Many patients experience transient but significant emotional disturbance known as the ‘cardiac blues’1 at the time of, or soon after, an acute cardiac event. This may include acute myocardial infarction (AMI), acute coronary syndrome (ACS) and coronary artery bypass graft surgery (CABGS). Common emotions include shock, low or fluctuating mood, sadness, worry, guilt and anger.1–3 Mood change is displayed by tiredness, irritability, tearfulness, loss of pleasure in usual activities, withdrawal from others, early waking and other sleep disturbance, and changes in appetite and sex drive.1–3 Cognitive changes that typically co-occur include confusion and forgetfulness, inability to concentrate, nightmares, reduced self-esteem, concerns about role changes, particularly regarding paid work, physical health and independence, and pessimism about the future.1–3 It has been suggested that almost all patients experience at least some symptoms of emotional distress at the time of, or soon after, an acute cardiac event.1
Early distress can be considered part of the normal emotional reaction to the cardiac event, and has been described as an appropriate bereavement or adjustment response to a life-threatening incident.1,4,5 Symptoms of distress can also occur as a normal physiological reaction to the illness or to hospitalisation itself.3,6–8 It has been noted that ‘after acute cardiac illness, this distress is a normal response to loss, threat of other losses, and awareness of mortality’.1 Goble and colleagues noted that distress or depression ‘is to be expected … is not an abnormal reaction and is not an illness’ after an acute cardiac event.1 Early distress typically resolves in the first 2–3 months after the cardiac event as patients recover physically,9,10 and according to Goble ‘it subsides, as does bereavement’.1
However, one in five patients meet diagnostic criteria for major depression after a cardiac event.6,11–13 These patients are thereby at increased risk of morbidity and mortality.14,15 It has been proposed that all cardiac patients should be screened for depression around the time of their cardiac event in light of the high prevalence and prognostic importance of post-event depression.11,12 It is anticipated that routine screening will improve outcomes for patients. However, many researchers have noted this has not been empirically tested.5,7,8,16–19 One of the key problems is the risk of false positive classification of patients with transient distress, or the ‘cardiac blues’, particularly if depression screening is undertaken in hospital or during early convalescence.5,8,19
Much attention has been given to the identification and treatment of the significant minority of cardiac patients with severe clinical depression.12,20,21 However, relatively little attention has been given to assisting the vast majority of patients who experience cardiac blues during convalescence after a cardiac event. A recent study of cardiac patients’ unmet needs for support identified psychological needs as second only to health information needs.22 This highlights the importance from the patients’ perspective of psychological support.
Several studies have found that early education of symptom management and behaviour change is essential for patient recovery and improves patient outcomes if it is provided in hospital or at the time of discharge.23,24 It is possible that providing patients with information and support on what to expect emotionally might similarly improve patient outcomes. Several studies have investigated cardiac patients’ preference on the mode and timing of education on behavioural self-management.23 However, there is little or no documented evidence on whether patients want to be informed on likely emotional responses to a cardiac event, or their preferences for when and how to receive such information. The aims of the study were therefore to:
- assess whether patients want to receive information on what to expect emotionally after a cardiac event
- identify patients’ preferences regarding the timing and format for such information.
The study also sought to document the prevalence of anxiety and depression in hospital and at two and six months after the event, and the prevalence of receipt of information on emotional issues related to a cardiac event in addressing these two key aims.
