Breast cancer, the most common cancer in women in Australia,1 has excellent survival rates. Consequently, there is an emphasis on the importance of returning women to health on completion of treatment. However, upper body symptoms such as restriction in range of motion, pain, fatigue, weakness, neuropathy and lymphoedema, as well as general deconditioning, can interfere with quality of life and prevent resumption of pre-diagnosis activities including paid or voluntary work and recreational pursuits.2
Exercise during treatment for breast cancer has been shown to improve quality of life and shoulder function while reducing fatigue and depression.3 Furthermore, exercise has been shown to improve survival, reducing all cause and breast cancer mortality.4 Current guidelines from major cancer bodies, including Cancer Australia, strongly encourage arm-specific and general exercise for women undergoing treatment for breast cancer.5 However, it is unknown if women treated for breast cancer in Australia receive this information in a timely manner and whether it is leading to a reduction in the upper limb morbidity that has historically been associated with treatment for breast cancer.
The aims of this study were to determine if advice was given on arm-specific physical rehabilitation and general exercise after diagnosis of breast cancer and, if so, how, when and by whom it was given. A second aim was to determine the prevalence of physical impairments in Australian women treated for breast cancer.
Methods
A web-based survey was sent to the women of the Review and Survey Group (n = 915) of Breast Cancer Network Australia (BCNA), a national consumer group, in September 2013. The survey was developed and improved through the combined use of expert opinion and focus groups (n = 5). It was tested and retested to ensure acceptability prior to its distribution. Email invitations to complete the survey were sent to the consumer group. A reminder was sent 2 weeks later and the survey closed 4 weeks after the initial invitation.
The respondents’ cancer treatment, the type and timing of physical rehabilitation advice and interventions, and the impairments they faced after diagnosis of breast cancer were reported. To determine whether the sample was representative of the Australian population, demographics of the survey respondents were compared with the general population from the most recent Australian Bureau of Statistics (ABS) reports.
As upper limb morbidity is dependent on the extent of the axillary surgery,6 the group was dichotomised on the basis of whether they underwent a sentinel node biopsy (SNB) or axillary lymph node dissection (ALND). The frequencies of responses were tabulated. For between-group comparisons independent t-tests were conducted for continuous data and Pearson chi-square tests for categorical data. Data were analysed using SPSS for Windows (version 20, IBM, Chicago, USA). Statistical significance was set at P <0.05.
Ethical approval was received from the Human Ethics Research Committee of the University of Sydney.
Results
Population characteristics
Three hundred and eighty seven women (42%) completed the survey, 86% having undergone treatment for breast cancer in the previous 1–5 years. Compared with the Australian population, our group was well aligned for both rural/urban divide and state representation, but was more educated, 48% having completed tertiary education, compared with 26% of the general population.7 Furthermore, 80% of our group held private health insurance, compared with 45% in the general Australian population.8 While 10% reported a history of shoulder symptoms previous to their diagnosis of breast cancer, this is lower than what has been reported in the general population of older Australian women.9 The ALND group was significantly younger (P = 0.01) and more likely to have had more extensive breast surgery (P <0.01) and undergone radiotherapy (P = 0.01) than the SNB group (Table 1).
