Estimates suggest that up to one-third of Australian women experience an unintended pregnancy in their lifetime,1 making it a significant public health issue.2 Unintended pregnancy is associated with serious social, psychological and physical consequences for women, children and families. For example, studies from the US and Europe suggest that unintended pregnancy is associated with a higher incidence of adverse birth outcomes, such as risk of congenital anomalies, spontaneous abortion, premature delivery and low birth weight.3 Importantly, unintended pregnancies are not always a consequence of sex without contraception. A recent US study found that almost half of the women who experienced an unintended pregnancy reported using contraception at the time.4
Recent international and Australian research has shown that young women (aged ≤25 years) are more likely than older women to experience an unintended pregnancy.5,6 An Australian study that used data from the Understanding Fertility Management in Australia National Survey suggests that 40.8% of women aged 18–32 years experienced an unintended pregnancy. This is compared with 27.6% of women aged 33–42 years and 22% of women aged 43–51 years who reported an unintended pregnancy.1 Although the research by Rowe et al1 suggests that contraceptive misuse or failure is an important contributor to unintended pregnancy, the specific methods used by each age group are not elucidated. While these findings highlight that unintended pregnancy disproportionately affects younger women, there are little Australian data that explain the sociodemographic and reproductive predictors, and contraceptive behaviours associated with unintended pregnancy among young women in particular. This information is essential to understand the scope of the issue, and facilitate an evidence-informed discussion about unintended pregnancy and contraceptive use in Australia.
This article reports data collected from the baseline survey of the Contraceptive Use, Pregnancy Intention and Decisions (CUPID) study of young Australian women aged 18–23 years. Our aims were to:
- report on the rate of unintended pregnancy
- identify demographic, and sexual and reproductive health factors of unintended pregnancy
- examine combinations of contraceptive use at the time of first pregnancy for women who experienced an unintended pregnancy.
Method
Study overview
CUPID is a longitudinal cohort study of young women living in Australia that involved three mixed-method surveys distributed at six-monthly intervals. The recruitment process has been described in detail elsewhere.7 Briefly, it involved an innovative approach using various online, offline and networking methods. This study has been approved by the ethics committees of the University of Newcastle (approval number H-2011-0331), the University of Queensland (approval number 2011001055), Family Planning NSW (approval number R2011-05) and the Australian Government Department of Health (approval number 31/2013).
Sample
Data from the 3795 women who completed the baseline survey were analysed. Compared with the Australian Bureau of Statistics (ABS) census data, this cohort was found to be broadly demographically representative of young Australian women, with the exception of an over-representation of those with a tertiary education.7
Measures
Outcome variable
Unintended pregnancy was defined as responding ‘yes’ to a question about accidental pregnancy – ‘Have you ever become pregnant by accident?’.
Explanatory variables
Participants who reported an unintended pregnancy were asked to indicate which, if any, form of contraception they were using at the time of conception. A participant’s age at first sex and first pregnancy were reported in years; knowledge about contraception was rated on a six-point scale, ranging from ‘Excellent’ to ‘No knowledge’.
Sociodemographic variables included age (reported in years), highest educational attainment (‘high school’, ‘post-high school’), area of residence8 (‘major city’, ‘inner regional’, ‘outer regional/remote/very remote’), relationship status (‘single’, ‘partner [not living together]’, ‘cohabitating’, ‘engaged/married’) and employment status (‘working and studying’, ‘working only’, ‘studying only’, ‘not working or studying’). All sociodemographic variables were reported as at the time of completing the survey.
Statistical analyses
This analysis was conducted using baseline data only (ie the first of three mixed-method surveys). Descriptive statistics were used to:
- report the rate of unintended pregnancy
- examine contraceptive combinations at first pregnancy for participants who experienced an unintended pregnancy
- describe demographic, and sexual and reproductive health characteristics of the sample compared with participants who had never been pregnant (using chi square for categorical variables and independent samples t-test for continuous variables).
Multinomial logistic regression was used to examine unique sociodemographic predictors of contraceptive use at the first unintended pregnancy for the top five contraceptive combinations. All analyses were conducted using Stata v.13 (StataCorp LP, College Station Texas). Statistical significance was set at P <0.05.
