Haematospermia refers to the presence of blood in the ejaculate. The epidemiology of haematospermia is poorly described because the majority of men do not witness their semen.1 For men who experience haematospermia, it can provoke significant anxiety. While most cases of haematospermia are benign, it may be secondary to a sinister underlying pathology and require systematic evaluation by the general practitioner (GP).2 A number of patients may require further evaluation by a urologist or other specialist, although even among high-risk populations, malignancy is rare.3
Anatomy
Several anatomical structures contribute to the ejaculate and any one of these may be the source of the haematospermia. Sperm production begins in the testes and sperm then travel via the epididymis, vas deferens and ejaculatory duct. Fluid from the seminal vesicles, prostate and Cowper’s glands then mixes with sperm to form the ejaculate. Finally, the ejaculate leaves via the urethra. For haematospermia to occur, the patient must have an intact ejaculation function.4
Aetiology
There is a broad differential for haematospermia (Box 1).5 Historically, the precise cause of haematospermia was often not established and therefore termed idiopathic. Recently, iatrogenic and infectious aetiologies have been reported as the most common causes of haematospermia.6 The main aim of assessment is to avoid missing malignancy, particularly prostate cancer. Testicular, bladder and urethral cancer very rarely cause haematospermia, and only if advanced.2
Box 1. Aetiology of haematospermia
|
|
Infection (in the form of prostatitis, urethritis, epididymo-orchitis):
- Bacterial – chlamydia, gonorrhoea, enterococcus, tuberculosis
- Viral – human immunodeficiency virus (HIV), cytomegalovirus (CMV), herpes simplex virus (HSV)
- Other – schistosomiasis
Iatrogenic
- Post-transrectal ultrasound (TRUS) biopsy
- Prostate radiotherapy or brachytherapy
- Post-vasectomy
- Post-orchidectomy
Malignancy
- Prostate
- Bladder
- Testicular
- Urethral
Trauma
- Coital trauma
- Perineal trauma
Prolonged abstinence
Obstruction
- Ductal obstruction
- Cysts of seminal vesicles/Wolffian duct/utricle
- Calculi of seminal vesicles, ejaculatory duct, prostate, urethra
Systemic disorders
- Hypertension
- Chronic liver disease
- Lymphoma
- Leukaemia
- Amyloidosis
- Bleeding disorders
Idiopathic
|
Approach
A focused history and examination is the initial step in the evaluation of haematospermia. It is important to differentiate between haematospermia and pseudo-haematospermia. The latter is haematuria or blood originating from the patient’s partner. If both haematuria and haematospermia are present, the approach should be as per the haematuria pathway (including urine cytology, computed tomography [CT] intravenous pyelogram and cystoscopy).7
Assess for the presence of the red flags of haematospermia, in particular:8
- patient’s age (>40 years)
- recurrent or persistent haematospermia
- prostate cancer risk factors (eg positive family history or African heritage)
- constitutional symptoms (eg weight loss, anorexia, bone pain).
It is also important to keep in mind the common aetiologies of haematospermia (are there symptoms of urinary tract infection or sexually transmissible infection [STI]?). Pain on ejaculation is highly suggestive of prostatitis or ejaculatory tract obstruction (very rare).5 Haematospermia may be simply explained by having had a recent urological procedure. Other causes include prolonged sexual intercourse/masturbation or, alternatively, a period of prolonged abstinence. GPs should enquire about a history of tuberculosis or schistosomiasis, the use of anticoagulants, or the presence of a bleeding disorder.1
Key features on examination include blood pressure (for severe hypertension) and temperature (for evidence of infection-related fever).9 A genital examination of the penis and urethral meatus, testes, epididymis and spermatic cord should be performed for the presence of masses, tenderness or superficial lesions.6
A digital rectal examination (DRE) should be conducted to palpate for prostate carcinoma (asymmetrical, hard nodules, non-tender) or prostatitis (intensely tender prostate). Finally, a systems review should be carried out for features of chronic liver disease, lymphoma or leukaemia. If there remains any doubt about whether the patient has true haematospermia or pseudo-haematospermia, ask the patient to collect sperm into a condom.1
Investigations
Certain investigations should be conducted in all patients with haematospermia, whereas others should be reserved for those with high-risk features.10,11 All patients should undergo urine microscopy, culture and sensitivity (MCS) for the presence of infection and red blood cells, urine cytology for evidence of bladder malignancy, and a full blood count and coagulation studies for coagulopathy. After clinical assessment, if an STI is suspected, urine nucleic acid amplification test for chlamydia and gonorrhoea should be performed, ideally with a first-pass urine specimen. A prostate-specific antigen (PSA) assay should be performed in men >40 years of age or if DRE is abnormal or significant prostate cancer risk factors are present. If tuberculosis or schistosomiasis is the suspected cause of haematospermia, perform urine and semen acid-fast bacilli and parasites.6
Guidelines for urology referral
The GP should consider each patient with haematospermia individually. Common indications for referral to a urologist are listed in Box 2.7,12
On review by the urologist, the patient may undergo further investigations such as:1
- transrectal ultrasound (TRUS) for prostate or seminal vesicle abnormalities
- scrotal ultrasound to assess for testicular abnormalities
- magnetic resonance imaging (MRI) or CT for fine pelvic anatomy detail
- cystoscopy for bladder and urethral pathology.