Table 1. Participant characteristics
|
|
|
SNB (n = 201)
|
ALND (n = 186)
|
|---|
|
Age*
|
56 (9)
range: 35–82
|
54 (10)‡
range: 27–74
|
|
Time since diagnosis†
|
|
<12 months
|
25 (12%)
|
15 (8%)
|
|
1–5 years
|
171 (85%)
|
163 (88%)
|
|
5–10 years
|
5 (3%)
|
5 (3%)
|
|
>10 years
|
0
|
3 (2%)
|
|
Affected side: dominant†
|
105 (52%)
|
100 (54%)
|
|
Pre-surgical history of shoulder problems†
|
20 (10%)
|
17 (9%)
|
|
Breast surgery†
|
|
WLE
|
103 (51%)
|
55 (30%)
|
|
Mastectomy
|
98 (49%)
|
131 (70%)‡
|
|
Radiotherapy
|
115 (57%)
|
129 (69%)‡
|
|
Aromatase inhibitor
|
89 (44%)
|
100 (54%)
|
|
Patient and hospital type†
|
|
|
|
Public patient and hospital
|
47 (23%)
|
46 (25%)
|
|
Private patient/public hospital
|
9 (4.5%)
|
13 (7%)
|
|
Private patient and hospital
|
145 (72%)
|
127 (68%)
|
|
Hospital location and oncology ward availability†
|
|
City with oncology
|
102 (51%)
|
80 (43%)
|
|
City without oncology
|
47 (23%)
|
43 (23%)
|
|
Regional with oncology
|
19 (10%)
|
26 (14%)
|
|
Regional without oncology
|
33 (16%)
|
37 (20%)
|
|
*Mean (SD); †n (%); ‡Significant difference between group (P <0.05)
WLE, wide local excision; SNB, sentinel lymph node biopsy; ALND, axillary lymph node dissection
|
Physical rehabilitation
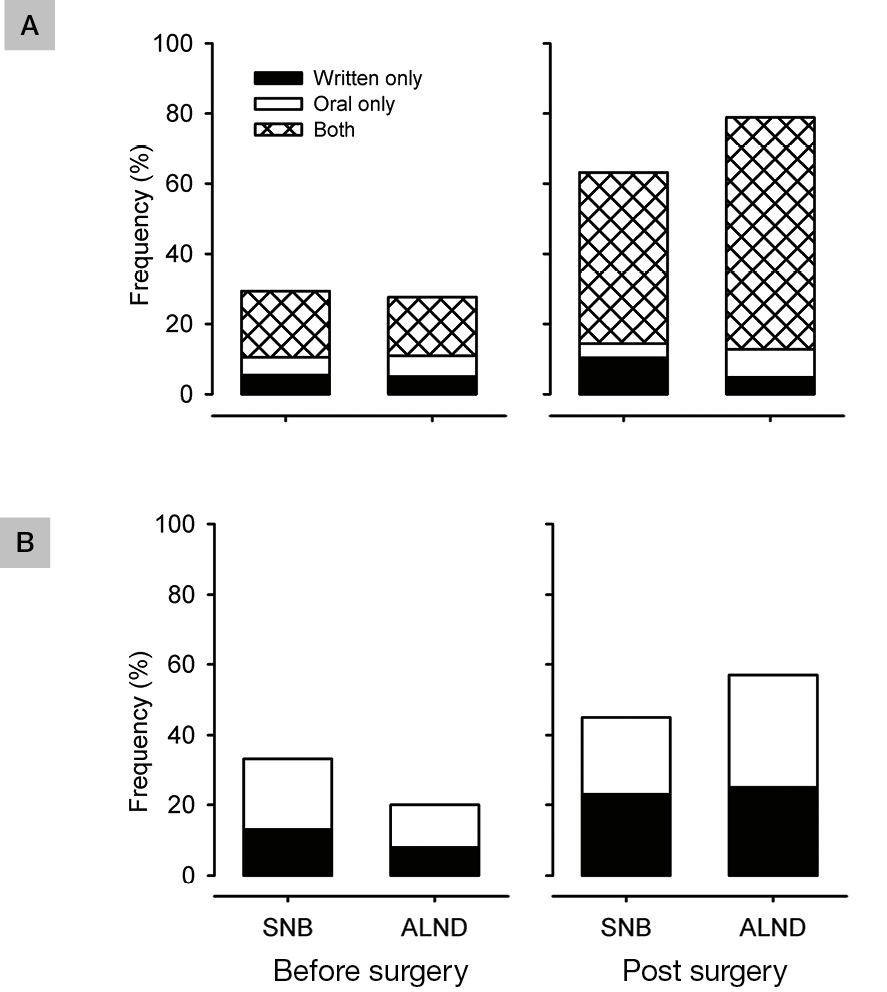 |
Figure 1. Advice received regarding physicial rehabilitation
A. Arm-specific exercises
B. General exercise |
Prior to surgery, overall, 30% reported receiving information regarding arm-specific rehabilitation and 22% reported receiving information regarding general exercise (Figure 1). Arm-specific information was commonly provided by multiple sources (34%). Breast cancer nurses or surgeons were most likely to provide this information (28%), followed by physiotherapists (10%). The women who received general exercise information often received it from multiple sources (49%). Again, breast cancer nurses or surgeons were most likely to provide the information (25%).
