Sleepwalking is characterised by:
- partial arousal during non-rapid eye movement (NREM) sleep, typically during the first third of the night
- dream content that may or may not be recalled
- dream-congruent motor behaviour that may be simple or complex
- impaired perception of the environment
- impaired judgement, planning and problem-solving.
Memory of episodes varies between episodes and between those who sleepwalk, ranging from complete amnesia to complete recall of the episode.1 Analgesia has been noted and those who sleepwalk are often unaware of being injured until they awaken.2,3 This paper provides a review of the most recent science on sleepwalking, to guide clinical decision-making.
A recent meta-analysis showed the estimated lifetime prevalence of sleepwalking is 6.9% (95% confidence interval [CI]: 4.6, 10.3).4 There was no significant difference in lifetime reports of sleepwalking between children and adults, suggesting that initial onset of sleepwalking in adults is rare and requires further investigation. The current prevalence rate of sleepwalking, within the past 12 months, was significantly higher in children 5.0% (95% CI: 3.8, 6.5) than in adults 1.5% (95% CI: 1.0, 2.3).4 This may be the result of less slow wave sleep during adulthood and, hence, fewer opportunities for sleepwalking, less observed sleepwalking or maturational changes.
There is some evidence for a genetic predisposition for sleepwalking in some people, although this is not well understood. Monozygotic twins have been found to be more concordant for sleepwalking than dizygotic twins.5,6 One study found more Caucasians who sleepwalk (35.0%) than non-sleepwalkers (13.3%) were DQB1*0501-positive, which is suggestive of the DQB1 genes being implicated in motor disorders in sleep.7 A study of a single family across four generations suggested that sleepwalking may be transmitted as an autosomal dominant trait with reduced penetrance.8
Associated problems
Sleepwalking has been associated with other sleep problems such as confusional arousals or awakenings, rhythmic movement problems, sleep disordered breathing, night terrors, sleep talking and bruxism.9–11 It has also been associated with daytime tiredness, and behavioural and emotional problems in children.12–14 However, comorbid sleep disorders, rather than sleepwalking per se, have been found to account for these daytime problems.11 It is essential, therefore, that presentations of sleepwalking with daytime tiredness and/or behavioural and emotional problems, particularly in children, include an assessment of other sleep disorders.
Assessment
Although our knowledge of sleepwalking is still in its infancy, Figure 1 provides guidelines on the assessment and treatment of sleepwalking in clinical practice based on what is currently known and least likely to cause adverse effects. Polysomnography is the only infallible measure of sleepwalking, if it occurs. However, it is costly and inconvenient, and there are difficulties in capturing infrequent and irregular behaviour, such as sleepwalking. It is therefore not recommended for routine assessment of sleepwalking. A history using self-report and reports from others of sleepwalking behaviour are sufficient in most cases. Polysomnography may be useful for forensic cases or when there is uncertainty about the differential diagnosis.
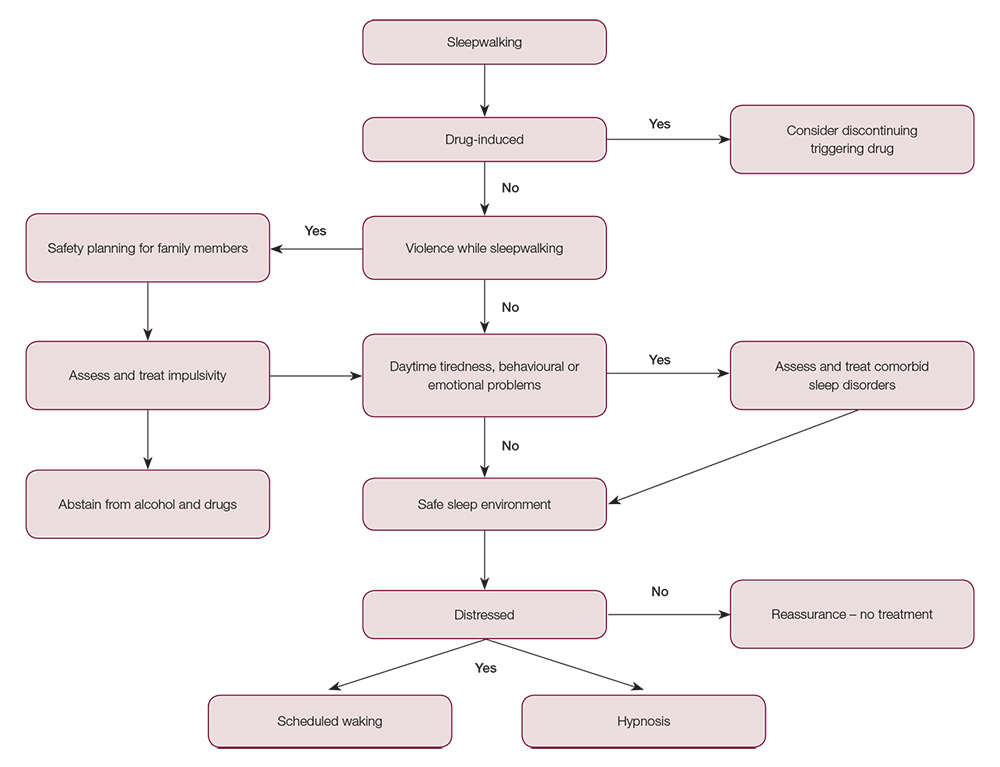
Figure 1. Flowchart for the assessment and treatment of sleepwalking
Case studies have identified a number of classes of medications that may trigger sleepwalking, including antibiotics, anticonvulsants, atypical antidepressants, typical and atypical antipsychotics, benzodiazepines, lithium, non‑benzodiazepine hypnotics, noradrenergic and specific serotonergic antidepressants, noradrenaline re-uptake inhibitors, quinine, selective and non‑selective beta blockers, selective serotonin re-uptake inhibitors (SSRIs), and tricyclic antidepressants.15 These have only been described in patients without a previous history of sleepwalking, so their effect on sleepwalkers is not known. If sleepwalking is triggered by a prescribed medication, discontinuation should be considered.
