Case
A male temporary resident of Korean descent, 31 years of age, was referred by a general practitioner (GP) to a metropolitan hospital with a four-week history of cough, lethargy, febrile illness and generalised arthralgia. He had an outpatient chest radiograph, which revealed a large left-sided pleural effusion with an ill-defined right mid-zone density suspicious for a Ghon focus (Figure 1). The patient reported no infectious contacts or a history of tuberculosis (TB) or immunosuppression. Observations were within normal parameters on presentation. Clinical examination revealed dullness to percussion of the left middle and lower lung zones, with decreased breath sounds. His inflammatory markers were 9 x 109/L for white cell count and 159 mg/L for C-reactive protein.
The patient was admitted for investigation and commenced intravenous antibiotics for possible pneumonia with an associated parapneumonic effusion.
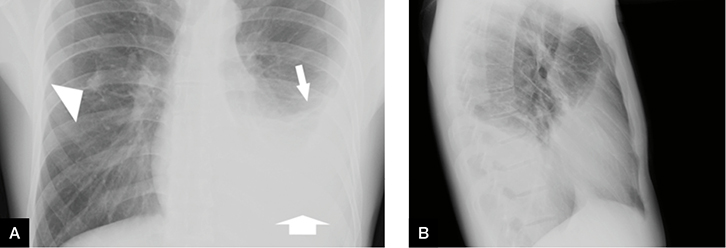 |
Figure 1. Initial chest X-ray
A. Anteroposterior view; B. lateral view revealing a left-sided pleural effusion with an ill-defined right midzone density (arrowhead). Pleural effusions on chest radiograph present as a homogenous opacification with obliteration of the costophrenic angle, a curved upper border (narrow arrow) and loss of silhouette of the identifiable diaphragm (wide arrow) |
Question 1
What initial steps can be undertaken to identify the aetiology of this patient’s unilateral pleural effusion?
Question 2
When should a patient be referred for specialist review? What investigations should be performed prior to referral?
Question 3
What are the pulmonary complications of rheumatoid arthritis?
Table 1. Causes of pleural effusion
by incidence10
| |
|
|
Cause
|
Incidence
|
|---|
|
Malignancy
|
27%
|
|
Heart Failure
|
20%
|
|
Pneumonia
|
18%
|
|
Tuberculosis
|
9%
|
|
Post-abdominal surgery
|
4%
|
|
Pericardial effusion
|
4%
|
|
Hepatic hydrothorax
|
3%
|
|
Idiopathic
|
3%
|
|
Trauma
|
2.5%
|
|
Pulmonary embolism
|
1.6%
|
|
Post-heart surgery
|
1%
|
|
Connective tissue disease
|
0.9%
|
Answer 1
Transudative effusions can often be identified on clinical assessment alone, especially with a history of cardiac, renal or liver impairment.1 These effusions are usually bilateral, but mild-to-moderate unilateral effusions can occur.2 A unilateral effusion associated with a history of pneumonia and febrile illness supports a diagnosis of parapneumonic effusion. Old age, weight loss, a history of smoking and malignancy can be indicative of a malignant pleural effusion.3 A patient’s drug history and occupational dust exposure (eg asbestos) are also relevant.4 A clinical history and physical examination can help identify the aetiology of a pleural effusion. However, distinction can only be established by pleural fluid examination.5
Dullness to percussion and tactile fremitus are the most useful clinical examination signs for a pleural effusion.2 Other examination findings may include asymmetrical chest expansion, diminished or absent breath sounds and friction rubs.2
Answer 2
Referral to a respiratory physician is indicated in the presence of a suspected unilateral exudative pleural effusion or a unilateral transudative effusion that respond poorly to treatment.4 Other red flag indicators include lung or pleural masses on imaging, sepsis associated with effusion, and the abrupt onset of symptoms, in the context of known emphysema or trauma.6
Blood tests including a full blood count, electrolytes, liver function tests, C-reactive protein and coagulation profile are recommended.6 Coagulopathy or thrombocytopaenia should be communicated on referral of the patient for specialist review.5
Pleural effusions on chest radiographs classically present as a homogenous opacification with obliteration of the costophrenic angle, a curved upper border and loss of silhouette of the identifiable diaphragm.3 Intense pleural inflammatory processes, including parapneumonic effusions and TB, can result in the development of loculations within contiguous pleural surfaces. These are identified on ultrasonography with greater sensitivity.4
An intercostal catheter was inserted into the patient under ultrasound guidance utilising Seldinger’s technique, evacuating a yellow-orange, turbid fluid. Fluid biochemistry analysis confirmed an exudative effusion, negative for acid-fast bacilli (AFB) and TB polymerase chain reaction (PCR). Antimicrobial therapy was rationalised to piperacillin and tazobactam for a possible evolving parapneumonic effusion in the context of a persistent low-grade fever.