In the month after surgery, overall, 75% and 44% reported receiving information on arm-specific and general exercises, respectively (Figure 1). Overall, 82% of respondents received information on arm-specific exercises and 50% received information on general exercise at some point around the time of surgery. Arm-specific exercises were provided by multiple sources for 42% of respondents and physiotherapists were the most common source (48%). Those who underwent ALND were more likely to receive information on arm-specific exercise than those who underwent SNB (ⅹ2 = 8.778; P = 0.003). Of those who received arm-specific exercises, 71% commenced their exercises within 2 weeks of completing surgery; however, 12% did not complete the exercises at all. The primary reason reported for not completing exercises was that they did not feel they had any shoulder problems that warranted completing the exercises (n = 16, 33%). Of those who reported completing exercises, 76% felt confident about which exercises to perform and 62% felt confident about when to progress their exercises.
In addition to surgery, treatments for breast cancer that are associated with chronic physical impairments are radiotherapy and aromatase inhibitors.10 Despite 74% of participants reporting that their arm movement had not returned to pre-surgical range before commencing radiotherapy, only 14% reported receiving advice about arm exercises at the commencement of radiotherapy; 28% perceived they now suffered from arm problems due to radiotherapy. Eighty-three per cent of those on an aromatase inhibitor (n = 157) reported suffering from joint pain, but only 6% of those with pain were referred to rehabilitation. Finally, 37% of those prescribed an aromatase inhibitor received information regarding the possible benefits of exercise to prevent bone loss, a known side effect from these medications.11
Upper-limb and breast morbidity
Arm, hand and shoulder problems were common in the first year after surgery regardless of the type of axillary surgery. All symptoms were significantly more common and of greater intensity in the ALND group (P <0.01; Figure 2). Of those who were 1–5 years post-surgery (n = 334; 86%), 55% reported currently experiencing upper limb problems as a result of their breast cancer treatment (Figure 3), and 44% reported ongoing pain and/or swelling in the breast, chest or trunk region. Women who underwent a mastectomy more commonly reported chest or breast swelling (ⅹ2 = 5.13, P = 0.02), but not pain (ⅹ2= 0.10; P = 0.75), compared with those who underwent a wide local excision.