Results
Sample characteristics
Of the 3795 women who completed the CUPID survey, 3397 (89.5%) reported ever having had sex. Of the sexually active participants, 716 (21.1%) reported having previously been pregnant or were pregnant at the time of survey completion. Of these participants, 84.6% reported being pregnant by accident. The majority reported either one (n = 420) or two (n = 131) occurrences of unintended pregnancy, while a small proportion reported three or more (9.1%). Age at first pregnancy was 12–23 years. The demographic profile of participants who had experienced a previous unintended pregnancy, compared with those who reported never being pregnant, is shown in Table 1. Briefly, women who had ever had an unintended pregnancy were slightly older (21.2 years of age ± 1.7) than those who were never pregnant (20.5 years of age ± 1.7). They were also more likely to be from outer regional/remote/very remote communities (16.7% versus 10.1%); cohabitating (34.7% versus 26.0%); engaged/married (20.1% versus 8.4%); and not employed (41.6% versus 25.6%).
Table 1. Interview schedule: key topics and questions
| |
Unintended pregnancy
(n = 606)
|
Never pregnant
(n = 2524)
|
P value
|
|---|
|
Age, years (mean [SD])
|
21.2 (1.7)
|
20.5 (1.7)
|
<0.001
|
|
Age at first sex, years [mean(SD)]†
|
15.5 (1.6)
|
16.8 (1.8)
|
<0.001
|
|
Highest education qualification
|
|
|
|
|
High school (%)
|
53.1
|
53.9
|
0.702
|
|
Post high school (%)
|
46.9
|
46.1
|
|
|
Area of residence
|
|
|
|
|
Major city
|
58.8‡
|
67.8
|
<0.001
|
|
Inner regional
|
24.3
|
21.9
|
|
|
Outer regional/remote/very remote
|
16.8‡
|
10.3‡
|
|
|
Relationship status
|
|
|
|
|
Single
|
20.6
|
23.2
|
<0.001
|
|
Partner (not living together)
|
24.3‡
|
42.2‡
|
|
|
Cohabitating
|
34.9‡
|
26.2‡
|
|
|
Engaged/married
|
20.3‡
|
8.4‡
|
|
|
Employment status
|
|
|
|
|
Working and studying
|
21.8‡
|
42.7‡
|
<0.001
|
|
Working only
|
36.6‡
|
31.7
|
|
|
Studying only
|
18.0‡
|
21.6
|
|
|
Not working or studying§
|
23.6‡
|
4.1‡
|
|
|
*As we were interested in the differences between women who reported an unintended pregnancy and those who had never been pregnant, women who reported intended pregnancy were excluded from this analysis.
†Range of age at first sex: 7–21 years of age
‡Greatest contribution to the overall chi square
§All women not working or studying as a result of being a full-time mother or on maternity leave (n = 75) had experienced an unintended pregnancy.
|
Contraceptive use at first unintended pregnancy
For participants who experienced an unintended pregnancy, the majority (73.4%) reported using some form of contraception. As shown in Figure 1, the combined oral contraceptive pill, used either alone or with another method, was the most frequently used form of contraception (39.1%). This was followed by condoms (29.4%), no contraception (26.6%) and withdrawal (used exclusively or in combination with another method; 18.5%). Few participants reported using long-acting reversible contraception when they first became pregnant (implant/rod: 1.2%; injection/needle: 1%; Mirena intrauterine device [IUD]: 0.3%; copper IUD: 0.2%).
