmacological measures may suggest inherent resistance in young women towards the use of pharmacological analgesics. Alternatively, there may be a lack of knowledge of pharmacological treatments for dysmenorrhoea. Further research may shed more light on these issues.
It is surprising that there was no relationship between COCPs and dysmenorrhoea, given the high prevalence of dysmenorrhoea in our cohort and that COCPs are widely used for the treatment of dysmenorrhoea in both sexually active and non–sexually active women.13 This unexpected finding may reflect the wide variety of indications for the use of hormonal contraception in young women, regardless of whether they experienced dysmenorrhoea. Indeed, approximately one-third of women using hormonal contraception stated that dysmenorrhoea was the reason for use of these agents. We did not assess the level of alleviation women with dysmenorrhoea achieved with the use of hormonal contraception. Data pertaining to their use and effectiveness was not obtained in this study and represents an avenue for further research in this group of women.
Although severe pain was more likely to prompt a consultation than milder pain, the majority of women with moderate to severe dysmenorrhoea had never sought medical attention for dysmenorrhoea. The low frequency with which women seek medical attention for dysmenorrhoea has been previously described.6 This is particularly relevant in young women who perceive dysmenorrhoea to be a common menstrual complaint that needs to be tolerated, and thus find difficulty determining if and when to seek medical attention.6 By contrast, 86% of women with dysmenorrhoea had sought information about period pain from other sources such as the internet and family members. These sources may be perceived as ‘more accessible’ to young women than a healthcare practitioner, but represent a greater potential for misinformation. These findings highlight the need for accessible, reliable and helpful information with which young women are comfortable.
A three-pronged approach could be taken to better inform young women of dysmenorrhoea and associated support services. First, informative leaflets could be handed out to girls in schools by the school nurse so that adolescent females are familiar with the symptoms for dysmenorrhoea, which they can observe, and for which they can contact their GP if they require prescription pain medication. Second, health professionals could be more proactive in asking about this sensitive topic so that if young women have dysmenorrhoea they may be more likely to discuss their pain. Third, given the information-seeking behaviours reported in this sample, health professionals and schools could promote the use of reliable websites on which accurate information on dysmenorrhoea is published.
Dysmenorrhoea significantly affects the quality of life of females in our sample. Approximately 50% of women with severe dysmenorrhoea reported time off, compared with only 2.6% with mild dysmenorrhoea. Given that 80% of women in our study reported moderate to severe dysmenorrhoea, this represents a significant recurrent burden not only for the women themselves, but also for the workforce and economy.
A major strength of this study is that we were able to gain an insight into the experience of young women with dysmenorrhoea in a representative general population of young females. When compared with national data for this age group, a greater proportion of participants in our study had attained tertiary education. However, no other significant differences were observed. Therefore, our findings should be generalisable to a general population of young females.
There were a number of potential limitations. The sample size only allowed an estimation of dysmenorrhoea prevalence. Additionally, the definitions of primary onset and secondary onset dysmenorrhoea were from self-report rather than proven pathology.
Conclusion
The prevalence of dysmenorrhoea is critically high in this sample of young females, with many indicating that pain had a significant adverse impact on numerous daily activities. However, a large proportion did not use pain medication and obtained information about dysmenorrhoea from sources other than health professionals, which poses a large risk of misinformation and a potential barrier to seeking early medical advice. Therefore, educational materials, information on reliable websites and guidance about dysmenorrhoea and treatment options should be made readily available to young women in schools as well as by health professionals.
Implications for general practice
Dissemination of accurate information about treatment options for dysmenorrhoea in Victoria may improve the quality of life of young females.
Authors
Asvini K Subasinghe PhD, Research Fellow, Department of Microbiology and Infectious Diseases, Royal Women’s Hospital, Parkville, Vic; Infection and Immunity, Murdoch Childrens Research Institute, Parkville, Vic. asvini.subasinghe@gmail.com
Lina Happo PhD, medical student, Department of Medicine, University of Melbourne, Parkville, Vic
Yasmin L Jayasinghe MBBS, FRANZCOG, PhD, Paediatric and Adolescent Gynaecologist, Department of Obstetrics and Gynaecology, University of Melbourne, Royal Women’s Hospital, Parkville, Vic; Department of Gynaecology, Royal Children’s Hospital, Parkville, Vic
Suzanne M Garland MBBS, MD, FRCPA, FAChSHM, FRANZCOG, Professor, Director of Microbiology and Infectious Diseases, Department of Microbiology and Infectious Diseases, Royal Women’s Hospital, Parkville, Vic; Infection and Immunity, Murdoch Childrens Research Institute, Parkville, Vic; Department of Obstetrics and Gynaecology, University of Melbourne, Royal Women’s Hospital, Parkville, Vic
Alexandra Gorelik MSc, Biostatistician, Department of Medicine, University of Melbourne, Parkville, Vic; Melbourne EpiCentre, Royal Melbourne Hospital, Parkville, Vic
John D Wark MBBS, FRACP, PhD, Professor, Endocrinologist, University of Melbourne Department of Medicine and Bone & Mineral Medicine, Royal Melbourne Hospital, Parkville, Vic
Competing interests: Dr Garland reports grants from Merck, GSK, CSL, Commonwealth Department of Health, and non-financial support from Merck, outside the submitted work; and has delivered lectures and received speaking fees from MSD and SPMSD for work performed in personal time.
Provenance and peer review: Not commissioned, externally peer reviewed.
Acknowledgements
We thank the YFHI and Safe-D research teams and participants for their time. YFHI was supported by an Australian NHMRC program grant (568971) and Safe-D study by a NHMRC project grant (1049065).