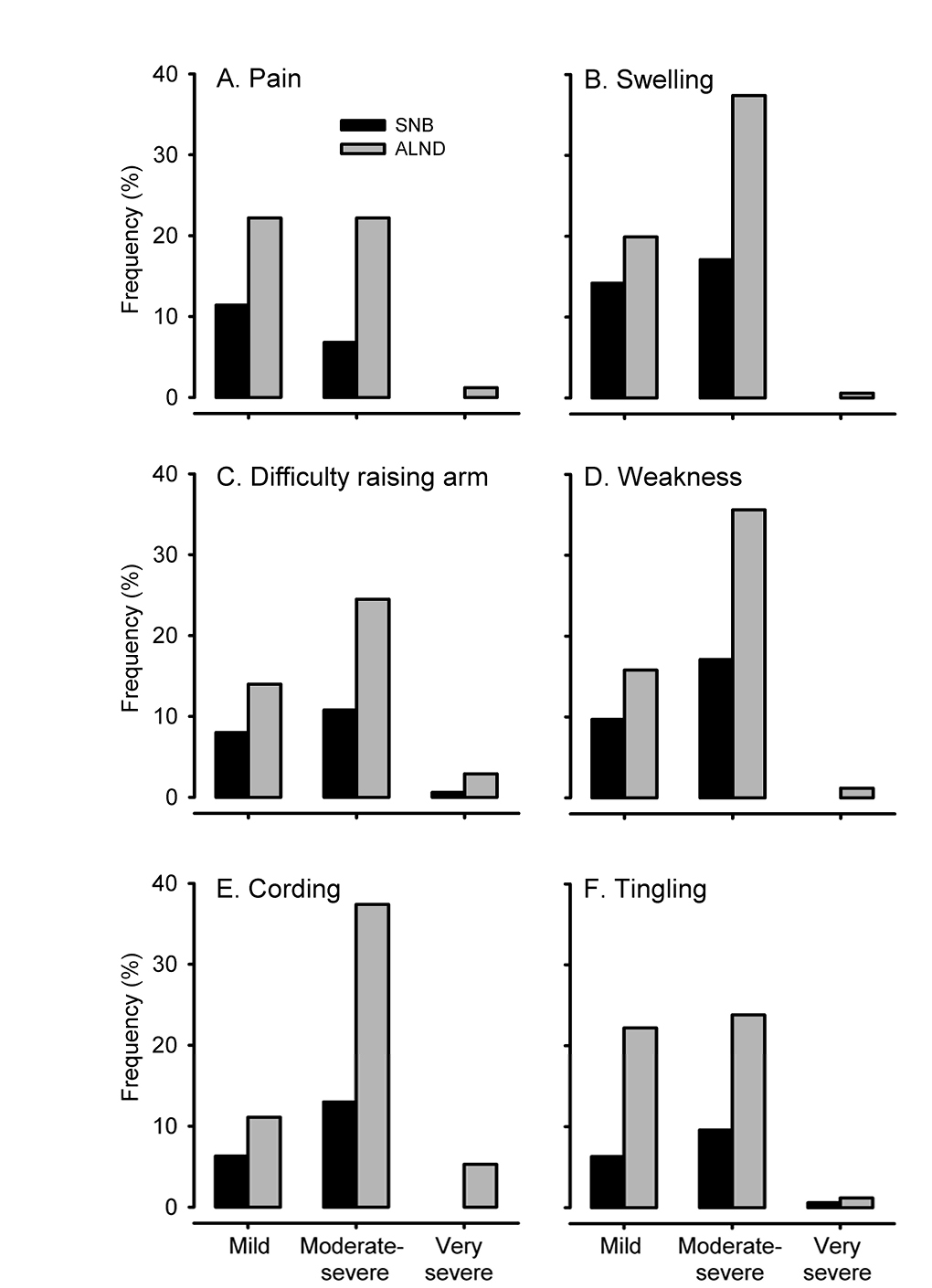 |
Figure 2. Frequency and severity of upper limb symptoms experienced in the first year for women who
underwent SNB (n=201) and ALND (n=186). |
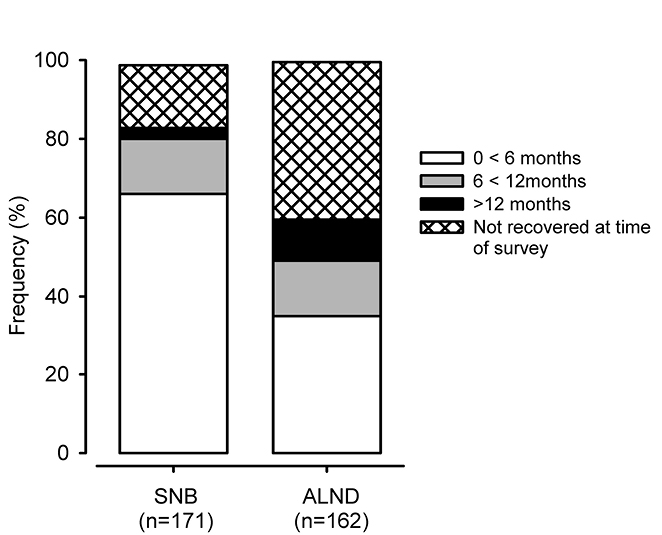 |
| Figure 3. Time for self-reported upper limb recovery from treatments for breast cancer to pre-surgery state in women treated 1–5 years previously |
Discussion
This national study shows that current physical rehabilitation management strategies offered to women treated for breast cancer in Australia do not prevent upper limb morbidity in the first year following surgery, regardless of whether women had undergone SNB or ALND. For many women, these symptoms had not resolved by 1 year after diagnosis of breast cancer, which is consistent with previous national and international findings.12–14 In addition, women experienced chest/breast pain and swelling as a consequence of their treatments in the first year, which for many had also not resolved.