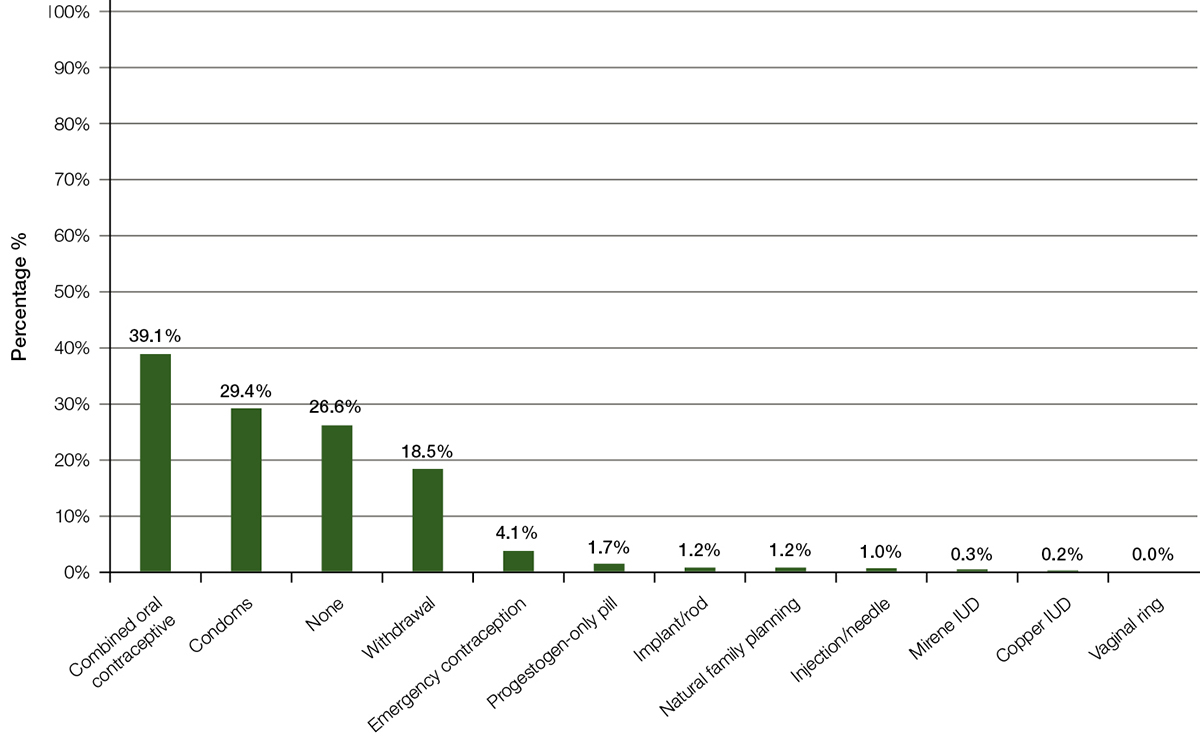
Figure 1. Specific forms of contraception used at first pregnancy for women aged 18–23 years in Australia reporting an unintended pregnancy
Participants were able to select multiple items, therefore numbers do not add to 100%.
IUD, intrauterine device
Furthermore, 31 distinct contraceptive combinations were reported. Of the participants who used contraception at the time of unintended pregnancy, 70% were using one form of contraception only. The identified contraceptive combinations (excluding emergency contraception) were then consolidated into eight major themes (Table 2). The most cited method used by the participants was the combined oral contraceptive pill (28.6%), followed by condoms (13.1%) and withdrawal (9.2%). The most common multiple contraceptive combination was the combined oral contraceptive pill with another non‑hormonal method (primarily condoms; 11.8%).
Table 2. Major combinations of contraceptive use at first pregnancy for women (n = 601) reporting an unintended pregnancy (excluding emergency contraception)
|
Contraceptive method
|
n
|
%
|
|---|
|
Oral contraceptive (combined and progestogen only)
|
172
|
28.6
|
|
None
|
161
|
26.8
|
|
Condoms
|
79
|
13.1
|
|
Withdrawal (only)
|
55
|
9.2
|
|
Oral contraceptive and other non-hormonal
|
71
|
11.8
|
|
Condoms and withdrawal
|
30
|
5.0
|
|
Long-acting reversible contraception
|
9
|
1.5
|
|
Other (includes natural family planning, long-acting reversible contraception with other method [hormonal and non-hormonal])
|
14
|
2.3
|
|
Missing
|
10
|
1.7
|
Sociodemographic predictors of contraceptive use before unintended pregnancy
The demographic, sexual and reproductive health, and health service predictors for the top five contraceptive combinations at unintended pregnancy (using no contraception as the reference) are shown in Table 3. In comparison with participants who did not use contraception, every unit increase in age (ie one year) at first sex was associated with a 27% increase in odds of using condoms at the time of unintended conception (odds ratio [OR]: 1.27; 95% confidence interval [CI]: 1.01–1.60; P: 0.041); and 50% increase in odds of using an oral contraception and a non-hormonal method combination (OR: 1.50; 95% CI: 1.18–1.91; P: 0.001). Meanwhile, every unit decrease in age (ie one year) at first pregnancy was associated with a 22% decrease in odds of using condoms (OR: 0.78; 95% CI: 0.66–0.93; P: 0.004); and an 18% decrease in odds of using an oral contraceptive and non-hormonal method combination (OR: 0.82; 95% CI: 0.69–0.98; P: 0.029) when compared with participants who did not use contraception. No other statistically significant differences were found for sociodemographics and method at unintended pregnancy.