Methods
Sample
Eligible patients were those consecutively admitted after an AMI or with ACS to two hospitals in Bendigo, a large provincial town in central Victoria, Australia. One is a public hospital and the other a smaller private hospital. Patients who were admitted to these hospitals after undergoing CABGS or percutaneous coronary intervention (PCI) at a metropolitan hospital were also eligible for inclusion. The two hospitals serve the Loddon Mallee, which is the largest health region in Victoria. It covers a wide rural population including Swan Hill, Kerang, Echuca, Barham, Kyneton, Castlemaine and other surrounding areas. Neither hospital had a systematic approach to the provision of written or verbal information on the emotional aspects of recovery after a cardiac event at the time of the study. All patients were admitted for their first cardiac event. Approval for the study was obtained from the Human Research Ethics Committees (HREC) of the two hospitals: Bendigo Health HREC 27/2008 and St John of God HREC 344. Full details of the study procedure appeared in an earlier publication, which investigated the trajectories of patients’ anxiety and depression scores over time.4
Procedure
Eligible patients were identified by medical or nursing staff from relevant admission books, approached by relevant clinical staff to ascertain their interest in the study, and approached by the researcher who explained the study and provided an introductory letter and consent form. All participating patients gave signed consent.
Baseline assessment in hospital
Sociodemographic information was collected during baseline interview at the hospital. This included age, gender, marital status, country of birth, employment status, current or last occupation, living arrangements, home ownership and private health cover. History of depression and anxiety were assessed by asking ‘Have you ever been depressed in the past, prior to your cardiac event?’ and ‘Have you ever experienced other mood difficulties such as anxiety?’ The 14-item Hospital Anxiety and Depression Scale (HADS)25 was used to assess anxiety (HADS-A) and depression (HADS-D) in hospital and at two months. The HADS has been shown to be psychometrically sound for use in cardiac populations.26 The generic cut-offs for mild-to-moderate symptoms are HADS-A ≥8 for anxiety and HADS-D ≥8 for depression.27 The optimal cut-offs for screening for mild to major anxiety and depression in cardiac patients are HADS-A ≥6 for anxiety and HADS-D ≥4 for depression.28 The lower cut-offs are particularly relevant for cardiac patients whose symptoms may not appear until later during the convalescent period. The lower cut-offs were identified in a cardiac sample (n = 206 patients with myocardial infarction) on the basis of the optimal sensitivity and specificity when compared with a gold standard clinical interview.28 Data for generic and cardiac-specific cut-offs are presented as an indication of levels of patient distress in the absence of a measure of the cardiac blues.
Collection of medical and clinical data
Medical and clinical data were collected at baseline from the coronary care or medical unit records. These included admission event (AMI, ACS, PCI, CABGS), history of hypertension, history of hypercholesterolaemia, family history of cardiovascular disease, diabetes mellitus and other significant comorbidities.
Admission clinical parameters and risk factors collected included current weight and height (for body mass index), waist girth, systolic and diastolic blood pressure, total cholesterol, high density lipoprotein (HDL) cholesterol, low density lipoprotein (LDL) cholesterol and smoking status. All risk factor data were coded according to the National Heart Foundation’s Guidelines for secondary prevention of heart disease.29
Follow-up questionnaires at two and six months
Patients completed a follow-up questionnaire at two and six months post-discharge. All constructs included in the baseline interview were reassessed at follow-up. Additional questions in the six-month interview explored patients’ experiences and preferences regarding the receipt of information on common emotional responses to an acute cardiac event. Patients were asked if they would have liked to have received information on the possible emotional responses following a cardiac event. Patients were given a list of possible formats and times for receiving the information. They were asked to indicate acceptable formats, times and, more specifically, their most preferred information format and time. Patients were also asked whether they received any information on what to expect emotionally after a cardiac event. The format and timing of these information were also assessed.
Data analysis
Frequencies were calculated to identify the proportion of patients with anxiety and depression when they were in hospital, and during the two-month and six-month interval. This was done using generic and cardiac-specific cut-offs. Frequencies were also calculated for each item relating to information receipt and preferences. Chi-square statistic was used to determine whether information desire and receipt were related to one another, and to anxiety and/or depression in hospital and at follow-up.
