The central nervous system (CNS) is primarily imaged using computed tomography (CT) and magnetic resonance imaging (MRI). Other modalities, such as positron emission tomography (PET), are used in specific specialist applications or research in close collaboration with neurologists, neurosurgeons and psychiatrists. The use of ultrasonography is mainly limited to assessment of infants prior to closure of the fontanelles.
Computed tomography
Advantages and disadvantages
Compared with MRI, the main advantages of CT are greater availability, lower cost and shorter acquisition time. It is generally the modality of choice for the initial assessment of acute intracranial conditions. Its shorter acquisition time allows reasonable image quality in noncompliant patients who may be confused and/or restless.
The main drawbacks of CT are the use of ionising radiation and the potential risks of intravenous contrast agents when required (contrast-induced nephropathy and allergic reactions). Soft tissue resolution of CT is not as good as that of MRI1 and images of the posterior fossa undergo a greater degree of degradation because of artefact from adjacent bony structures.
Requesting CT scans
CT is the modality of first choice in acute stroke because of ready availability and quick acquisition time (Table 1). Its primary role in the setting of acute stroke is the exclusion of intracranial haemorrhage and stroke mimics, such as tumours. In hyperacute ischaemic stroke, CT may be negative for the first few hours. Early signs of brain infarction are detected on a non-contrast CT in up to 61% of cases within six hours. The sensitivity increases substantially after 24 hours.2
Table 1. Common indications for computed tomography brain and spine
|
Brain
|
Spine
|
|---|
|
Stroke
|
Trauma
|
|
Trauma
|
Back and neck pain with radicular symptoms
|
|
Thunderclap headache
|
Back and neck pain with sinister features
|
|
Acute headache
|
Spinal infection when magnetic resonance imaging or nuclear medicine are not available
|
|
Atypical headache
|
|
|
Delirium
|
|
|
Coma
|
|
|
Ventriculo-peritoneal shunt assessment
|
|
CT is also the modality of choice in trauma. It is very sensitive for acute haemorrhage, skull fractures and spinal fractures. In spinal imaging, CT is useful in trauma, atypical back and neck pain when aggressive pathology is suspected, and in back and neck pain with associated radicular symptoms.
Contrast or non-contrast study
Non-contrast studies of the brain and spine are sufficient for most indications. Diagnosis of common conditions such as cerebral infarction and haemorrhage can be made without intravenous contrast.
A contrast-enhanced CT of the brain is of value in specific situations (eg known CNS tumour, investigation for potential intracranial metastases, CNS infection). In addition, the imaging team may detect an unexpected abnormality on the plain scan at the time of scanning that warrants contrast administration.
CT neck and cerebral angiography is a specific contrast-enhanced technique that is valuable in the assessment of intracranial and neck vessels. The most common applications are in the assessment of patients with acute stroke who are potentially eligible for thrombolysis or mechanical clot retrieval, assessment of the extracranial carotid arteries in place of Doppler ultrasound or magnetic resonance angiography, and in subarachnoid haemorrhage.
Spinal CT imaging is usually performed without contrast. This is adequate for the assessment of fractures, degenerative disease, acute disc herniation, metastatic lesions, large epidural soft tissue lesions and established infection (eg discitis, osteomyelitis). Spinal cord detail is poor on CT; this is much better assessed with MRI.
Contrast and renal dysfunction
In the past decade, a substantial amount of new data has emerged questioning the causal nature of the relationship between intravenous iodinated contrast and clinically significant acute renal dysfunction (contrast-induced nephropathy). New evidence suggests that intravenous contrast is safer than previously thought in patients with mild to moderate renal dysfunction.3
The Royal Australian and New Zealand College of Radiologists (RANZCR) recently changed its guidelines on the administration of intravenous contrast. It has lowered the estimated glomerular filtration rate (eGFR) threshold for which no special precautions are required prior to administration of intravenous contrast. The guidelines also recommend that emergency radiological examinations that require intravenous contrast administration should not be delayed in order to obtain renal function tests prior to the procedure.3 The latter includes tests such as CT angiography and perfusion in the setting of acute stroke. Despite the potentially high doses of intravenous contrast required if both tests are performed as part of an acute stroke workup, it is deemed that in the appropriate clinical setting the benefits outweigh the small risk of acute renal injury.