Table 3. Association of demographic, sexual and reproductive health factors, and health service use of the top five contraceptive combinations used at unintended pregnancy among young Australian women using ‘no contraception’ as the reference (n = 538)
| |
Oral contraception only
(cf no contraception; n = 172)
|
Condoms only
(cf no contraception; n = 79)
|
Withdrawal only
(cf no contraception; n = 55)
|
Oral contraception/non-hormonal method
(cf no contraception; n = 71)
|
|---|
| |
OR
(95% CI)
|
P
|
OR
(95% CI)
|
P
|
OR
(95% CI)
|
P
|
OR
(95% CI)
|
P
|
|
Highest education
|
|
|
|
|
|
|
|
|
|
High school
|
0.72 (0.45–1.15)
|
0.169
|
1.08 (0.59–2.00)
|
0.794
|
1.05 (0.53–2.08)
|
0.880
|
0.64 (0.34–1.20)
|
0.163
|
|
Post high school (ref)
|
–
|
–
|
–
|
–
|
–
|
–
|
–
|
–
|
|
Area of residence
|
|
|
|
|
|
|
|
|
|
Major city (ref)
|
–
|
–
|
–
|
–
|
–
|
–
|
–
|
–
|
|
Inner regional
|
1.49 (0.85–2.62)
|
0.162
|
0.81 (0.39–1.71)
|
0.587
|
0.98 (0.44– 2.19)
|
0.966
|
0.63 (0.29–1.39)
|
0.254
|
|
Outer regional/remote/very remote
|
1.19 (0.63–2.25)
|
0.602
|
0.75 (0.32–1.76)
|
0.506
|
0.58 (0.20–1.70)
|
0.323
|
0.57 (0.23–1.41)
|
0.221
|
|
Relationship status
|
|
|
|
|
|
|
|
|
|
Single (ref)
|
–
|
–
|
–
|
–
|
–
|
–
|
–
|
–
|
|
Partner (not living together)
|
1.82 (0.89–3.72)
|
0.099
|
1.82 (0.74–4.47)
|
0.193
|
1.57 (0.60–4.11)
|
0.359
|
0.82 (0.34–2.01)
|
0.664
|
|
Cohabitating
|
1.32 (0.69–2.52)
|
0.407
|
1.33 (0.57–3.13)
|
0.514
|
0.72 (0.27–1.91)
|
0.514
|
0.84 (0.38–1.88)
|
0.678
|
|
Engaged or married
|
0.91 (0.43–1.91)
|
0.805
|
1.38 (0.54–3.55)
|
0.502
|
1.16 (0.43–3.14)
|
0.776
|
0.57 (0.22–1.48)
|
0.246
|
|
Employment status
|
|
|
|
|
|
|
|
|
|
Working and studying (ref)
|
–
|
–
|
–
|
–
|
–
|
–
|
–
|
–
|
|
Working only
|
0.91 (0.48–1.72)
|
0.763
|
0.74 (0.33–1.63)
|
0.453
|
0.83 (0.34–2.03)
|
0.678
|
0.60 (0.26–1.38)
|
0.229
|
|
Studying only
|
0.84 (0.38–1.86)
|
0.668
|
0.85 (0.34–2.17)
|
0.740
|
1.00 (0.34–2.91)
|
0.999
|
0.84 (0.32–2.18)
|
0.722
|
|
Not working or studying
|
0.67 (0.33–1.39)
|
0.284
|
0.40 (0.16–1.04)
|
0.061
|
0.67 (0.24–1.86)
|
0.445
|
0.63 (0.25– 1.59)
|
0.331
|
|
Consulted doctor in past six months
|
|
|
|
|
|
|
|
|
|
Yes (ref)
|
–
|
–
|
–
|
–
|
–
|
–
|
–
|
–
|
|
No
|
1.15 (0.55–2.37)
|
0.713
|
0.68 (0.23–2.01)
|
0.486
|
1.03 (0.35–3.04)
|
0.963
|
0.37 (0.10–1.36)
|
0.133
|
|
Transportation issues
|
|
|
|
|
|
|
|
|
|
Usually/always easy (ref)
|
–
|
–
|
–
|
–
|
–
|
–
|
–
|
–
|
|
Always/sometimes difficult
|
1.24 (0.61–2.53)
|
0.554
|
1.73 (0.73–4.08)
|
0.213
|
0.81 (0.25–2.59)
|
0.716
|
1.88 (0.80–4.44)
|
0.150
|
|
Age at first sex (years)
|
1.16 (0.98–1.37)
|
0.090
|
1.27 (1.01–1.60)
|
0.041
|
0.99 (0.79–1.25)
|
0.934
|
1.50 (1.18–1.91)
|
0.001
|
|
Age at first pregnancy (years)
|
1.06 (0.94–1.20)
|
0.345
|
0.78 (0.66–0.93)
|
0.004
|
1.07 (0.91–1.27)
|
0.412
|
0.82 (0.69–0.98)
|
0.029
|
|
Contraceptive knowledge
|
|
|
|
|
|
|
|
|
|
Excellent/very good (ref)
|
–
|
–
|
–
|
–
|
–
|
–
|
–
|
–
|
|
Good/fair/no knowledge
|
0.89 (0.54–1.48)
|
0.665
|
0.99 (0.52–1.89)
|
0.984
|
0.79 (0.38–1.67)
|
0.543
|
0.64 (0.32–1.27)
|
0.202
|
|
Note: multinomial regression with contraceptive combinations as the outcome (REF: no contraception; n = 161)
|
Discussion
Most participants (84.6%) who reported a previous pregnancy considered it an accident. The majority of participants (73.4%) indicated that they used some form of contraception, most commonly the combined oral contraceptive pill (39.1%), at the time of conception. Condoms were also used by those who experienced an unintended pregnancy, both alone (13.1%) and in combination with the pill (11.8%). Importantly, the study found very few sociodemographic factors that determined contraceptive use prior to an unintended pregnancy.