Results
Study sample
There were 219 eligible patients. However, 59 (27%) were excluded because of an acute medical condition or concurrent physical impairment (n = 24), unavailability for interview in hospital prior to transfer or discharge (n = 23), unavailability for follow-up interview (n = 2) and refusal to participate (n = 10). Therefore, 160 (73%) patients completed the baseline interview in hospital. Two-thirds (66%) were from the public hospital and one-third (34%) from the private hospital. Half (50%) of the patients were admitted following an AMI and one-third (30%) with a diagnosis of ACS. The remainder had undergone either PCI (12%) or CABGS (8%). One hundred and forty-two (89%) out of the 160 included at baseline were re-interviewed at two months and 140 (88%) at six months. Thirteen (8%) patients died over the course of the study after participating in the baseline interview.
Patient characteristics
The study sample was described in detail elsewhere.4 Most patients were male, born in Australia, and were married or in a de facto relationship. Their ages ranged from 40 to 96 years, with a mean (SD) age of 67.6 (11.5) years and median of 68 years. Sociodemographic and clinical characteristics are illustrated in Table 1.
Table 1. Profile of the sample
|
|
Variable
|
n
|
%
|
|---|
|
Sociodemographic characteristics
|
|
Male gender
|
109
|
68
|
|
Married/de facto
|
108
|
67
|
|
Born in Australia
|
140
|
87
|
|
In workforce
|
52
|
33
|
|
Manual occupation
|
28
|
19
|
|
Private health cover
|
62
|
39
|
|
Home owner
|
101
|
63
|
|
Medical history
|
|
History of hypertension
|
116
|
73
|
|
History of hypercholesterolaemia
|
96
|
60
|
|
Positive family history of cardiovascular disease
|
104
|
65
|
|
Diagnosed diabetes mellitus
|
43
|
27
|
|
Significant comorbidity
|
119
|
74
|
|
Psychological history
|
|
History of depression
|
59
|
37
|
|
History of anxiety
|
43
|
27
|
|
CVD risk factors in hospital
|
|
Obese (BMI >30)
|
47
|
29
|
|
Above waist girth target (n = 50)
|
36
|
72
|
|
High systolic blood pressure (≥130)
|
97
|
61
|
|
High diastolic blood pressure (≥80)
|
56
|
35
|
|
High total cholesterol (≥4) (n = 108)
|
73
|
68
|
|
Low HDL cholesterol (<1) (n = 96)
|
55
|
57
|
|
Current smoker
|
26
|
16
|
|
Comorbidities were most commonly chronic illnesses including respiratory conditions (asthma and chronic obstructive pulmonary disease), heart failure and other vascular conditions, renal failure, osteoarthritis and rheumatoid arthritis and, less commonly, cancer. Risk factor targets are defined based on National Heart Foundation of Australia Guidelines.29
|
Anxiety, depression and distress in hospital and at two months post-event
The poportions of patients classified as anxious and depressed in hospital and two months post-event are shown in Table 2.
More than one-third of patients (36%) in hospital were classified as anxious and around one-fifth (18%) as depressed using the generic cut-offs (HADS-A ≥8; HADS-D ≥8 respectively).27 More than half (54%) were classified as anxious and half (50%) as depressed using the cardiac-specific recommendations (HADS-A ≥6; HADS-D ≥4).28 Almost three-quarters (72%) of participants had some symptoms of anxiety or depression (HADS-A ≥6 and/or HADS-D ≥4) in hospital. These prevalence rates had reduced by 30–50% by the two-month and six-month follow-up. However, half the patients (49%) still had some symptoms of either anxiety or depression during the follow-ups.