Case 1
A previously fit and well woman, 28 years of age, presented to her general practitioner (GP) with a one-day history of vertigo and nystagmus. The GP suspected vestibular neuronitis, but wanted to exclude a central cause. Following a phone discussion with the radiologist, the GP decided to investigate the brain with CT because MRI was not readily available.
A plain brain CT showed a 15 mm acute parenchymal haemorrhage of the left middle cerebellar peduncle (Figure 1) with no significant associated oedema or mass effect. In view of the patient’s age and the atypical location of the haemorrhage, CT angiography was performed. This showed an arteriovenous malformation that was thought to be supplied by the posterior inferior cerebellar artery and drained by the inferior vermian vein.
The patient remained stable and was transferred to the neurosurgical centre for further management.
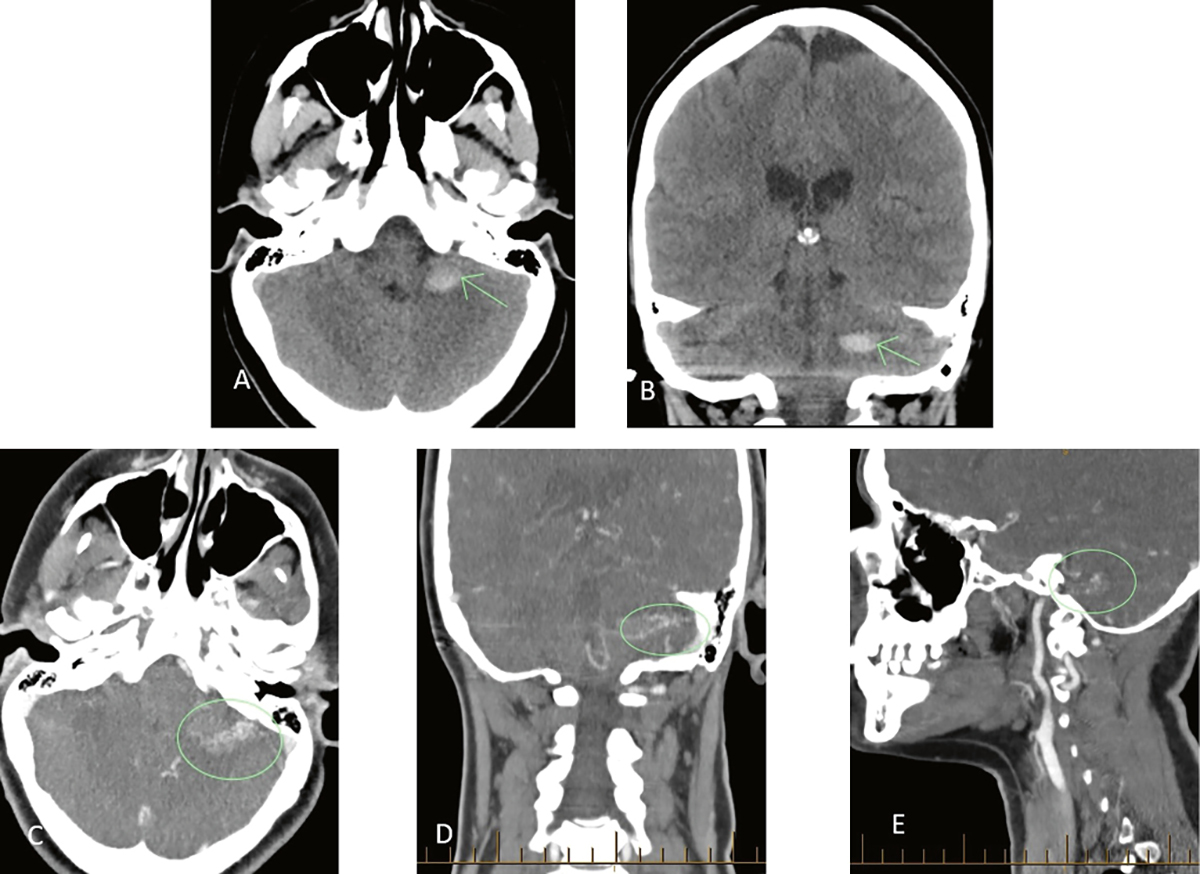
Figure 1. Plain CT brain and CT angiogram demonstrating an AVM
A, B. Axial and coronal plain CT of the brain showing an acute parenchymal haematoma of the left cerebellar peduncle
C–E. Axial, coronal and sagittal post-contrast angiography images showing the nidus of an underlying AVM
AVM, arteriovenous malformation; CT, computed tomography
Magnetic resonance imaging
Advantages and disadvantages
The main strengths of MRI are its superior soft tissue contrast and lack of ionising radiation. The images are not affected by adjacent bone structures as much as they are with CT, allowing better visualisation of the posterior fossa. MRI provides exquisite detail of the spinal cord that CT cannot approximate. Although CT is better at depicting abnormalities of cortical bone, MRI is better at assessing bone marrow. MRI also finds wider applications in functional imaging.