It is well established that user-dependent contraceptive methods (eg the pill) are characterised by larger disparities between typical and perfect use rates when compared with their non–user dependent counterparts (eg intrauterine devices).9 Additionally, user non-compliance with the pill is well described,10 as is user dissatisfaction with condoms, often leading to discontinuation of the method.11 These findings highlight the continued trend for young women to use short-term hormonal and barrier methods over more effective long-acting reversible contraception (LARC), as has also been demonstrated elsewhere.12
Interestingly, 18.5% of participants reported using the withdrawal method exclusively or in combination with another method prior to an unintended pregnancy. Withdrawal relies on the willingness and skill of the male partner, and is much less effective at preventing pregnancy than hormonal methods, particularly among young people.9 It is unclear why the participants used this method at such high rates, above and beyond significantly more effective hormonal methods.
Practising the withdrawal method may reflect cultural or religious values,13 relationship dynamics, sexual pleasure considerations,14 a lack of knowledge about other hormonal methods,15 or a convenient contraceptive choice.16,17 Additionally, using the withdrawal method may have been to avoid the side effects associated with hormonal contraceptives, given previous indications of the importance of side effects in contraceptive decision-making.18
Furthermore, despite reporting that their pregnancy was accidental, 26.6% of participants reported using no contraception prior to the unintended conception. The reasons for these responses are unclear. Potentially, participants may be illustrating ambivalent views towards conception and pregnancy. Research has found a relationship between pregnancy ambivalence and contraceptive use, where participants who report ambivalence use less effective methods19 or no contraceptive at all.20 Alternatively, these findings may reflect issues with access,21,22 or other social or relational impacts (including relationship status) on unprotected intercourse leading to unintended pregnancy.23
Contraceptive use prior to unintended pregnancy takes place within complex and varied individual, social and relationship contexts. In the clinical setting, taking the time to listen to women about their individual needs and circumstances of their life may lead to better discussions about what contraceptive method works best for them. It is also important to allow for follow-up appointments to check on acceptability of side effects and other aspects of the method. This may also increase the woman’s satisfaction with the method and lead to better effectiveness.
Given the high rate of oral contraceptive failure, ensuring women understand how to use their contraception effectively is also important. Although reducing unintended pregnancies by increasing the access that women have to LARC is an important step, it is important to ensure they are provided with knowledge and information about all available methods so they are able to make the best decision for themselves.24 Future research could investigate why young women continue to use short-term hormonal, barrier and natural methods above and beyond their more effective LARC counterparts.
Strengths and limitations
This study is the first to explore contraceptive use before unintended pregnancy as experienced by young Australian women using a large sample of participants that was demographically similar to women of the same age in the Australian population. Importantly, this allows for a greater understanding of contraceptive use at the time of unintended conception. However, it must be noted that we used non–random-sampling techniques (with a large focus on social media) to recruit the participants.7 While this method of recruitment does not allow us to produce a response rate or provide a comparison between responders and non-responders, we achieved a similar demographic profile to other cohort studies of young women using traditional sampling techniques.25
This study should also be considered in light of a few other limitations. First, we used a dichotomous measure of unintended pregnancy (‘Yes’ or ‘No’). Although this meant that we were unable to capture the complexity of unintended pregnancy, pregnancy intendedness is difficult to accurately measure.26 Our measure of pregnancy intendedness was developed on the basis of feedback from focus groups of young women.27 The measure was constructed to ensure maximum clarity and relevance for young women, an approach that is increasingly recognised as useful.1
Second, we relied on retrospective and self-reported accounts of unintended pregnancy. Research has shown that opinions towards pregnancy often change after the birth of the child.28 There may have been participants in our study who experienced an unintended pregnancy but did not consider it as such at the time of completing the survey, and vice versa. This means that the rate of unintended pregnancy in our cohort may be under-reported.