Table 2. Proportion of patients classified as anxious and/or depressed in hospital and at two months
|
|
|
|
In hospital
(n = 160)
|
Two months
(n = 142)
|
|---|
|
|
|
n
|
%
|
n
|
%
|
|
Cardiac-specific cut-offs
|
Anxious or depressed
|
115
|
71.9
|
69
|
48.6
|
|
Anxious
|
87
|
54.4
|
46
|
32.4
|
|
Depressed
|
80
|
50.0
|
47
|
33.1
|
|
Anxious and depressed
|
52
|
32.5
|
24
|
16.9
|
|
Generic cut-offs
|
Anxious or depressed
|
64
|
40.0
|
32
|
22.5
|
|
Anxious
|
57
|
35.6
|
26
|
18.3
|
|
Depressed
|
29
|
18.1
|
17
|
12.0
|
|
Anxious and depressed
|
22
|
13.8
|
11
|
7.7
|
|
Note, anxiety and depression defined using the Hospital Anxiety and Depression Scale (HADS); cardiac-specific cut-offs: HADS-A ≥6; HADS-D ≥4;28 generic cut-offs: HADS-A ≥8; HADS-D ≥827
|
Experiences of and preferences for receipt of information about emotional adjustment
Receipt of information
Most patients did not receive (n = 79/140; 56%) or could not recall receiving (n = 26; 19%) any information on what to expect emotionally after a cardiac event. Only 35 (25%) patients had received such information, 12 (10%) at discharge and the remainder at a later stage. Most who received it got it verbally from a health professional (n = 18) or via pamphlet (n = 15). Few received it via phone (n = 7), book (n = 3), CD (n = 2) or DVD (n = 1).
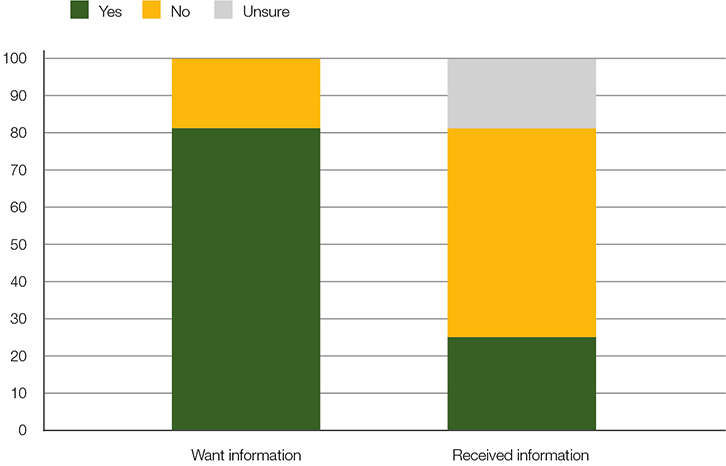 |
| Figure 1. Proportion of patients who wanted and received information on what to expect emotionally |
Desire for information
The majority of patients (114 out of 140; 81.5%) indicated they would have liked to receive information on what to expect emotionally. Most wanted this information at the time of discharge from hospital (n = 80; 70%) or immediately after discharge (n = 25; 22%). Others wanted it arouvnd two months post-event (n = 19; 16%). Nine patients (8%) indicated two of these time points. Acceptable formats included pamphlet (n = 98; 86%) and/or verbally from a health professional (n = 85; 75%). Fewer patients endorsed the formats of a telephone call (n = 43; 38%), book (n = 17; 15%), DVD (n = 16; 14%) or CD (n = 14; 12%). The formats that were most preferred were verbally from a health professional (n = 64; 57%) and a pamphlet (n = 33; 29%). Eleven (10%) patients nominated pamphlet and verbal information despite being instructed to only select one preference. The three options accounted for 96% of the preference votes by the participants. Proportions for acceptable and preferred formats are illustrated in Figure 2.
