Case study
A man, aged 32 years, presented one month after undergoing cryotherapy with liquid nitrogen for an apparently common wart on his hand. A progressively enlarging painful lump that bled easily had first appeared at the site of treatment 10 days post-cryotherapy.
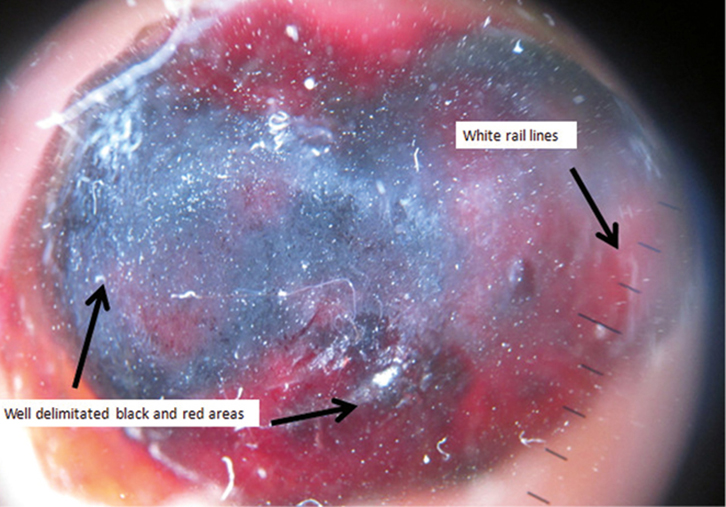
On examination, there was a vascular nodule, 2 cm in diameter, on the palmar surface of the middle phalanx of his right-hand third finger (Figure 1). Polarised, non-contact dermoscopy revealed a well-delineated lesion, with black and red areas plus white rail lines (Figure 2).
 |
 |
| Figure 1. Vascular tumour on the palmar surface of the middle phalanx of the third finger of the right hand. |
Figure 2. Well-delineated black and red areas with white rail lines consistent with pyogenic granuloma |
Question 1
What are the differential diagnoses?
Question 2
What is the most likely diagnosis?
Question 3
Is dermoscopy helpful for a better diagnosis of this condition?
Question 4
What are the treatment options for this disease?
Answer 1
The clinical differential diagnoses include:
- pyogenic granuloma
- bacillary angiomatosis
- Kaposi´s sarcoma (especially in patients with acquired immunodeficiency syndrome [AIDS] or those who are immunosuppressed)
- non-melanoma skin cancer (eg basal cell carcinoma, squamous cell carcinoma and keratoacanthoma)
- benign cutaneous tumours (eg seborrhoeic keratosis, true haemangioma, common warts)
- malignancies (eg amelanotic melanoma, metastatic carcinoma).
Answer 2
Pyogenic granuloma (PG) is a rapidly growing, benign acquired vascular proliferation that commonly affects the fingers, hands, forearms and face. It is also called a lobular capillary haemangioma because of its histological features.1 There is often a history of preceding trauma to the area. There is no evidence to implicate any infectious agent, but angiogenic and hormonal factors have been implicated. The expression of a new form of oestrogen receptor (ER-b) has been reported in a wide variety of vascular tumours including haemangiomas.2
Answer 3
Dermoscopy is a useful tool to diagnose pyogenic granulomas. Although seven different patterns are described, none are 100% specific.3 The three main structures that can be distinguished are:
- a reddish homogeneous area, with high sensitivity and low specificity (also found in 89% of amelanotic melanomas)
- ‘white collarete’ (specificity 90.7%)
- white rail lines (specificity 81.4%).
In cases in which these three structures are observed in combination, the specificity to diagnose pyogenic granuloma rises to almost 100%.
Haemorrhagic crusts and ulceration are also present in 46% of cases. However, new patterns have been described since the report of Zaballos et al.3 The presence of a central, irregular, whitish-yellow amorphous structure with a peripheral crown of polimorphous atypical vessels has also been described.4 Nevertheless, obtaining a small sample for pathological confirmation is mandatory in adults to rule out amelanotic melanoma.5
Answer 4
Current therapeutic modalities include surgical and non-surgical management.6 Surgical excision and primary closure offers a low rate of recurrence6 plus a complete sample for histological examination. Another reasonable option is curettage/shave excision with cautery, which has high cure rates and potentially better cosmetic results. Non-surgical management includes cryotherapy, laser therapy, sclerotherapy, topical timolol and topical imiquimod.7
Cryotherapy with liquid nitrogen (1–2 mm rim of normal tissue with two freeze–thaw cycles is widely recommended), CO2 laser and dye laser flashlamp also offer a low rate of recurrence. However, cryotherapy may cause heavy bleeding requiring careful haemostasis. Complete resolution of the lesion may require several treatment sessions. The choice of these treatment methods depends on the expertise of the clinician, but has the important disadvantage of no sample for histological processing unless combined with a biopsy.
Laser therapy (585 nm and 595 nm) is safe and effective, best for small pyogenic granulomas (<5 mm in diameter) and in children. Sclerotherapy using sodium tetradecyl sulphate, monoethanolamine oleate, and absolute ethanol injection have been also performed with variable success.6
Timolol gel or ophthalmic solution (0.5%) has been used to treat infantile haemangiomas on the face and periocular region by vasoconstriction of the vessels feeding the tumour and also by suppressing vascular endothelial growth factor (VEGF). Only two cases have been described in the literature at the present time with good response.7
Imiquimod 5% cream is a synthetic imidazoquinolin heterocyclic amine that enhances, through cytokine induction, both the innate and acquired immune pathways, resulting in immunomodulating, antiviral and antitumour effects. The inflammatory response that occurs can be a limiting factor for use in children. The treatment regime for topical imiquimod 5% cream should be varied in frequency of application and duration according to clinical response. Isolated cases and small case series with no more than 10 patients have been published, with successful results in all cases.8
Case continued
The history and examination findings were consistent with a pyogenic granuloma. Surgical removal of the lesion by excision, curettage and electrocautery was performed, and histological study confirmed the diagnosis. After six months of follow-up, no recurrence was observed.
Authors
Pablo Fernandez-Crehuet PhD, MD, Consultant, Department of Dermatology, Hospital Alto Guadalquivir, Andújar, Jaén, Spain. pablocre-huet@hotmail.com
Ricardo Ruiz-Villaverde MD, PhD, Consult-ant, Department of Dermatology, Hospital Virgen de las Nieves, Granada, Spain.
Competing interests: None.
Provenance and peer review: Not commissioned, externally peer reviewed.