In contrast to CT, there are numerous available MRI sequences, each emphasising soft tissue contrast in a unique manner. However, only a limited number of sequences are acquired as part of one study. The sequences used will depend on the body part being imaged, the clinical questions/expected pathology and patient compliance.
The main drawbacks of MRI include limited availability and long acquisition time. The images are thus more prone to movement artefact. Patient claustrophobia is also a greater issue with MRI. Given the use of a strong magnet, metallic surgical implants may either be completely contraindicated or may result in artefact that degrades image quality. Great care is required in monitoring equipment and other objects taken into the scanning room as any ferromagnetic objects may become dangerous projectiles once close to the magnetic field.
A further potential disadvantage of MRI is that its higher sensitivity to pathology may result in higher rates of detecting incidental abnormalities of no clinical significance. This has the potential to generate further patient anxiety4 and unnecessary follow-up investigations. This is also an issue with CT, but to a lesser degree.
Requesting MRI
Medicare Benefits Schedule (MBS) requesting rights of GPs were expanded in 2013 to allow the request of MRI studies of the head and cervical spine (as well as of the knee) for specific clinical indications in patients aged 16 years and older. The permissible indications for head MRI are unexplained seizure(s) and chronic headache with suspected intracranial pathology. For cervical spine MRI, the indications are cervical radiculopathy and trauma.5
Cervical radiculopathy
MRI is of value when conservative treatment has failed and intervention is being considered (spinal steroid injection or surgery). Because cervical degenerative changes are common and often asymptomatic, the reliability of MRI depends on careful correlation with the clinical findings.
Trauma
In cervical trauma, CT is superior to MRI and plain radiographs in identifying cervical spine fractures and is more readily available. MRI is superior in identifying soft tissue injuries (particularly spinal cord and ligaments). However, the identified abnormalities may not all be clinically significant.
Chronic headache
MRI is indicated for persistent/atypical headache or migraine when there is a change of neurological status. In most headache syndromes, there is a lack of evidence to suggest that imaging improves health outcomes. Imaging is thus not indicated in patients with primary headache disorder6,7 (eg migraine, tension-type, cluster headaches). In a meta-analysis of multiple studies looking at imaging in patients with migraines and a normal neurological examination, the summary prevalence of significant intracranial abnormalities (eg aneurysm, arteriovenous malformation, tumour) was 0.2% with an upper 95% confidence interval (CI) limit of 0.6%.8 Potential ‘beneficial’ alleviation of anxiety from a negative scan was shown to be a non-sustained effect in one study, being present at three months but not maintained after a year.9
Seizures
MRI is the imaging modality of choice in non-urgent assessment of apparently unprovoked seizures. In emergency situations, CT is recommended because of its accessibility and speed.
Other neurological conditions
MRI is the imaging modality of choice for several other neurological conditions, including multiple sclerosis, brain and spinal cord tumours, stroke when the diagnosis is not clear on CT, and dementia.
