Wheeze is a common presentation in young children. About 20% of infants wheeze in infancy and at least 40% of children <6 years of age have at least one wheezing episode.1,2 The presentation of wheeze can be a diagnostic and therapeutic challenge, as differential diagnoses are many and diagnostic tools are few. The medical literature can also be difficult to negotiate as wheezing syndromes are given myriad labels. In asthma alone these include viral wheezing, pre-school wheeze, episodic viral wheeze and multiple trigger wheeze. These labels exist in an attempt to identify phenotypic groups that may benefit from a different treatment approach. However, in clinical practice, few children sit neatly under a single diagnostic label; most occupy a spectrum with symptoms of varying severity.3 This is illustrated in the following case.
Case
A child aged 2 years with a history of wheeze since birth that seemed to have improved by 1 year of age, now presents with a 6-month history (corresponding with colder months) of repeated episodes of wheeze, especially when active. The child’s mother had observed a regular wet cough and sporadic coryzal symptoms over this time, but is unsure of their exact duration. History includes current eczema and a family history of asthma and allergies. The child is happy and thriving, and has a wet-sounding cough in clinic but no audible wheeze or respiratory distress on examination.
In this case, the history of wheeze from birth suggests the possibility of tracheomalacia or bronchomalacia. The family history of asthma/atopy and wheezing when active raises the possibility of early asthma; however, sporadic coryzal symptoms also raises suspicion of intercurrent viral lower respiratory tract infections (LRTIs) and moist cough for months is suggestive of protracted bacterial bronchitis.
Without a clear diagnostic label there is no single correct treatment approach and a diagnosis may become more certain depending on the treatment response. The algorithm shown in Figure 1 considers the most common primary presentations with wheeze and gives one possible approach to this problem. A brief summary of the major wheezing conditions is provided in Table 1.
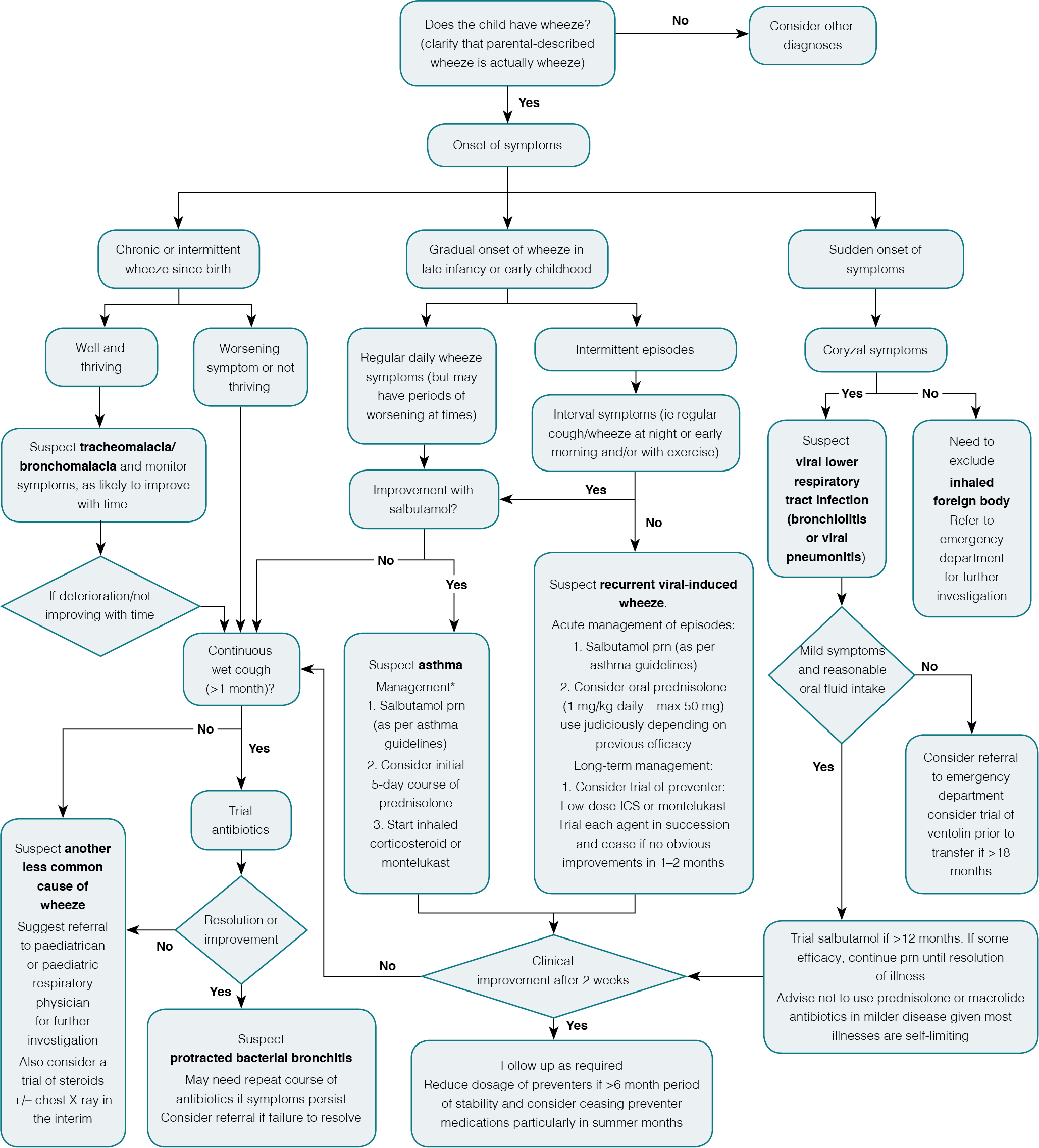 |
Figure 1. Algorithmic approach to young children presenting with wheeze in primary care
*Therapeutic benefit from asthma medications is poor for those 1-2 years of age and usually absent in the first year; ICS, inhaled corticosteroids |
Table 1. Summary of the most common wheezing conditions in young children
|
|
Condition
|
Estimated incidence in children
|
Clinical signs
|
Investigation
|
Expected clinical course
|
Management
|
|---|
|
Viral wheezing (these include a spectrum of viral LRTIs that are not always clearly separated eg viral LRTI/recurrent viral-induced wheeze/bronchiolitis – management of episodes is identical and the distinction is sometimes arbitrary)
|
Very common, especially in the first 2 years of life
50% of children will have at least one wheezing episode17
|
Wheeze associated with respiratory tract infections
May be singular or recurrent
Bronchiolitis (usually in children <2 years) manifests with fine crackles +/– wheeze on auscultation
|
No specific investigations
Nasal samples sent for virology usually do not change clinical management but isolation of RSV in infants is highly suggestive of bronchiolitis