Violence during sleepwalking
Patients who sleepwalk do not seek out other people while sleepwalking, but may inadvertently encounter them.16 They can be led back to bed and do not need to be awakened. As the most common emotion experienced during sleepwalking is fear, triggering a fight/flight response, a very small proportion of people who sleepwalk are sometimes violent towards others. Reports in the literature are limited to violence by men, typically younger men. It is hypothesised that those who sleepwalk and are violent have impulsive tendencies that are exacerbated in sleepwalking because of the emotional arousal and impaired frontal cortical function during sleep that would ordinarily inhibit impulsive aggression.17 It is imperative that priority be given to ensure the safety of other family members. It is hypothesised that treatments for impulsive aggression may reduce the tendency for violence during sleepwalking.17 However, it is also important that people at risk of violence during sleepwalking abstain from alcohol and drugs, which are known to exacerbate impulsivity.17
Interventions
Sleepwalking generally does not cause any problems for the sleepwalker, but can result in injury (eg falling from a high point18 or walking through glass doors or windows19) or may simply cause significant embarrassment, such as being found naked wandering down the street.20 Locking windows and external doors and removing breakable objects is recommended. It is important not to lock sleepwalkers in their rooms, particularly children, as this poses a safety risk in case of fire.
There have been no clinical trials to assess the efficacy of any treatments for sleepwalking, despite more than 100 years of case reports of psychological, pharmacological and other interventions.21 If sleepwalking is causing distress to the sleepwalker or their family members, or the sleepwalker is limiting their activities (eg not going on school camps or travelling), psychological interventions – scheduled waking or hypnosis – hold the greatest potential with the least likelihood of adverse effects.21
Scheduled waking involves waking the sleepwalker briefly 15–30 minutes before they would normally sleepwalk. Hypnosis that provides the hypnotic suggestion that sleepwalker will wake if their feet touch the ground is based on a similar premise of disrupting the sleepwalking process. A recorded hypnosis session can be implemented independently by the patient. Both interventions should be done daily for about two to three weeks. Although sleep hygiene is routinely recommended for treating sleepwalking, there have been no empirical studies evaluating its effectiveness – it is therefore not a recommended intervention for sleepwalking at this stage.
Conclusion
Sleepwalking is a relatively common and innocuous arousal disorder during NREM sleep. Most people who sleepwalk do not require treatment, but comorbid sleep disorders that result in daytime tiredness, and behaviour and emotional problems require intervention. In the absence of clinical trials, tentative, low-risk treatments are suggested for sleepwalking that results in personal distress or violence towards others.
Case
Lily, aged 8 years, presented to her general practitioner following a four-year history of sleepwalking, on average, twice a week. She had not sustained any injuries while sleepwalking, but her parents were concerned about the potential for injury in unfamiliar environments, for example, if she attended a school camp or sleepovers. Lily’s father also has a history of sleepwalking. Lily had no evidence of comorbid sleep or daytime problems. In addition to psychoeducation about safe sleep environments, treatment involved teaching Lily’s parents to do scheduled waking – briefly waking Lily nightly for three weeks, 20 minutes before she usually sleepwalked. No sleepwalking episodes were observed in the two weeks prior to the one-month review.
Author
Helen M Stallman PhD, DClinPsych, CertMedEd, Senior Lecturer, Psychology, Centre for Sleep Research, School of Psychology, Social Work and Social Policy, University of South Australia, Adelaide, South Australia. helen.stallman@unisa.edu.au
Competing interests: None.
Provenance and peer review: Not commissioned, externally peer reviewed