In suspected cases of dementia, MRI and CT are equally useful in excluding other intracranial pathologies that may cause cognitive impairment (eg tumours, haematomas).10 MRI is more sensitive in detecting changes that can help with dementia subtype diagnosis (eg early subcortical vascular changes, differential regional atrophy patterns in Alzheimer’s disease, normal pressure hydrocephalus). However, this requires specialist input for appropriate correlation of clinical and radiological findings as there is often overlap in the clinical and radiological findings of the dementia subtypes. For example, normal pressure hydrocephalus is a relatively rare condition (incidence ranges from 2–20 per million per year),11 but is often overcalled on imaging studies because other conditions such as atypical Alzheimer’s disease and atypical frontotemporal dementia can mimic the radiological findings.
Case 2
A man, 40 years of age, with a history of stable pulmonary sarcoidosis, presented to his GP with a two-week history of progressively worsening headache and visual disturbance. He denied fevers, seizures and nausea/vomiting, but on examination the GP suspected papilledema. Blood tests showed moderate leucocytosis and serum C-reactive protein was also elevated. In view of the new onset nature of the headache, associated visual disturbance and suspicious fundoscopy, the patient was referred for urgent CT.
Diffuse low attenuation change in the left occipital lobe was seen on the plain CT scan. Post-contrast scans confirmed a solitary rim-enhancing lesion of the left occipital lobe with white matter oedema and mild mass effect leading to mild displacement and distortion of the occipital horn of the left lateral ventricle (Figure 2).