A chest computed tomography (CT) scan revealed a residual left-sided effusion with pleural thickening and sub-pleural consolidation suggestive of chronicity. Bronchoscopy revealed inflamed bronchial mucosa with induced sputum, bronchial washings and post-bronchoscopy sputum negative for AFB and TB PCR. Thickening of the visceral and parietal pleura was observed on video-assisted thoracoscopy, and surgical biopsy revealed non-specific chronic pleuritis.
The patient reported progressively worsening arthralgia with bilateral knee joint effusions throughout his admission. Knee joint arthrocentesis revealed an inflammatory effusion, but was negative for TB PCR and crystals. Immunological markers were found to be 125 IU/L for rheumatoid factor and 432 IU/mL for anti-cyclic citrullinated peptide. The evolution of the patient’s arthritic presentation, together with the immunological markers and histological findings, affirmed the diagnosis of rheumatoid pleuritis.
Answer 3
Rheumatoid pleural effusion is an uncommon complication of rheumatoid arthritis (RA) and is found in 2–5% of patients.7,8 It frequently occurs during periods of active arthritis and in patients with subcutaneous nodules. However, a small number of patients develop effusions before, or simultaneously with, the onset of arthritic symptoms.7,8 Other components of the pulmonary anatomy can be directly affected by RA, including the airways (eg bronchiectasis, bronchiolitis), vasculature (eg pulmonary hypertension, vasculitis) or parenchyma (eg rheumatoid nodules, interstitial lung disease).9
This case report presents an uncommon initial presentation of rheumatoid pleuritis prior to the onset of RA joint symptoms. Clinical diagnosis can be achieved by the examination of the pleural fluid, together with pleural histology, immunological blood tests, clinical symptoms and signs. In regards to this case presentation, the use immunosuppressive therapies must be carefully considered given the risk of TB re-activation in the context of a suspected Ghon focus. The patient returned to Korea for ongoing management due to the cost of medical care.
Key points
- Referral to a respiratory physician is indicated in the presence of a suspected unilateral exudative pleural effusion or a unilateral transudative effusion that respond poorly to treatment.
- Rheumatoid pleuritis is a rare initial clinical manifestation of rheumatoid arthritis and can precede joint presentation.
- Any of the components of the pulmonary anatomy can be directly affected by rheumatoid arthritis, including the airways, vasculature, pleura or parenchyma.
Authors
Yogeesan Sivakumaran MBBS (Hons), Senior Resident Medical Officer, Concord Repatriation General Hospital, Concord, Sydney, NSW. yogeesan.sivakumaran@gmail.com
Alice Macdonald Cottee MBBS (Hons) BMedSci (Hons), Respiratory Medicine Advanced Trainee, Department of Respiratory and Sleep Medicine, Concord Repatriation General Hospital, Concord, Sydney, NSW
Soo Wei Foo MBBS (Hons), DM, FRACP, Visiting Medical Officer, Department of Respiratory and Sleep Medicine, Concord Repatriation General Hospital, Concord, Sydney, NSW
Competing interests: None.
Provenance and peer review: Not commissioned, externally peer reviewed.