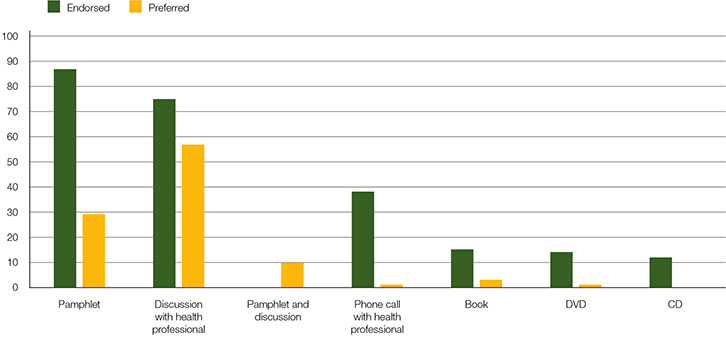 |
Figure 2. Endorsed and most preferred format for information about what to expect emotionally
Note, ‘pamphlet and discussion combined’ was not listed in the original list of options to be ‘endorsed’, hence data only available for ‘preferred’ |
Association between information desire, receipt and anxiety/depression
There was a significant association between wanting and receiving information (ⅹ2 = 7.62, df = 1, P = 0.006). This was largely due to the fact that all but one (96.2%) of the 26 patients who did not want information, did not receive it. However, of the 114 patients who wanted information, the majority (70.2%) did not receive it. Only 29.8% of those who wanted information received it. Neither wanting nor receiving information was significantly related to anxiety/depression either in hospital (ⅹ2 = 0.002, df = 1, P = 0.965; ⅹ2 = 0.003, df = 1, P = 0.953 respectively), at 2 months (ⅹ2 = 0.672, df = 1, P = 0.412; ⅹ2 = 0.226, df = 1, P = 0.635) or at 6 months (ⅹ2 = 0.502, df = 1, P = 0.479; ⅹ2 = 1.373, df = 1, P = 0.241).
Discussion
The present findings highlight a strong desire from patients to be informed on what to expect emotionally after a cardiac event, namely information on the cardiac blues. Almost all the patients in this study wanted this information to be provided in written form as a brochure, in verbal form from a health professional or a combination of the two formats. Most wanted this information at the time of hospital discharge or shortly after. It is important to note that even those who did not experience distress wanted to be informed about the cardiac blues.
Around one-third of patients received any information on the emotional aspects of having a cardiac event, and only 10% received this information at their preferred time (on discharge from hospital). Having received information was not related to the presence of symptoms. The majority of those who did not receive information actually wanted it.
These findings support previous work that found a desire among cardiac patients for education and support more generally.30,31 The combination of written and verbal support in particular has been shown in a randomised controlled trial to reduce anxiety and depression in patients with myocardial infarction.32 A systematic review of the approaches to CABG patient education concluded that a combination of methods resulted in superior improvements when compared with single approaches alone.33 Several authors have emphasised the importance of early education in hospital or during discharge.23,24
The rate of in-hospital distress was high. Almost three-quarters of patients had some symptoms of anxiety or depression in hospital. This was based on combined scores using cardiac-specific cut-offs for the two HADS subscales. Almost half had some symptoms at two and six months after the event. This high prevalence of symptoms underscores the need for all patients to be informed about the possibility of emotional disturbance at the time, or soon after, the cardiac event. Satisfaction with discharge education has been found to reduce psychological distress later.30 This further supports the importance of providing appropriate and comprehensive information at that time.
Early emotional issues resolve for many patients.10,34 Those who present with early symptoms can therefore be reassured that symptoms of cardiac blues are likely to be transient and can be considered part of a ‘normal adjustment response’. Normalising common emotional reactions to a cardiac event as cardiac blues may enhance recovery and warrants empirical investigation. The symptoms commonly experienced by patients after the event (eg low or fluctuating mood, tearfulness, loss of pleasure in usual activities, sleep disturbance, reduced self-esteem, changes in appetite and sex drive, concerns about role changes, and worries about the future)1,2 are typical of a normal grief response to an experience of loss or trauma.1 ‘Prevention and management depend on the patient’s learning that a depressed mood is a normal temporary response to the illness … and that recovery is the rule’.1