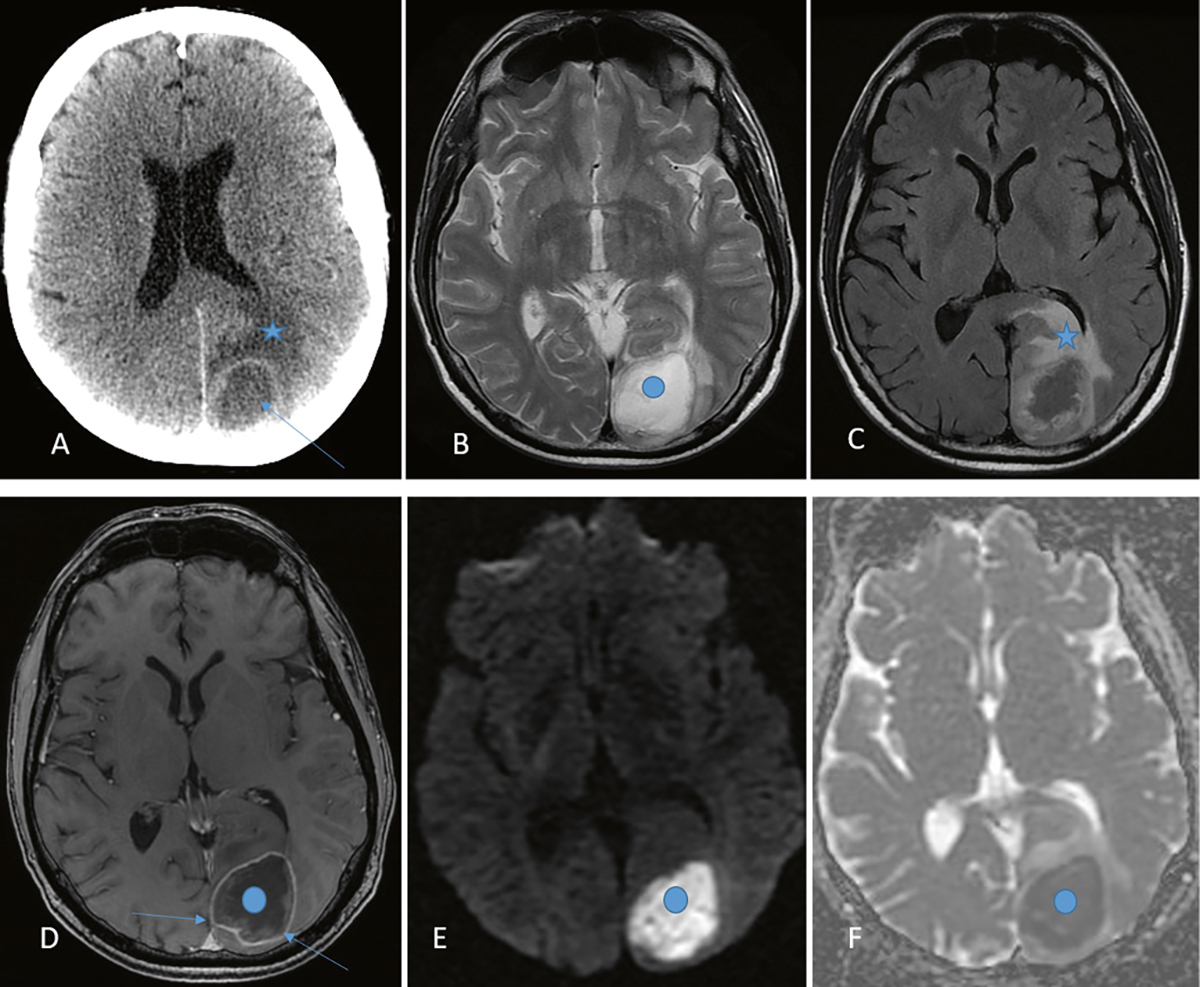
Figure 2. CT and MRI brain in cerebral abscess
A. Axial post-contrast CT brain showing a ring enhancing lesion (arrow) of the left occipital lobe and white matter oedema (star) B. Axial T2-weighted MRI sequence showing the lesion, which is hyperintense (bright) centrally (blue dot) C. Axial FLAIR MRI sequence better demonstrating the surrounding oedema (star) D. Axial T1 post-contrast MRI demonstrating rim enhancement (arrows) but no central enhancement (blue dot) E, F.Axial diffusion-weighted ADC map showing restricted diffusion in the lesion (blue dots; bright on diffusion-weighted, dark on ADC map) ADC, apparent diffusion coefficient; CT, computed tomography; FLAIR, fluidattenuated inversion recovery; MRI, magnetic resonance imaging
At this point, the main differential diagnosis of this lesion was thought to include cerebral abscess, high-grade glioma and solitary cerebral metastasis (although there was no known primary malignancy). To try to differentiate tumour from abscess, an MRI was performed. The diffusion-weighted sequence showed striking restricted diffusion throughout the centre of the lesion most compatible with an abscess in this clinical setting. The patient was urgently transferred to the neurosurgical centre for further management.
Further illustrative cases are shown of various common pathologies as seen on MRI (Figure 3) and CT (Figure 4).
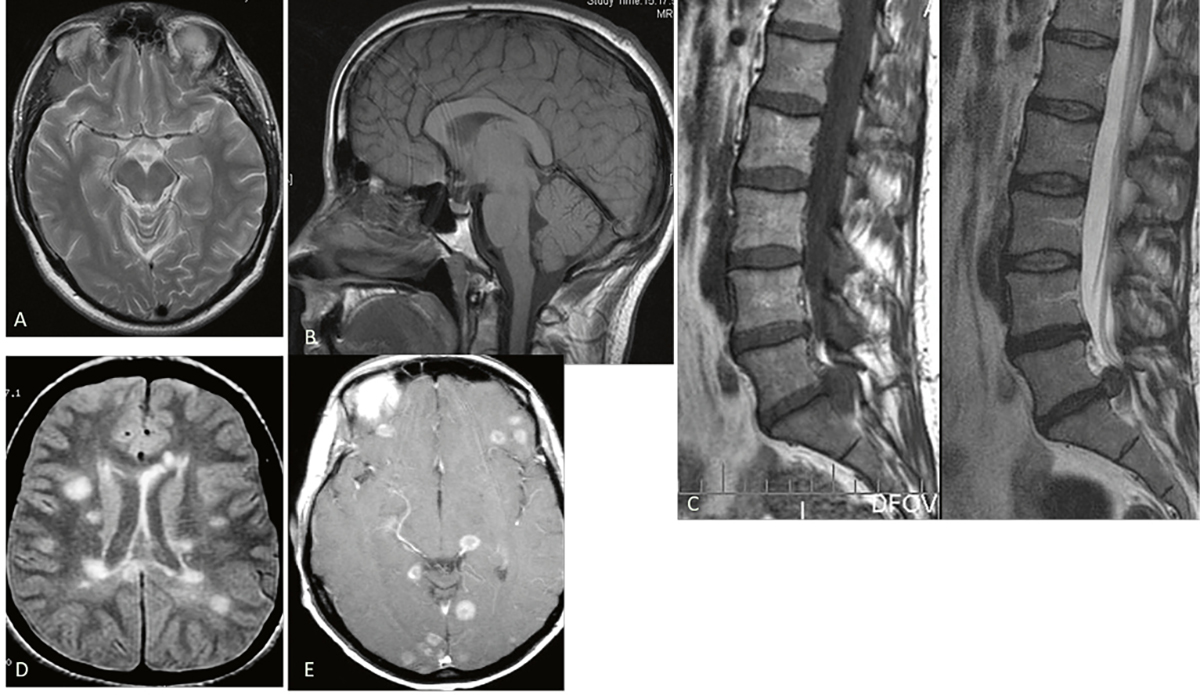
Figure 3. Various MRI images showing normal anatomy and pathology.