As the majority of women had received information on exercises for the upper limb, the number of women reporting moderate-to-very-severe symptoms in the first year following surgery was disappointing. A number of factors may contribute to these ongoing impairments. First, clinicians may be using outdated information and guidelines to inform their clinical practice.15–17 Historically, women were cautioned against using their arm on the side of surgery because of the belief that it increased the risk of lymphoedema.18,19 Evidence from systematic and narrative reviews15,20 has discredited this belief.
A second factor may be related to ongoing monitoring of symptoms, particularly in the first year after diagnosis of breast cancer. In the current study, very few women received upper limb exercises or referral to a rehabilitation specialist at the onset of radiotherapy even though most had not recovered their upper limb function and radiotherapy is a major risk factor for pain.10 The effects of a lack of monitoring for new or ongoing symptoms are possibly compounded by two additional factors: women not reporting symptoms until they have progressed21 and the responsiveness of clinicians to symptoms.22,23 Evidence for the benefits of monitoring and intervening at the presentation of mild symptoms has been found for various arm problems experienced after breast cancer treatment, including shoulder range of motion,24 pain25 and lymphoedema.26
Responsiveness to symptoms may be conditional on availability of persons with expertise. Breast cancer nurses and surgeons were reported as the most frequent sources of information and, certainly, they are well positioned to provide the initial advice regarding the importance of exercises. However, management of impairments such as pain, cording, shoulder stiffness, muscle weakness and swelling, particularly in the acute period, may require more specialised knowledge. Lack of appropriate referral for timely treatment may contribute to long-term impairments.
More than half of the respondents reported seeking care outside their treating hospital and frequently paid for these services out of their own pockets. The current findings are based on the reports of women in the BCNA Survey and Review group, who have higher levels of education and are more likely to have private health insurance than the general Australian community27 and, therefore, may have a higher level of understanding of the effects of treatment from breast cancer. While the private healthcare system may afford greater access to a multidisciplinary team for management of physical impairments, it is clear that it was not sufficient to improve outcomes in this group. The reasons for this remain unknown. Regardless, the concern with our findings is that they may underestimate the level and frequency of impairments arising from treatment of women with breast cancer in the wider general population who may have fewer resources and lower levels of education than our sample.
From this survey, it is clear that the current processes of rehabilitation after treatment for breast cancer in Australia are insufficient to reduce the physical impairments arising from treatment of breast cancer. Some issues need to be addressed within the oncology setting, such as ensuring the information provided is based on current evidence. In addition, alternative prevention and intervention models of care, including self-management and e-health, need to be explored to accommodate Australian health systems and financial and geographical constraints.16 Even if alternative models are available, general practitioners (GPs) have an important role in ensuring that the patient understands these symptoms are important and can be addressed, reinforcing/supplementing the exercise advice, monitoring for early identification of physical impairments and referring women on, when warranted. The increasing focus on development of shared-care models in the oncology field, further highlights the importance of the role of general practice.28
Implications for general practice
- Chronic physical impairments are common, secondary to treatment for breast cancer.
- GPs are well placed to assist in detecting and referring patients to rehabilitation specialists, such as physiotherapists, for interventions.
Competing interests: None.
Provenance and peer review: Not commissioned, externally peer reviewed.