However, cardiac patients also need to know that depression is possible after a cardiac event. One in five patients will go on to experience serious depression after a cardiac event,6,11–13 and are thereby at increased morbidity and mortality risk.14,15 Around one-fifth of patients in the present study were above threshold for depression in hospital (using the generic cut-off), but this rate had almost halved after two months. This is consistent with previous studies. Patients can be alerted to seek help if they have ongoing symptoms of distress if they were informed of the possibility of depression. Informing patients in this way might help to ensure early presentation for assessment and treatment, which should further improve patient outcomes. Appropriate and efficacious treatments for depression in cardiac patients include cognitive behaviour therapy, exercise, selective serotonin reuptake inhibitors (SSRIs) and collaborative care.12 Some authors have identified specific risk factors or ‘red flags’ to alert patients and health professionals to an increased risk of depression.4 Informing patients and health professionals of red flags might also increase help-seeking behaviour when appropriate, which may lead to improved patient outcomes. Again, this aspect of information provision warrants empirical investigation. Importantly, several studies have shown that health professionals need education on the identification and management of anxiety and depression in the cardiac setting.21,35
The present study has some limitations that should be noted. First, we used HADS to identify patients with symptoms of anxiety and/or depression. This has recently received criticism for its unclear factor structure.36 However, two recent systematic reviews concluded that HADS is an effective tool in identifying ‘emotional distress’,36,37 hence its suitability in the present study. Second, the findings are based on a relatively small sample that included patients from regional and rural Victoria. Therefore, it may not be generalisable to those residing in metropolitan areas. However, the patient sample is typical of cardiac samples in all other settings, which supports the relevance of the findings. Third, it was not possible to verify patients’ reports of the information they received on emotional recovery. We only had access to patients’ records during their hospital stay, not at the two-month and 6six-month follow-up. It is likely that reports of low receipt of information are accurate given neither participating hospital had a systematic approach to disseminating information on the emotional aspects of recovery. We found no evidence of the systematic provision of information of this kind (unpublished data) in a subsequent consultation with 19 hospitals in metropolitan Melbourne and regional areas of Victoria.
The present findings point to the need for a systematic approach to informing cardiac patients on the likelihood of cardiac blues. This could be done in hospital during admission for an acute event, at the time of hospital discharge and in various post-event settings (eg cardiac rehabilitation, hospital outpatient clinics and general practice). Along with the need for appropriate patient resources, health professional training may be required to support translation of these findings into clinical practice, given that many patients want advice from a health professional. Future studies could investigate the impact of providing this information to patients, particularly in terms of impact on patients’ understanding of their symptoms and presentation for early assessment and treatment, if required.
Authors
Barbara M Murphy PhD, Director of Research, Heart Research Centre, Melbourne, VIC; Department of Psychology, University of Melbourne, VIC; School of Medicine & Public Health, University of Newcastle, NSW. barbara.murphy@heartresearchcentre.org
Rosemary O Higgins DPsych, Senior Research Fellow, Heart Research Centre, Melbourne, VIC; Department of Physiotherapy, University of Melbourne, VIC; School of Psychology, Deakin University, VIC
Alun C Jackson PhD, Director, Heart Research Centre, Melbourne, VIC; Centre on Behavioural Health, University of Hong Kong, PRC
John Edington MB, ChB, FFA (SA), FANZCA, Director of Anaesthesia, Bendigo Health, Bendigo, VIC
Anthony Jackson BSc (Hons), MBBS, FRACP, Director of Cardiology, St John of God Hospital, Bendigo, VIC
Marian U Worcester PhD, Senior Research Fellow, Department of Epidemiology and Preventive Medicine, Monash University, VIC
Competing interests: Murphy, Judd, Humphreys, Edington and Anthony Jackson received a grant in relation to this work from Victorian beyondblue Centre of Excellence.
Provenance and peer review: Not commissioned, externally peer reviewed.
Acknowledgements
We thank Ms Deborah Ludeman, Ms Susan Crebbin and Mr Michael Le Grande from the Heart Research Centre who were involved in data collection and management for this study. Thank you also to Professor John Humphreys, Department of Rural Health, Monash University Bendigo, and Professor Fiona Judd, Department of Psychiatry, University of Melbourne for their contributions as investigators on the original study. Thank you also to the patients and staff from Bendigo Health and St John of God Hospital, Bendigo, who participated in this study. This study was made possible through a grant from the beyondblue Victorian Centre of Excellence (bbVCoE).