Third, we examined combinations of contraceptive use at the time of first unintended pregnancy. Hence, the intricacies associated with contraceptive use for repeated unintended pregnancies may be different. Indeed, 20% of participants reported two unintended pregnancies, and this may be an avenue for further exploration in the future.
Fourth, similar to other longitudinal health surveys29 women from lower educational backgrounds were under-represented. However, this was adjusted in the multivariate analysis.
Finally, as our primary interest was on the contraceptive practices leading to unintended pregnancy, we did not collect data on the outcome of these pregnancies. This may be an area of interest for future research.
Conclusion
Most of the participants who reported ever being pregnant considered the pregnancy to be accidental. Almost three quarters of participants were using some form of contraception at the time; generally, the pill, condoms or withdrawal method. In the clinical setting, conversations about contraception might benefit from discussing the disparities between rates of effectiveness under perfect and typical use conditions, while acknowledging the social and personal aspects of contraceptive (non-)use.
Follow-up consultations could ensure that the chosen method continues to be suitable, or provide alternative methods if it is not. All women presenting to their GP for advice about contraception should be provided with a comprehensive conversation about the available methods, and a decision about the most appropriate method made by the woman in consultation with her GP.
Authors
Jacqueline Coombe BSocSci (Hons), PhD candidate, Research Centre for Generational Health and Ageing, Faculty of Health, University of Newcastle, Callaghan, NSW. jacqueline.coombe@uon.edu.au
Melissa L Harris BA, Psych (Hons), PhD, Research Fellow, Research Centre for Generational Health and Ageing, Faculty of Health, University of Newcastle, Callaghan, NSW
Britta Wigginton BA (Hons), PhD, Lecturer, School of Public Health, University of Queensland, Herston, Qld
Jayne C Lucke BA (Hons), PhD, Director, Australian Research Centre in Sex, Health and Society, La Trobe University, Melbourne, Vic
Deborah Loxton BPsych (Hons), PhD, Co-Director, Research Centre for Generational Health and Ageing, Faculty of Health, University of Newcastle, Callaghan, NSW
Competing interests: The funding partners (Australian Research Council [ARC; Linkage Project Grant LP100200349] and industry partners Family Planning NSW and Bayer Australia Ltd) had no input into this paper and researchers worked independently from the funders. The research on which this paper is based was conducted at the universities of Queensland and Newcastle. All authors had full access to all of the data for this paper.
Jayne Lucke has received funding from the ARC and the National Health and Medical Research Council (NHMRC). She served as a director of Family Planning Queensland and was Chief Investigator on an ARC Linkage Grant that involves cash and in-kind support from Family Planning NSW and Bayer Australia. She has received personal fees and non-financial support from Merck, Sharpe & Dohme (Australia) Pty Ltd outside the submitted work. She is Director of the Australian Research Centre in Sex, Health and Society, which receives funding from diverse sources listed in the annual report (available at www.latrobe.edu.au/arcshs). Deborah Loxton has received funding from the ARC and NHMRC. She was Chief Investigator on an ARC Linkage Grant that involves cash and in-kind support from Family Planning NSW and Bayer Australia. She is Deputy Director on the Australian Longitudinal Study on Women’s Health, which is funded by the Department of Health. She is also the co-director of the Research Centre for Generational Health and Ageing at the University of Newcastle, which receives funding for research projects from diverse sources. Melissa Harris and Britta Wigginton were previously employed through an ARC Linkage Grant that involved some cash and in-kind support from Family Planning NSW and Bayer Australia. Jacqueline Coombe is supported by an Australian Postgraduate Award (APA).
Provenance and peer review: Not commissioned, externally peer reviewed.
Acknowledgements
We gratefully acknowledge funding support from the Australian Research Council (Linkage Project Grant LP100200349), and industry partners Family Planning NSW and Bayer Australia Ltd. We are grateful to the women who provided the survey data. All members of the Faculty of Health and Medicine at the University of Newcastle are affiliated with the Hunter Medical Research Institute (HMRI).