|
60% will outgrow wheeze by 6 years
A further 15% acquire wheezing after 6 years
After 7–8 years, only 1 in 5 will outgrow it
|
Trial salbutamol if >1 year of age and continue only if effective
Supportive care involving monitoring adequate fluid intake (>50% of usual intake) and for signs of increasing respiratory distress
|
|
Asthma
|
15–20 % of the paediatric population32
|
Wheeze on a regular basis
Some will have persistent/interval symptoms between episodes of viral wheeze (cough and/or wheeze at night or with exercise)
|
Spirometry with bronchodilator response may be possible in children ≥5 years of age in experienced laboratories
|
Usually expected to be lifelong but clinical courses can vary widely between individuals
|
Exacerbations:
Regular salbutamol (as per asthma guidelines) and consider oral prednisolone for up to 5 days
Regular preventer usually indicated
|
|
Airways malacia (airways floppiness): either tracheomalacia or bronchomalacia
|
1 in 210033
|
Usually present soon after the neonatal period with wheeze, stridor, cough and rattling; children are usually well and often labelled as ‘happy wheezers’
|
Bronchoscopy usually diagnostic but not necessary in most cases
|
Majority outgrow it by age 2 years
Secondary PBB can occur, presumably from poor cough clearance
|
Treatment rarely required
If there are worsening symptoms or failure to thrive, specialist referral is indicated
|
|
Protracted bacterial bronchitis (PBB)
|
Probably common, but exact incidence unknown
|
Chronic wet cough (typically >4 weeks). Concurrent wheeze and/or rattly breathing is common
|
Bronchoscopy may assist diagnosis, but usually unnecessary
Radiological findings usually normal or non-specific
|
Majority resolve with 1–2 courses of antibiotics
|
2–6 week course of antibiotics:
commonly amoxicillin/clavulanic acid (approximately 20 mg/kg/dose twice daily)
|
Does the child actually have wheeze? How accurate is the parent’s description?
In a child who has intermittent symptoms and is asymptomatic at the time of examination, the diagnosis of wheeze is often entirely dependent on accurate parental description. Parental recognition of wheeze can differ from medically defined wheeze. In questionnaire surveys in European populations, wheeze was only correctly identified by parents 83.5% of the time4 and in rural populations 34% had never heard of the term.5 In a UK population, one-third of parents who believed their infant had wheeze changed their minds after being shown video recordings of wheeze.6
Wheeze from the lower airways is a predominantly expiratory sound. Furthermore, it is often described as a ‘musical sound’ or ‘polyphonic ‘ in nature because of the smaller airways resonating at different pitches as a result of their different sizes and variable degrees of obstruction. Given the difficulty in describing wheeze, sometimes the only pragmatic way of getting a clear idea is for the clinician to attempt to vocally reproduce the sound. With the widespread use of smart phones, the easiest course of action has become to ask the parents to make an audio or video recording. An audio guide to breath sounds can be found on the 3M Stethoscopes website (http://solutions.3m.com/ wps/ portal/ 3M/ en_EU/ 3M-Littmann-EMEA/ stethoscope/ littmann-learning-institute/ heart-lung-sounds/ lung-sounds/ #wheeze-expiratory).