Box 2. Indications for urology referral
|
- Men ≥40 years of age
- Persistent or recurrent haematospermia
- Suspicious DRE findings
- Abnormal PSA results
- Suspicion of prostate, bladder, testicular or urethral malignancy on history, examination or investigations
- Concurrent haematuria
- Haematospermia despite treatment for suspected cause
|
Management
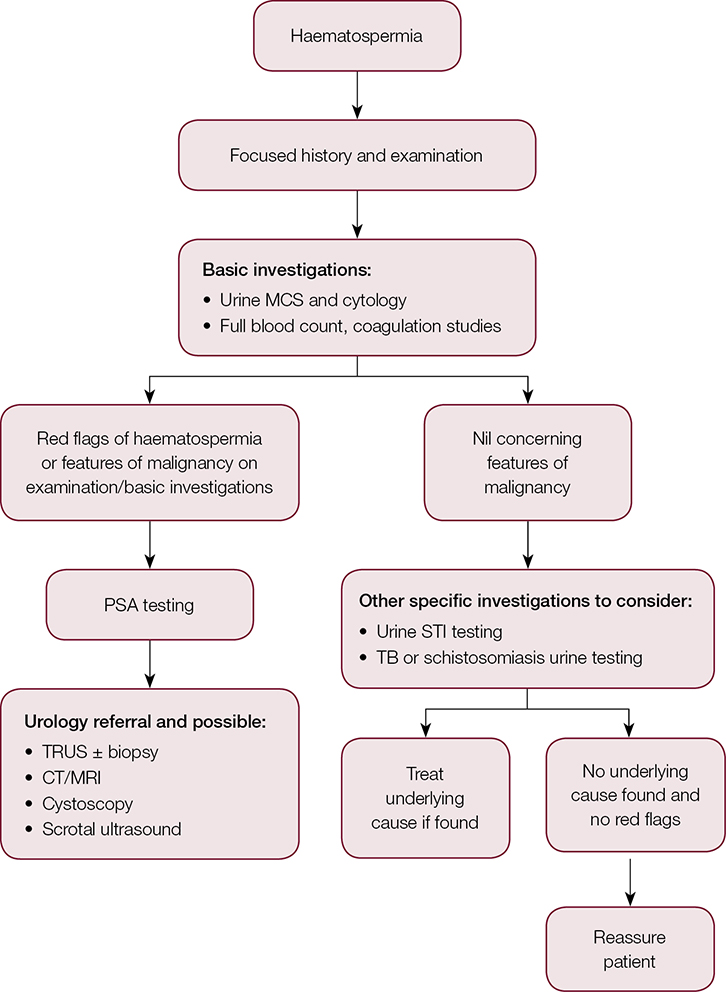 |
Figure 1. Haematospermia approach and management summary
CT, computed tomography; MCS, microscopy, culture, sensitivity; MRI, magnetic resonance imaging; TB, tuberculosis; TRUS, transrectal ultrasound. |
The management of haematospermia will depend on the underlying cause. If none is found, and the haematospermia is an isolated event, reassurance is all that is required (Figure 1).6 In an anxious patient, this can be challenging. Questions regarding the effects of haematospermia on male fertility and the risks of cancer are common. Most causes of haematospermia will have no effect on fertility;6 however, some rare pathology such as testicular malignancy may diminish reproductive capacity. It is also important to note that the vast majority of men with haematospermia who have been reviewed and investigated by a urologist do not have an underlying malignancy.2
If an infection is suspected or proven, appropriate antimicrobials should be initiated. For empirical treatment of STIs, we recommend intramuscular ceftriaxone and oral azithromycin.13 For mild-to-moderate prostatitis or epididymo-orchitis related to a urinary tract infection, we recommend trimethoprim or amoxycillin with clavulanic acid, both of which have good prostate penetration.14 If an unusual infection is found (eg tuberculosis or schistosomiasis), referral to an infectious diseases clinic is appropriate.
Patients with iatrogenic haematospermia should have been counselled pre-procedure about the risk of haematospermia. Post-prostate biopsy haematospermia usually takes
20 ejaculations to resolve.7 If malignancy is identified, the treating urologist will arrange further investigations and treatment.
For ductal obstruction and cystic abnormalities of the accessory glands, the treating urologist may perform interventions such as cystic aspiration or deroofing, or endoscopic removal of calculi.3 In the rare event of a systemic cause for haematospermia, appropriate speciality referral will have to be made.
Finally, if the patient is troubled by persistent haematospermia without an identified cause after a diagnostic work-up by both the GP and urologist, one option would be to start a 5-alpha reductase inhibitor such as finasteride or dutasteride. This reduces vascular endothelial growth factor (VEGF) expression and sub-urethral vessel microdensity. It is particularly useful in elderly patients with benign prostatic bleeding; however, patients should be warned that it may take six months before the haematospermia improves.15 For younger men with persistent idiopathic haematospermia, it is reasonable to consider treatment with one month of doxycycline.
Key points
- Haematospermia is an anxiety-provoking symptom in men that may be encountered by the GP.
- While most haematospermia is benign and self-limiting, it may occasionally be due to an underlying malignancy (such as prostate cancer) and hence warrants a systematic evaluation.
- Red flags of haematospermia identified on clinical assessment and basic investigations help distinguish between harmless haematospermia and that which will need specialist referral. These include patient’s age (≥40 years), recurrent or persistent haematospermia, prostate cancer risk factors (eg positive family history or African heritage), or constitutional symptoms such as weight loss, anorexia, bone pain.
- Management of haematospermia will depend on the underlying cause. If none is found and the haematospermia is an isolated event, reassurance is all that is required.
Author
Nandu Dantanarayana MBBS (Hons), MS, Department of Surgery, St Vincent’s Hospital, Darlinghurst, NSW. nandu.dantan@gmail.com
Competing interests: None.
Provenance and peer review: Not commissioned, externally peer reviewed.