A. Normal brain axial T2 image
B. Normal brain sagittal T1 image
C. L5/S1 disc protrusion; sagittal T1 and T2 images
D. Multiple sclerosis, axial FLAIR image
E. Cerebral metastases axial T1 post-contrast FLAIR, fluid-attenuated inversion recovery; MRI, magnetic resonance imaging
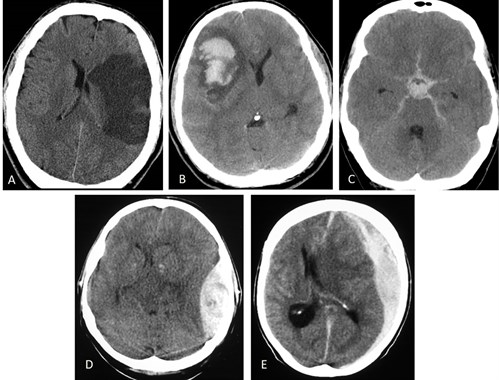
Figure 4. Various intracranial pathologies on CT
A. Established left MCA infarct
B. Intracerebral haemorrhage
C. subarachnoid haemorrhage
D. Acute left epidural haematoma
E. Acute left subdural haematoma Note brain swelling and early dilatation of temporal horns of lateral ventricles in association with subarachnoid haemorrhage and various degrees of mass effect on all other images. CT, computed tomography; MCA, middle cerebral artery
Nuclear medicine
PET is a nuclear medicine molecular imaging technique that consistently maps and quantifies the distribution of metabolic changes in the brain using various radioisotopes, most commonly 18-fluorodeoxyglucose (18FDG). It finds application in various neurological conditions, including identifying epileptogenic foci in intractable seizures and the differential diagnosis of neurodegenerative disease that cause dementia but have differing patterns of hypometabolism.12
Single photon emission computed tomography (SPECT) uses gamma ray–emitting radioisotopes incorporated into tracers that are rapidly taken up by the brain, but do not redistribute, and reflect cerebral blood flow at the time of injection. It can aid in the diagnosis and ongoing evaluation of multiple neurological conditions including (but not limited to) cerebrovascular disease, dementia, epilepsy and traumatic brain injury.
Key points
- CT and MRI are the workhorses of routine clinical neuroimaging. Given its wider availability and quicker acquisition time, CT is used more frequently in the initial evaluation of most neurological emergencies. MRI has the advantages of not using ionising radiation and providing greater soft tissue resolution.
- It is vital to include relevant clinical information on the request form to ensure the most useful images are acquired (especially important for MRI) and are interpreted appropriately. In complex cases, discussion with the radiologist prior to imaging is particularly helpful.
- Imaging is not indicated in straightforward primary headache syndromes.
Author
Julius Tamangani MBChB, FRCR, FRANZCR, Consultant Radiologist, Bendigo Healthcare, Bendigo, Vic. jtamangani@bendigohealth.org.au
Competing interests: None.
Provenance and peer review: Commissioned, externally peer reviewed.