Do antibiotics have a role? The emergence of protracted bacterial bronchitis (PBB)
Prescribing antibiotics for cough and other viral symptoms has declined recently, possibly because of concerns about antibiotic-resistant bacteria. This has been a necessary shift but a consequence has been the re-emergence of a small group of children who present with chronic wet cough, who have been largely ignored in the literature until the last 10 years. These children would have been described previously as having chronic bronchitis but this has been re-labelled as persistent or protracted bacterial bronchitis (PBB)7 to separate this from adult conditions. Evidence suggests that PBB may be a common enough condition7,8 to warrant its inclusion in national and international cough guidelines.9,10
The hallmarks of PBB are a prolonged moist or productive cough that lasts >4 weeks and a response to antibiotics.11 If left untreated, children with PBB continue to have wet cough for months or years. Wheeze is documented in 50–75% of these children8,11 and the diagnosis has a high degree of overlap with other wheezing conditions including asthma,8 tracheomalacia and bronchomalacia.12 However, their wheeze symptoms are not solely explained by these overlapping conditions.11
Previously, bronchoscopy was performed to confirm the presence of lower airway pathogens, usually Haemophilus influenzae, Streptococcus pneumoniae or Moraxella catarrhalis.7,8,12,13 In spite of these pathogens being present, PBB rarely evolves into pneumonia, but concern exists that in the long term, if left untreated, bronchiectasis may develop.8 Bronchoscopy is no longer considered necessary, because of its semi-invasive nature, and usually one or two courses (2–6 week) of antibiotics (usually amoxicillin/clavulanic acid), are curative.8,14 Evidence of antibiotic efficacy with symptom dissipation usually occurs within 2 weeks but continuation of antibiotics for a further 4 weeks is thought to be required to allow for airways healing if symptoms have been prolonged.8 Despite initial resolution, later recurrence and need for repeat treatment is required in the majority of patients.15
A diagnosis of PBB is not absolute and many children have wet cough secondary to repeat, intercurrent viral infections. The average duration of symptoms for viral respiratory tract infections is 4 weeks,16 usually with an improving dry cough at the end of the illness. The key distinguishing feature of PBB is usually an absence of waxing and waning coryzal symptoms with improvement to dry cough.
Is it asthma or viral wheeze? Which children outgrow this phenomenon?
The Tucson Children’s Respiratory Study found that that the majority of children who wheezed at a young age were no longer wheezy by the age of 6 years.17 From this age onwards, only 1 in 5 children outgrow their symptoms by the age of 19 years.18 Children who did not outgrow their wheeze tended to have allergies to furry animals, greater severity of symptoms and more persistent symptoms. Whether children who transiently wheeze with viruses should be labelled as asthmatic is still being debated and separating the two groups is not always clear cut.
Our understanding of viruses and wheezing has advanced remarkably in the last 10 years. With the advent of sensitive polymerase chain reaction (PCR) methods, viruses can be detected in 80–90% of children with asthma exacerbations19–23 and two-thirds of those detected are from human rhinovirus (HRV) species,23,24 the viruses usually identified as causing the common cold.25 Outside of exacerbations, viral detection (12–41%) and HRV detection (12–28%) in asthmatics is considerably reduced,26 suggesting a strong correlation between viruses/HRV and asthma exacerbations. In the general paediatric population, HRV accounts for a significant portion of acute respiratory illness (15–48.5%)16,27,28 but not as prominently as in children with asthma. In a US birth cohort of healthy children with parents with atopy, Lee et al29 showed that, on average, children acquire 12.2 HRV infections/child/year and the majority of these children are asymptomatic. These represent de novo infections, as the same type of HRV is never found in the same patient after 4 weeks unless serious immunodeficiency is present.30 Evidence currently suggests that children with asthma have a susceptibility to HRV and have a predisposition to more frequent and severe infections from these viruses.23,31 The frequency of asthma exacerbations coincides with peak periods of HRV, from late autumn to early spring so many children with asthma experience frequent and occasionally continual symptoms throughout the winter months. Whether this situation should be diagnosed as intermittent viral-induced asthma or chronic asthma is unclear. This problem should be resolved in the near future, as many research groups, including our own, are focusing on the exact mechanisms of rhinovirus susceptibility in asthmatic children. This research has the potential to improve diagnostic and therapeutic options. In the interim, the main stay of therapy in asthma has not had any dramatic shifts of late.
For a further detailed discussion about asthma phenotypes and asthma treatment, excellent up-to-date summaries have recently been published in the 2014 National Asthma Council Australia’s Australian Asthma Handbook (see www.asthmahandbook.org.au)
Key points
- Determining the cause of wheeze in young children can be difficult and sometimes is determined only following a trial of treatment.
- Parents’ description of wheeze can be inaccurate and often needs elaboration or confirmation with impersonation or video recordings.
- Asthma is very common but other causes are also common and worth considering in the event of poor efficacy of asthma treatment.
- A diagnosis of PBB should be considered for children with >4 weeks of continuous wet cough.
Competing interests: Peter Le Souëf’s institution has received grants unrelated to this work from NHMRS and Astra Zeneca.
Provenance and peer review: Commissioned, externally peer reviewed.